The Effects of Physical Activity Duration,Sleep Quality,and Weight Control on Patient-Reported Outcomes in Hypertensive Patients
-
摘要:
目的 探讨高血压患者体力活动时长、睡眠质量、体重控制与患者报告结局(patient- reported outcomes,PRO)之间的关系,为高血压患者PRO的提高提供有效信息。 方法 2020年4—6月自云南省4个县中随机抽取625例高血压患者参加现场调查。问卷内容包括患者基本情况、生活方式、健康状况及高血压患者报告结局量表-PROISCD-HY(V1.0)。t检验、方差分析及多元线性回归用于分析体力活动时长、睡眠质量、体重控制与PRO之间的关系,并用Bootstrap法检验中介效应。 结果 调整潜在协变量后,多元线性回归模型显示体力活动时长≥2 h与PRO显著相关[B = 6.551,95%CI(2.611,10.491)],分层后发现关联仅在男性、女性及中青年中存在,在老年人中不存在。睡眠质量好与PRO之间均存在显著相关性[B = 1.870,95%CI(0.449,3.291)],关联在各人群中均存在。通过运动+饮食控制的患者PRO得分升高[B = 1.904,95%CI(0.383,3.424)],饮食及其他方式控制体重的患者PRO得分降低[B = -4.873,95%CI(-7.860,-1.887);B = -7.105,95%CI(-12.211,-1.999)],各人群关联情况不同。Bootstrap法发现体力活动时长对PRO存在直接和间接影响,睡眠质量在体力活动时长与PRO间起部分中介作用。 结论 体力活动时长≥2 h,睡眠质量好,控制体重能提高高血压患者的PRO。 Abstract:Objective To investigate the correlation between physical activity duration, sleep quality, weight control, and PRO(patient- reported outcomes) in individuals with hypertension, providing effective information for enhancing patient-reported outcomes in this population. Methods A total of 625 hypertensive patients were randomly selected from four counties in Yunnan Province from April to June 2020 to participate in a field survey. The questionnaire