A Systematic Evaluation of Incidence and Influencing Factors of Falls in Adult Cancer Patients
-
摘要:
目的 系统评价成人肿瘤患者跌倒发生率及影响因素,为早期识别和预防跌倒发生提供证据支持。 方法 计算机检索PubMed、中国知网等8个英文和中文数据库,检索时间为数据库建立至2024年1月,纳入以成人肿瘤患者跌倒发生率和(或)影响因素为结局的横断面研究、队列研究和病例对照研究。由2名研究者独立筛选文献、文献质量评价、提取数据后,使用RevMan 5.4进行Meta分析。 结果 共计纳入19篇文献,样本量总计 70508 例。结果显示,成人肿瘤患者跌倒的合并发生率为23.0%(95%CI 0.23,0.24)。年龄、女性、低文化程度、跌倒史、跌倒恐惧、肿瘤中晚期、肿瘤种类(乳腺癌、生殖系统肿瘤、前列腺癌)、共病、化疗、放疗、多重用药(n 5)、药物( 抗抑郁药、抗精神病药、镇静催眠药)、相关症状(发热、周围神经病变、疲乏、抑郁)、营养不良、低体重、认知功能障碍、平衡障碍、步态异常、低日常生活能力是成人肿瘤患者跌倒的影响因素。结论 肿瘤专业医护人员应早期识别跌倒发生的影响因素并采取针对性措施来减少跌倒发生。 Abstract:Objective To systematically evaluate the incidence and influencing factors of falls in adult cancer patients, and provide evidence support for early identification and prevention of falls. Methods Eight Chinese and English databases, including PubMed, Embase, CNKI, and Wanfang Database, were searched by computer. The databases were established until January 2024 and included in cross-sectional, cohort, and case-control studies based on the incidence and/or influencing factors of falls in adult cancer patients. Two researchers independently screened and reviewed literature, evaluated literature quality, and extracted data before conducting meta-analysis using RevMan 5.4 software. Results A total of 19 articles were incorporated into the research, with a total sample population size of 70508 cases. The results showed that the incidence of comorbid falls in adult tumor patients was 23.0% (95%CI 0.23, 0.24). Age, female, low education level, fall history, fall fear, middle and late stage of tumor, tumor type (breast cancer, reproductive system tumor, prostate cancer), comorbidity, chemotherapy, radiotherapy, multiple drugs (n ≥ 5), drugs (antidepressants, antipsychotics, sedatives and hypnotics), related symptoms (fever, peripheral neuropathy, fatigue, depression), malnutrition, low weight, cognitive dysfunction, balance disorders, gait abnormalities, and low ability of daily living were the influencing factors for falls of adult tumor patients.Conclusion Cancer professionals should identify the influencing factors of falls early and take targeted measures to reduce the occurrence of falls. -