included patients' basic information, lifestyle, health status and the PRO Scale for Hypertension-PROISCD-HY (V1.0). Statistical analyses including t-tests, one-way ANOVA, and multivariate linear regression were conducted to investigate the relationships between physical activity duration, sleep quality, weight control, and PRO, with the Bootstrap method used to examine potential mediating effects. Results After adjusting for potential covariates, the multiple linear regression model indicated a significant association between a physical activity duration of ≥2 hours with PRO[B = 6.551, 95%CI(2.611, 10.491)]. Stratified analysis showed that this association was only present among males, females, and younger adults, but not in older adults. Additionally, a positive correlation was found between good sleep quality and PRO[B = 1.870, 95%CI(0.449, 3.291)], with this association being consistent across all populations after stratification. Patients who managed their condition through exercise and diet had higher PRO scores[B = 1.904, 95%CI(0.383, 3.424)], while those controlling weight through diet and other methods exhibited a decrease in PRO scores[B = -4.873, 95%CI(-7.860, -1.887); B = -7.105, 95%CI(-12.211, -1.999)], with variations among different groups. The bootstrap method revealed that physical activity duration had both direct and indirect effects on PRO, with sleep quality acting as a partial mediator between physical activity duration and PRO. Conclusion A Physical activity duration of at least 2 hours, good sleep quality, and weight control have been shown to improve PRO in individuals with hypertension. -
Key words:
- Hypertension /
- Patient-reported outcomes /
- Multiple linear regression /
- Bootstrap
-
岗松 (Baeckeafrutescens)为桃金娘科 (Myrtaceae) 岗松属 (BaeckeaL.) 植物,是南方民间的常用著名药材。以叶如松针较短而得名,又名鸡儿松、松毛枝、长松、沙松等。全球约有68种岗松属植物,而我国仅有岗松一个种,主要分布于海南、广东、广西、福建、浙江、江西等省份[1]。岗松属植物主要含有挥发油、间苯三酚、黄酮类、萜类等化学成分。其中,二氢黄酮类成分是一种的具有广泛的药理作用的化合物,如抗癌[2]、PTP1B抑制[3]、抗氧化[4]、抗菌[5]和抗炎[6-7]等活性。具有生物活性的天然产物一直以来都是治疗各种疾病的新药的最有价值的来源之一[8]。
作为本研究组对桃金娘科植物中活性次生代谢产物挖掘研究工作的一部分,本研究从岗松的枝叶中分离得到5个二氢黄酮类化合物,图1,其中化合物1、3和5为首次从该植物中分离得到。尽管这些成分已被报道[9-16],但它们的绝对构型报道较混乱。因此,笔者采用手性拆分、ORD和ECD计算的方法进一步确定了它们的绝对构型。此外,评价了这些成分对4种人肿瘤细胞株(HCT116、Hela、DU145和A549)的细胞毒活性。
1. 材料与方法
1.1 材料与仪器
旋光数据在AUTOPOL Ⅵ旋光仪上测定;圆二色谱在Applied Photophysics分光偏振计上测定;NMR谱在Bruker Avance Ⅲ-500核磁共振仪上测定,TMS作为内标;ESI-MS在Agilent 1290 UPLC/6540 Q-TOF质谱仪上测定;硅胶 (80~100目,200~300目,中国青岛海祥化工厂);凝胶为Sephadex LH-20 (40~70 μm;Healthcare BioSciences AB,Uppsala, Sweden),反相填充材料Rp-18(50 μm, 德国Merck公司);半制备型HPLC为Agilent 1260型高效液相色谱;色谱柱为ZORBAXSB-C18柱 (9.4 × 250 mm, 5.0 μm) , CHIRALPAK IC (4.64 × 250 mm, 10 × 250 mm, 5.0 μm)柱。