Key words:
- Tumor /
- Fall /
- Incidence /
- Influencing factors /
- Systematic evaluation
-
随着胰腺外科技术的提高及治疗模式的转变,对胰头良性占位的治疗强调更小创伤和快速康复理念的Beger手术,越来越受到临床重视[1-2]。临沧市人民医院对2014年1月至2020年1月收治的59例慢性胰腺炎、胰头良性及低度恶性肿瘤患者施行手术治疗,其中行改良Beiger手术31例,胰十二指肠切除术(PD)28例,现将治疗体会报告如下。
1. 资料与方法
1.1 一般资料
选取2014年1月至2020年1月临沧市人民医院肝胆外科收治的59例胰头肿块型慢性胰腺炎、胰头良性及低度恶性肿瘤患者作为研究对象,随机分成改良Beger手术组与PD 手术组。59例患者中 54例有不同程度的腹疼表现,5例无明显症状,为体检发现。52例有7~22 a长期酗酒史。术前均B超、CT、MRI等影像检查,以胰头肿块局限性病变为主要表现,未侵犯十二指肠及血管。59例患者均术后病理石蜡切片明确诊断。两组患者平均年龄、性别、疾病谱、酗酒史、并存疾病等情况,差异无统计学意义(P > 0.05),见表1。
表 1 两组一般资料比较($ \bar x \pm s$ )Table 1. Comparison of the general data between two groups ($\bar x \pm s $ )项目 Beger组(n = 31) PD组(n = 28) t/χ2 P 男/女(n) 23/8 21/7 210.06 0.25 年龄(岁) 43.7 ± 3.1 44.2 ± 2.7 0.843 0.20 疾病谱[n(%)] 胰头肿块型慢性胰腺炎 26(83.9) 23(82.1) 202.21 0.11 胰头囊肿合并胰管结石 2(6.5) 1(3.6) 18.34 0.19 胰头实性假乳头状瘤 1(3.2) 1(3.6) 45.54 0.33 导管内乳头状黏液瘤 1(3.2) 1(3.6) 3.19 0.46 胰头浆液性囊腺瘤 1(3.2) 1(3.6) 11.51 0.29 长期酗酒史(n) 27 25 146.04 0.27 并存疾病(n) 2.96 0.31 糖尿病 16 17 高血压病 7 9 冠心病 7 5 1.2 手术方法
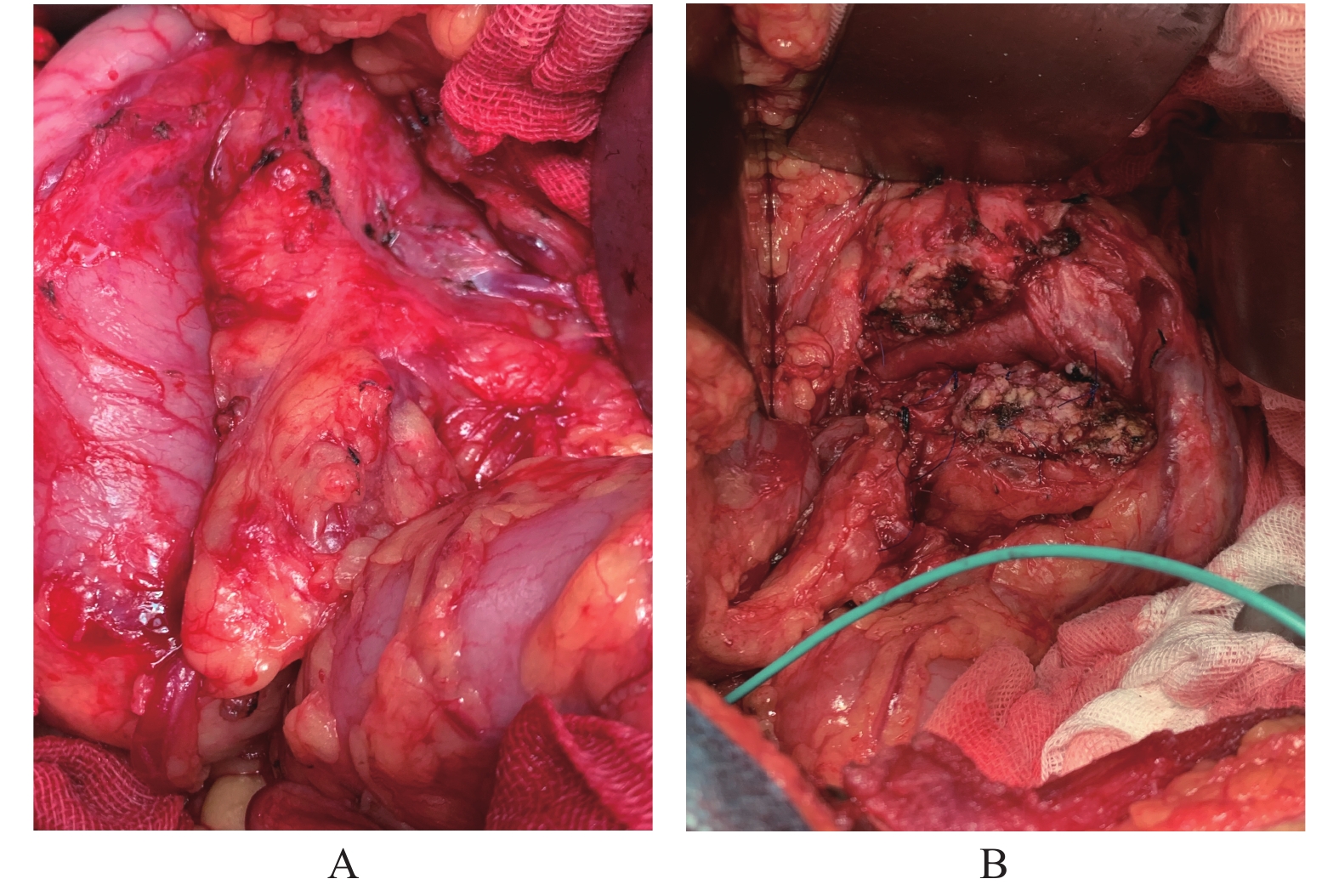
改良Beger手术:取上腹部正中或右侧肋缘下斜切口,切开胃结肠韧带,显露胰头,明确胰头病变区域,排除病变广泛侵袭或致密黏连,判断胰头部病变可整块切除,术中取材冰冻病理检查明确诊断,除外胰头癌等。解剖肝十二指肠韧带,显露门静脉、胃十二指肠动脉,避免胰十二指肠前上动脉损伤,解剖肠系膜上静脉,电凝离断胰颈,显露胰管置静脉穿刺硅胶管标记引流,胰腺断面用4-0 Prolene血管缝合线缝合止血,Allis钳钳夹胰腺断面头侧向右上方向牵引,逐一显露结扎胰腺钩突段肠系膜上静脉及门静脉右壁分支,循肠系膜上动脉切除胰腺钩突,避免损伤胰十二指肠下动脉。用电刀或刀片小心分离胰头,不游离胰后筋膜,距离十二指肠内侧残留 0.5~0.7 cm胰腺组织,弧形切除胰头及病变,保护十二指肠血管弓。经胆囊管置入取石网篮至胰腺段胆管作术中标记,避免胰内胆管损伤(图1)。缝扎胰管及残余胰头组织。胰管空肠黏膜对黏膜端侧吻合重建胰肠通路。胰周置双套管引流,同时术后肠内外营养支持治疗等。
PD手术:围手术期治疗及手术切口同Beger手术,手术方式采用标准的Whipple手术操作流程完成。
1.3 术后随访
通过电话、门诊复诊的方式了解术后患者疼痛程度、镇痛药物使用频率、术后糖尿病、脂肪泻、肿瘤复发以及生活质量改善等情况。疼痛情况采用疼痛积分表评价,胰瘘分级按2016版国际胰瘘研究小组的诊断和分级标准,胆漏以穿刺或引流管可见胆汁样液体判断。
1.4 统计学处理
应用SPSS统计学软件对数据分析,两组手术相关指标比较采用t检验,术后并发症相关指标比较采用Fisher确切概率法,术后随访采用χ2 检验,P < 0.05为差异有统计学意义。
2. 结果
所有患者均完成手术,无手术死亡。两组术后住院时间、术后并发症发生率,差异有统计学差异(P < 0.05),Beger组优于PD组。56例(Beger组29例,PD组27例)患者获随访6个月~5 a,无肿瘤或结石复发,疼痛缓解率、新发糖尿病、新发脂肪泻等指标,差异无统计学意义(P > 0.05),见表2。