1.2 植物标本来源
岗松 (B. frutescens) 枝叶于2016年10月采自广西壮族自治区东兴市,由中国科学院昆明植物研究所李嵘研究员鉴定。标本保存于中国科学院昆明植物研究所植物化学与西部植物资源持续利用国家重点实验室刘海洋课题组。
1.3 实验方法
1.3.1 提取分离
岗松枝叶 (10.0 kg) 粉碎后甲醇回流提取3次,合并提取液,减压回收甲醇,得到浸膏1.3 kg。浸膏用1.0 kg 硅胶 (80~100 目)拌样,2.0 kg 硅胶 (200~300 目)装柱,用石油醚-乙酸乙酯 (1∶0→0∶1,v/v) 和氯仿-甲醇 (1∶0→1∶1,v/v) 梯度洗脱得到七个 (Fr.1-Fr.7) 不同馏分。Fr.2 (53 g) 用正相硅胶划段(石油醚-丙酮,1∶0→1∶1,v/v)后,合并为三个馏分,经反复使用Rp-18色谱柱(甲醇-水,1∶1→1∶0,v/v),硅胶柱层析 (石油醚-丙酮,10∶1→1∶1,v/v), Sephadex LH-20色谱柱(氯仿-甲醇,1∶1,v/v)及半制备HPLC(乙腈-水,60%→80%,v/v)分离纯化得到了化合物1 (81.1 mg)、2 (23.6 mg)和3(401.5 mg)。Fr. 5 (48 g) 用MCI gel脱色,脱色后经Rp-18色谱柱 (甲醇-水,1∶1→1∶0,v/v),硅胶柱层析(氯仿-甲醇,1∶1,v/v),进一步使用半制备HPLC(乙腈-水,30%→50%,v/v)分离纯化得到了化合物4 (7.2 mg)和5 (118.7 mg)。
1.3.2 手性分析及拆分
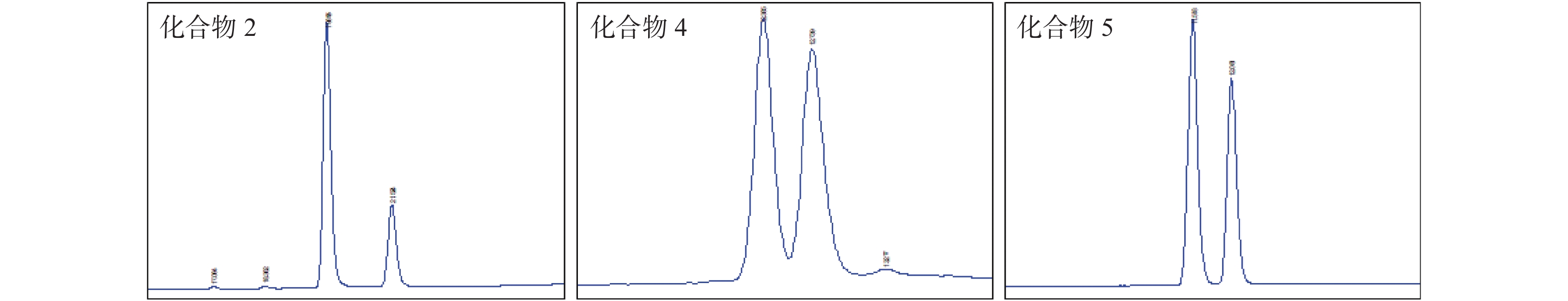
分离得到的化合物1-5分别进行HPLC手性分析 (色谱柱:CHIRALPAK I,4.64 × 250 mm, 5.0 μm; 色谱条件:正己烷-异丙醇,1∶0→3∶2, v/v, 30 min) , 显示化合物1和3只有一个峰,化合物2、4和5分别都有两个峰(图2)。进一步手性拆分 (色谱柱:CHIRALPAK I,10 × 250 mm, 5.0 μm; 色谱条件:正己烷-异丙醇,70∶30,v/v),分离得到(+)-2,(-)-2,(+)-4,(-)-4, (+)-5和(-)-5。
1.3.3 计算方法
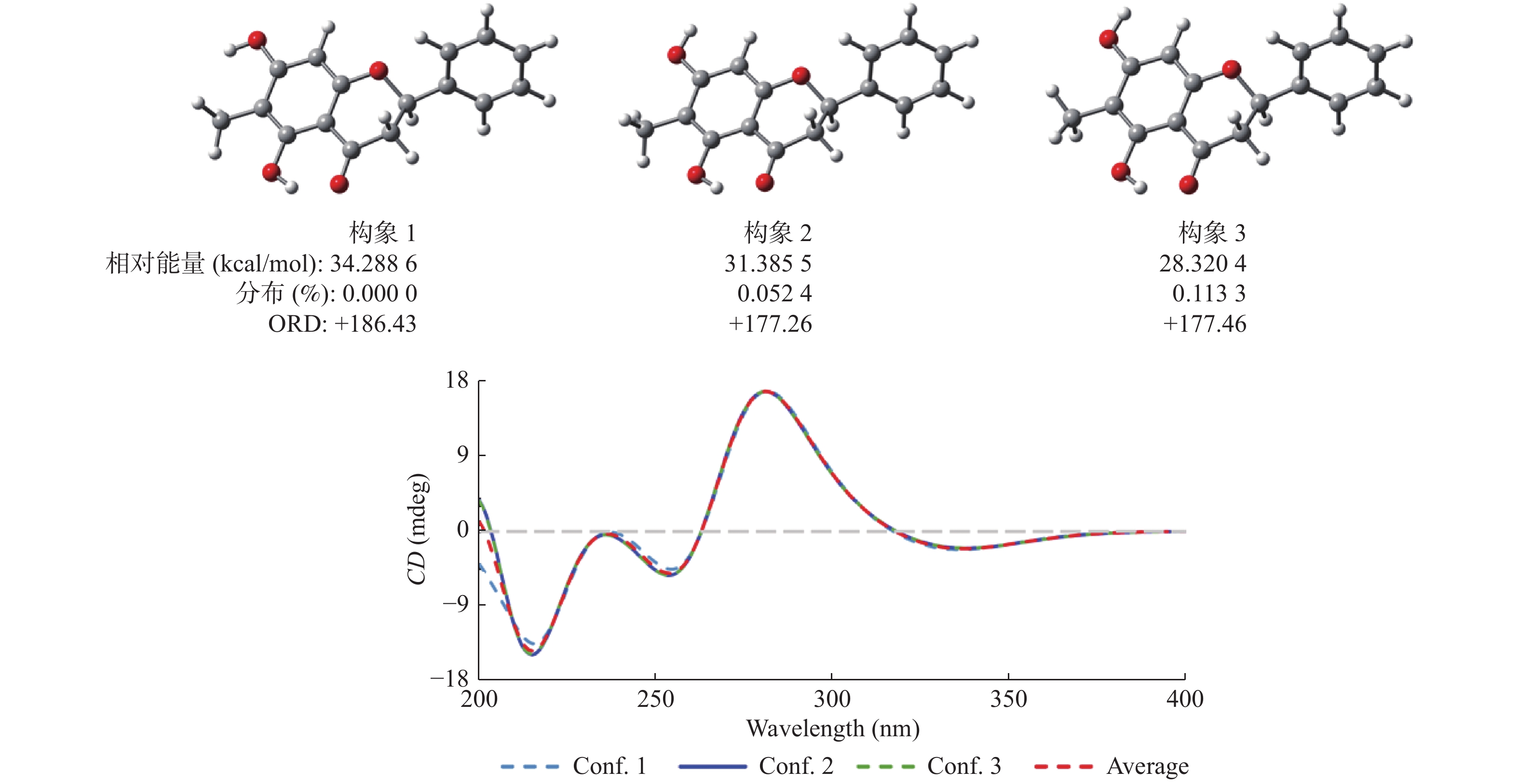
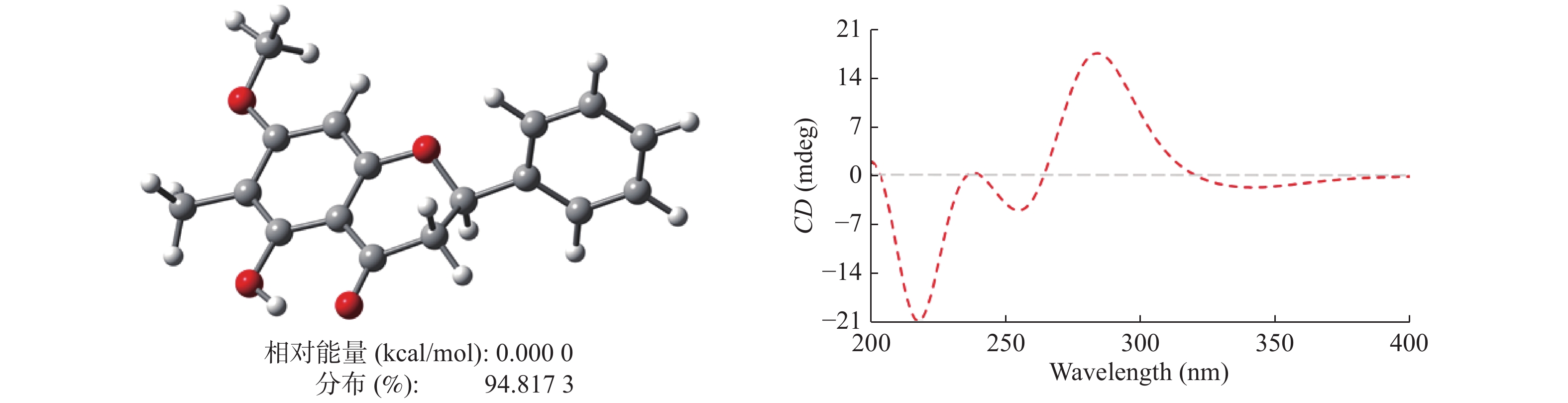