表 2 两组手术相关指标比较($\bar x \pm s $ )Table 2. Comparison of surgical indicators between the two groups ($ \bar x \pm s$ )指标 Beger组(n = 31) PD组(n = 28) t/χ2 P 手术时间(min) 231.4 ± 42.3 268.1 ± 52.5 2.98 0.06 术中出血量(mL) 405.5 ± 64.1 449.9 ± 61.2 13.18 0.08 术后住院时间(d) 17.1 ± 3.4 28.5 ± 4.1 −17.85 < 0.001 术后并发症[n(/%)] 4/12.9 12/42.9 5.31 0.01 术后出血 0 2 胰漏 3 2 胆漏 1 1 不全性肠梗阻 0 3 非计划再次手术 0 2 胃瘫 0 2 新发脂肪泻(n) 2 3 0.77 0.07 新发糖尿病(n) 2 2 0.85 0.92 疼痛缓解(n) 有效 26 24 1.68 0.79 无变化 3 3 0.91 0.83 3. 讨论
胰头部炎症肿块导致患者疼痛的病理基础是炎症区域淋巴细胞浸润和神经束膜崩解等病理学改变,且胰头部炎性病变较胰体尾部更重,发生时间更早,故去除胰头部炎性病变,可减轻疼痛及炎性包块对胆管、十二指肠的压迫症状,明确病灶性质,同时也阻止胰腺慢性纤维化的持续发展,避免患者内、外分泌功能的严重受损。胰头肿块型慢性胰腺炎传统的手术方式包括胰十二指肠切除术、保留幽门的胰十二指肠切除术等,对于胰头部良性病变而言创伤过大,切除了过多正常器官,患者术后生活质量受到不同程度的影响[1-3]。1985年德国乌尔姆大学外科医院 Hans G·Beger 教授[4]报道并总结了保留十二指肠胰头切除治疗慢性胰腺炎患者的10 a手术经验,此后该术式在全球逐渐推广,并被命名为 Beger手术,又称保留十二指肠的胰头切除术(duodenum-preserving pancreatic head resection,DPPHR)。目前普遍认为DPPHR适用于胰头肿块型慢性胰腺炎、胰头囊肿或良性肿瘤,以及胰头部位未侵犯十二指肠及胆总管,无需行淋巴结清扫低度恶性肿瘤[3]。DPPHR较传统术式而言,手术创伤小,不破坏消化道的正常解剖和完整性,具有更低的手术并发症和死亡率。但该手术没有绝对适应证,对手术操作技巧及经验要求很高,难度较大。有关DPPHR治疗胰头部占位的手术并发症相关Meta分析,提示胰瘘、二次手术率、病死率等严重术后并发症发生率与PD术无明显差异,但DPPHR能够更为有效地避免胰腺内、外分泌功能受损[5-6]。本治疗组发生胰漏3例(9.68 %)、新发糖尿病、脂肪泻各2例,与同期PD组比较并无优势。但因手术创伤及腹腔骚扰较小,无术后出血、肠梗阻、胃瘫及非计划再次手术发生,术后住院时间较PD组明显缩短,节约了医疗成本。尤其对胰头肿块型慢性胰腺炎,DPPHR术后疼痛症状改善明显,患者更易接受,满意度较高。本组DPPHR术后随访良性和低度恶性肿瘤患者尚未见复发。相对PD,在确保胰头病灶切除的原则,DPPHR进一步降低机体损伤以及手术并发症,术中输血更少,术后住院时间更短,术后职业康复和生活质量得到显著提高[7-8]。
对于慢性胰腺炎、胰腺良性、交界性及低度恶性肿瘤患者,切除病变组织、改善患者的腹痛症状,防止病变癌变才是手术的最终目的,无论是采用 DPPHR 或 PD,均能够彻底切除病变,达到理想的手术效果。结合文献[9-11],笔者体会,对此类患者行Beger手术的指征为:(1)胰头部慢性胰腺炎内科或内镜治疗不能解决的顽固性腹痛;(2)邻近器官出现局部并发症,如胆道梗阻、十二指肠梗阻、假性动脉瘤或门静脉受累等;(3)不排除恶变者。胰头肿块型慢性胰腺炎早期手术比晚期手术获益更大,可取得理想的长期缓解疼痛效果。早期手术后发生胰腺外分泌功能不全的风险也更低。与晚期行手术者相比,对发病 < 3 a的患者早期手术,其长期生活质量将获得改善。本组患者术后顽固性疼痛缓解率达到89.7%(26/29)。
改良Beger手术重点及难点是确保十二指肠以及胆总管血供,避免十二指肠及胆管壁坏死而导致手术失败。如何顺利完成手术,结合文献[2,12],笔者体会;(1)离断胰腺颈部是首要步骤。一般情况,解剖分离肠系膜上静脉并不困难,但慢性胰腺炎往往出现血管炎性浸润,炎症致密黏连,多数情况胰颈后隧道封闭,经验不足,强行分离可能出现难以控制的大出血。笔者的经验是,病程较长胰颈炎症致密黏连者,先解剖辨认门静脉、肠系膜上静脉在胰颈的出入点,参照血管轨迹用蚊式钳逐一钳夹结扎胰腺组织,可完整显露血管。离断胰腺颈部,向右牵拉胰头部,从容离断肠系膜上静脉右侧属支,切除胰头,特别是钩突部胰腺组织,最大限度去除炎性病变,解除对肠系膜上静脉的压迫;(2)保留少部分薄层胰头组织及十二指肠内侧血管弓的完整:切除胰头部炎性病变,需保留十二指肠内侧部分胰腺织,至少保留一侧的十二指肠内侧形成的血管弓,避免十二指肠及胆管下端缺血。有研究表明,胰十二指肠动脉缘大部分行走于胰后筋膜内,保全胰后筋膜的完整性即保证了十二指肠的血供[13]。笔者体会,显露胰头时,应重点保护胃十二指肠动脉,切除钩突时,不损伤胰后筋膜。至少保留距离十二指肠约 0.5~0.7 cm 范围内的胰头组织并确切缝扎主胰管,保证血管弓的完整性。对胰头严重黏连者,如果刻意准求胰头的彻底切除,则增加损伤前后动脉弓血管的几率,造成十二指肠缺血坏死的严重并发症。合并胆管下段炎性狭窄的处理:胰头部炎性包块常可引起胆管下段狭窄,导致梗阻性黄疸。切除胰头部组织时,可在胰头创面内行胆管下段开窗,引流胆汁于胰腺创面内,为避免开窗的胆管下段再愈合狭窄,可将切开的胆管侧壁与胰腺创面缝合,近侧的胆总管切开并置入 T 管引流,既可在围手术期保护远侧胰肠吻合口,也可术后造影观察远侧胆管通畅情况。(3)避免胰内胆管壁损伤。Beger手术由于保留了胆管周围的胰腺组织,肉眼不易确切辨别胰内胆管的走行,经验不足必然损伤胆管。有主张切除胰头时,胆总管预切开,置入金属探条引导保护胆管。也行胆总管切开,远端置入导尿管作为引导者,但有时通过较为困难。笔者的经验是于胆囊管开口置入取石网篮,容易通过十二指肠乳头,在手指触摸下辨别胆管的走行路径保留薄层胰腺组织,既不损伤胆管,又不需切开胆总管T管引流,病变胰腺组织也得到了最大限度切除,简单有效。
应用标准的Whipple 术式或保留幽门胰十二指肠切除术治疗胰腺良性疾病及低度恶性肿瘤目前仍然是经典治疗方法。改良Beger手术切除胰腺组织少、手术创伤小、手术安全、恢复更快、对缓解顽固性腹痛确切、患者术后生存质量及营养状况明显改善。但晚期胰腺炎疼痛的处理非常复杂,许多非手术和外科治疗方法及疗效仍需进一步评估,应用也需慎重。
-
表 1 纳入文献的基本信息和质量评价结果(n=19)
Table 1. Basic characteristics and evaluation of included literatures (n=19)
纳入文献 发表年份 研究类型 国家 样本量 跌倒发生率 影响因素 NOS/AHRQ评分 Komatsu,Hiroko等[6] 2018年 横断面研究 日本 50 0.180 abechr 7 Argyriou,Andreas A等[7] 2020年 队列研究 希腊 122 0.172 bip 6 Bao,Ting等[8] 2016年 横断面研究 美国 296 0.319 p 9 Capone,Luann J等[3] 2012年 病例对照 美国 286 0.030 bfijlnouvwy 6 Chen,Tuo-Yu等[9] 2014年 病例对照 美国 1640 0.303 oy 7 Huang,Min H等[10] 2019年 队列研究 美国 1097 0.233 acdfjmprsy 9 Huang,Min H等[11] 2015年 队列研究 美国 41 0.560 bijmt 8 Kenis,Cindy等[12] 2022年 病例对照 比利时 3681 0.209 bdfgikoqstxz 9 Komatsu,Hiroko等[4] 2019年 横断面研究 日本 88 0.491 aech 9 Kong,Qiu-Huan等[13] 2014年 队列研究 中国 203 0.133 bfhnsxyz 6 Lamba,Nayan等[14] 2021年 病例对照 美国 42759 0.241 bdi 7 Pandya,Chintan等[15] 2016年 横断面研究 美国 17958 0.252 abecdijprsz 11 Saberi,Najmeh等[16] 2022年 横断面研究 伊朗 300 0.353 bedghijm 8 Rattanakrong,Nida等[17] 2022年 队列研究 泰国 123 0.236 lmp 9 Puts,Martine T E等[18] 2013年 队列研究 加拿大 112 0.152 bdhijsz 7 Turner,Justin P等[19] 2017年 横断面研究 澳大利亚 385 0.239 btuvz 7 Vande Walle,Nathalie等[20] 2014年 队列研究 比利时 809 0.176 bdfkoqrstxz 8 Wildes,Tanya M等[21] 2018年 横断面研究 美国 498 0.183 stw 8 刘伟等[22] 2021年 队列研究 中国 60 0.283 m 8 注:影响因素:a:年龄;b:性别;c:文化程度;d:居住情况;e:工作情况;f:跌倒史;g:跌倒恐惧;h:肿瘤分期;i:肿瘤分类;j:肿瘤治疗方式;k:营养状况;l:体重;m:BMI;n:发热;o:疼痛;p:周围神经病变;q:疲乏;r:抑郁;s:共病;t:多重用药;u:抗抑郁药;v:抗精神病药;w:镇静催眠药;x:认知功能;y: 平衡与步态;z:日常生活能力。 表 2 成人肿瘤患者跌倒影响因素Meta分析结果(2)