ORD和ECD的计算主要通过Gaussian 16软件来实现的。首先,化合物1和2的构象通过CONFLEX 8B软件进行了分析,并分别给出了3个 (图3)和1个 (图4) 可用构象。这些初始结构通过密度泛函理论 (DFT) 在B3LYP/6-31+G(d) 水平上进行了优化。优化后构象的ECD计算通过依时性密度泛函理论 (TDDFT) 在B3LYP/6-311++G (2d, p) 水平上进行,而ORD计算则通过依时性密度泛函理论 (TDDFT) 在B3LYP/6-31++G (d, p) 水平上进行。计算后的ECD图谱通过SpecDis 1.6软件来实现其可视化。
1.3.4 细胞毒活性
在96孔微孔板上使用MTT法评估化合物1‒5对四种人肿瘤细胞株 (HCT116、CCRF-CEM、DU145和A549)的细胞毒活性。对化合物进行了5个剂量测试,剂量范围为10‒8~10‒4 M,各化合物的IC50值通过非线性回归分析计算。以广谱抗肿瘤药喜树碱(CPT)为阳性对照,每个试验重复3次。
2. 结果
化合物1:淡黄色粉末C16H14O6;negative ESI-MSm/z 269 [M‒H]‒;[α] ‒46.8 (c = 0.22,MeOH);ECD (MeOH) λmax (Δε)220 (+3.26),237 (‒0.08),256 (+0.79),281 (‒3.56),336 (+0.46) nm;1H NMR(Acetone-d6,500 MHz) δ: 5.51 (1H,dd,J = 12.9,2.7 Hz,H-2),1.97 (3H,s,H3-6),6.07 (1H,s,H-8),7.38 (1H,m,H-4′ ),7.43 (2H,m,H-3′ /H-5′ ),7.55 (2H,d,J = 7.4 Hz,H-2′ /H-6′ ),12.42 (1H,s,OH-5),3.31 (1H,dd,J = 17.1,12.9 Hz,H-3a),2.78 (1H,dd,J = 17.1,2.7 Hz,H-3b);13C NMR (Acetone-d6,125 MHz)δ: 79.9 (C-2),43.7 (C-3),196.8 (C-4),162.4 (C-5),104.8 (C-6),7.0 (6-CH3),165.1 (C-7),95.2 (CH-8),161.6 (C-9),103.0 (C-10),140.2 (C-1′ ),127.3 ×2 (CH-2′ /CH-6′ ),129.4 ×2 (CH-3′ /CH-5′ ),129.3 (CH-4′ )。以上数据与文献[10]报道的5,7-二羟基-6-甲基二氢黄酮的数据基本一致。
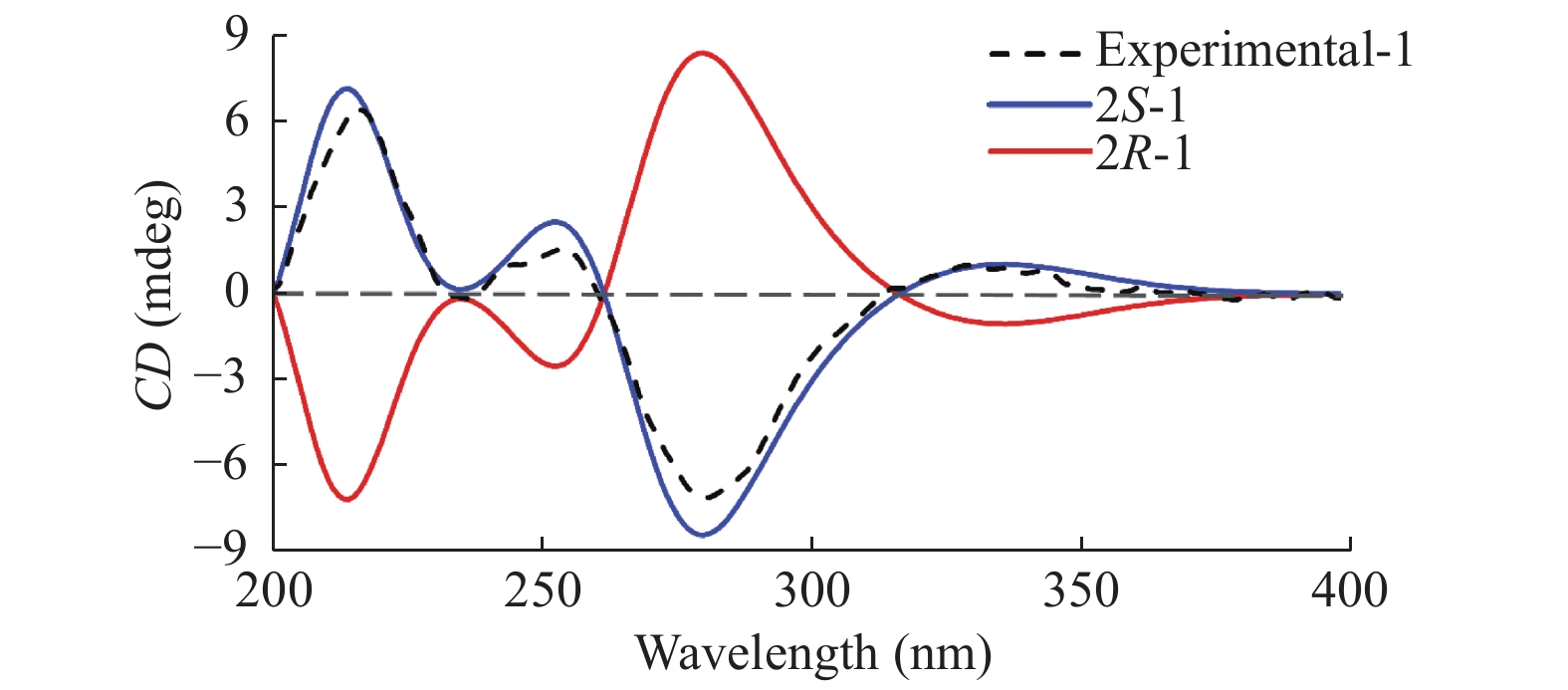
初步ORD计算结果表明, (2R)-1的比旋光值为正值(+180.38), 而化合物1的测试比旋光值为‒46.8 (c = 0.22,MeOH), 由此推断化合物1为2S构型,此结论通过后续的ECD计算(图5)结果进一步得到证实。