Table 2. Meta analysis results on the influencing factors of falls in adult tumor patients(2)
-
[1] Sung H,Ferlay J,Siegel R L,et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries[J]. CA Cancer J Clin.,2021,71(3):209-249. doi: 10.3322/caac.21660 [2] Melissa S,Kathy M,Thomas S,et al. Addressing falls among older oncology patients through complexity science.[J]. Nursing Administration Quarterly,2019,43(3):280-288. doi: 10.1097/NAQ.0000000000000360 [3] Capone L J,Albert N M,Bena J F,Tang A S. Predictors of a fall event in hospitalized patients with cancer[J]. Oncol Nurs Forum,2012,39(5):E407-E415. [4] Hiroko K ,Kaori Y ,Yasuhiro K ,et al. Falls and functional impairments in breast cancer patients with chemotherapy-induced peripheral neuropathy[J]. Asia-Pacific Journal of Oncology Nursing,2019,6(3):253-260. [5] Zhao J,Wang G,Chen L,Yu S,Li W. Risk factors for falls in hospitalized patients with cancer:A systematic review and meta-analysis[J]. Asia Pac J Oncol Nurs,2022,9(8):100107. doi: 10.1016/j.apjon.2022.100107 [6] Hiroko K ,Kaori Y,Yasuo H ,et al. Falls and physical inactivity in patients with gastrointestinal cancer and hand-foot syndrome[J]. Asia-Pacific Journal of Oncology Nursing,2018,5(3):307-313. [7] Argyriou A A,Bruna J,Anastopoulou G G ,Velasco R,Litsardopoulos P,Kalofonos HP. Assessing risk factors of falls in cancer patients with chemotherapy-induced peripheral neurotoxicity[J]. Support Care Cancer,2020,28(4):1991-1995. doi: 10.1007/s00520-019-05023-5 [8] Ting B,Coby B,Christina S,et al. Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence,risk factors,and fall risk.[J]. Breast Cancer Research and Treatment,2016,159(2):327-33. doi: 10.1007/s10549-016-3939-0 [9] Tuo-Yu C ,C M J. Predictors of falls among community-dwelling older adults with cancer: results from the health and retirement study[J]. Supportive Care in Cancer : Official Journal of the Multinational Association of Supportive Care in Cancer,2014,22(2):479-85. [10] Huang H M ,Blackwood J ,Godoshian M ,et al. Predictors of falls in older survivors of breast and prostate cancer: A retrospective cohort study of surveillance,epidemiology and end results—Medicare health outcomes survey linkage[J]. Journal of Geriatric Oncology,2018,10(1):89-97. [11] Huang MH,Shilling T,Miller KA,Smith K,LaVictoire K. History of falls,gait,balance,and fall risks in older cancer survivors living in the community[J]. Clin Interv Aging,2015,10:1497-1503. doi: 10.2147/CIA.S89067 [12] Cindy K ,Lore D ,Johan F ,et al. Incidence of falls and fall-related injuries and their predictive factors in frail older persons with cancer: A multicenter study[J]. BMC Geriatrics,2022,22(1):877-877. [13] Kong Q ,Wang Y ,Song C ,et al. Prospective analysis of the risk factors for falls in lymphoma patients[J]. European Journal of Oncology Nursing,2014,18(5):540-544. [14] Nayan L ,Fang C ,N D C ,et al. Frequency,etiologies,risk factors,and sequelae of falls among patients with brain metastases: A population- and institutional-level analysis[J]. Neuro-oncology Practice,2022,9(2):114-122. [15] Pandya C ,Magnuson A ,Dale W ,et al. Association of falls with health-related quality of life (HRQOL) in older cancer survivors: A population based study[J]. Journal of Geriatric Oncology,2016,7(3):201-210. [16] Najmeh S ,Ali K D ,Mahnaz I ,et al. Falls in older ambulatory care patients with cancer in Iran: Implications for clinical practice[J]. Journal of Evaluation in Clinical Practice,2021,28(4):624-630. [17] Nida R ,Akkradate S ,Sujitra B. Incidence and risk factors associated with falls among women with breast cancer during taxane-based chemotherapy[J]. Supportive care in cancer : Official journal of the Multinational Association of Supportive Care in Cancer,2022,30(9):7499-7508. [18] Puts M T,Monette J,Girre V,et al. The fall rate of older community-dwelling cancer patients[J]. Support Care Cancer.,2013,21(3):775-783. [19] Turner,Justin P et al. “Factors associated with use of falls risk-increasing drugs among patients of a geriatric oncology outpatient clinic in Australia: A cross-sectional study”[J]. Journal of Evaluation in Clinical Practice,2017,23(2):361-368. [20] Nathalie W V ,Cindy K ,Pieter H ,et al. Fall predictors in older cancer patients: A multicenter prospective study[J]. BMC Geriatrics,2014,14(2):135. [21] Wildes T M,Maggiore R J,Tew W P,et al. Factors associated with falls in older adults with cancer: A validated model from the Cancer and Aging Research Group[J]. Support Care Cancer,2018,26(10):3563-3570. doi: 10.1007/s00520-018-4212-3 [22] 刘伟,刘晓明. 老年乳腺癌全乳切除术后患者跌倒发生情况及其影响因素[J]. 中国老年学杂志,2021,41(18):4101-4104. doi: 10.3969/j.issn.1005-9202.2021.18.060 [23] James S L,Lucchesi L R,Bisignano C et al. The global burden of falls: global,regional and national estimates of morbidity and mortality from the global burden of disease study 2017[J]. Inj Prev,2020,26:3-11. [24] 康宁,于海军,陆晓敏等. 中国老年人跌倒发生率的Meta分析[J]. 中国循证医学杂志,2022,22(10):1142-1148. [25] 杨欣,姚梅琪,张玉萍等. 住院老年患者跌倒风险与风险感知的差异性研究[J]. 中华护理杂志,2023,58(19):2326-2332. [26] 荆凤,王园园,邢唯杰等. 乳腺癌患者芳香化酶抑制剂诱导的骨关节症状预防和管理的证据总结[J]. 中华护理杂志,2023,58(7):808-815. [27] Sattar S,Kenis C,Haase K,et al. Falls in older patients with cancer: Nursing and allied health group of international society of geriatric oncology review paper[J]. J Geriatr Oncol,2020,11(1):1-7. doi: 10.1016/j.jgo.2019.03.020 [28] 张雨欣,张开利. 老年人恐惧跌倒相关性活动限制的研究进展[J]. 中华护理杂志,2023,58(1):112-116. doi: 10.3761/j.issn.0254-1769.2023.01.016 [29] 任晓华,关琼瑶,马祥萍,等. 云南省肿瘤科护士癌痛知识知晓及癌痛护理开展现状调查[J]. 昆明医科大学学报,2021,42(9):167-172. [30] 李思思,张艳,李宏洁,等. 老年癌症患者共病的研究进展[J]. 中国全科医学,2020,23(7):880-883+888. [31] 田露,陈英,龙艳慧,等. 肿瘤患者化疗后居家跌倒预防自我管理体验的质性研究[J]. 中华护理杂志,2020,55(11):1648-1652. doi: 10.3761/j.issn.0254-1769.2020.11.008 [32] 中国抗癌协会肿瘤支持治疗专业委员会,中国抗癌协会肿瘤临床化疗专业委员会. 化疗诱导的周围神经病变诊治中国专家共识(2022版). 中华肿瘤杂志,2022,44(9): 928-934. [33] 王静,罗雨田,叶琼告,等. 宫颈癌化疗病人癌因性疲乏程度及影响因素分析[J]. 护理研究,2021,35(4):630-633. [34] Strini V,Schiavolin R,Prendin A. Fall Risk Assessment Scales: A Systematic Literature Review[J]. Nurs Rep,2021,11(2):430-443. [35] 肖先皓,宋禾,周建平. 肿瘤相关性肌肉减少症的发病危险因素分析—一项基于NHANES数据库的研究[J]. 中国实用外科杂志,2024,44(2):194-198. [36] 周华萍,甘彩芳,程菁,等. 营养状态指标对老年食管癌患者化疗耐受性的影响[J]. 中国老年学杂志,2024,44(4):802-805. doi: 10.3969/j.issn.1005-9202.2024.04.011 -








 下载:
下载:



 下载:
下载:



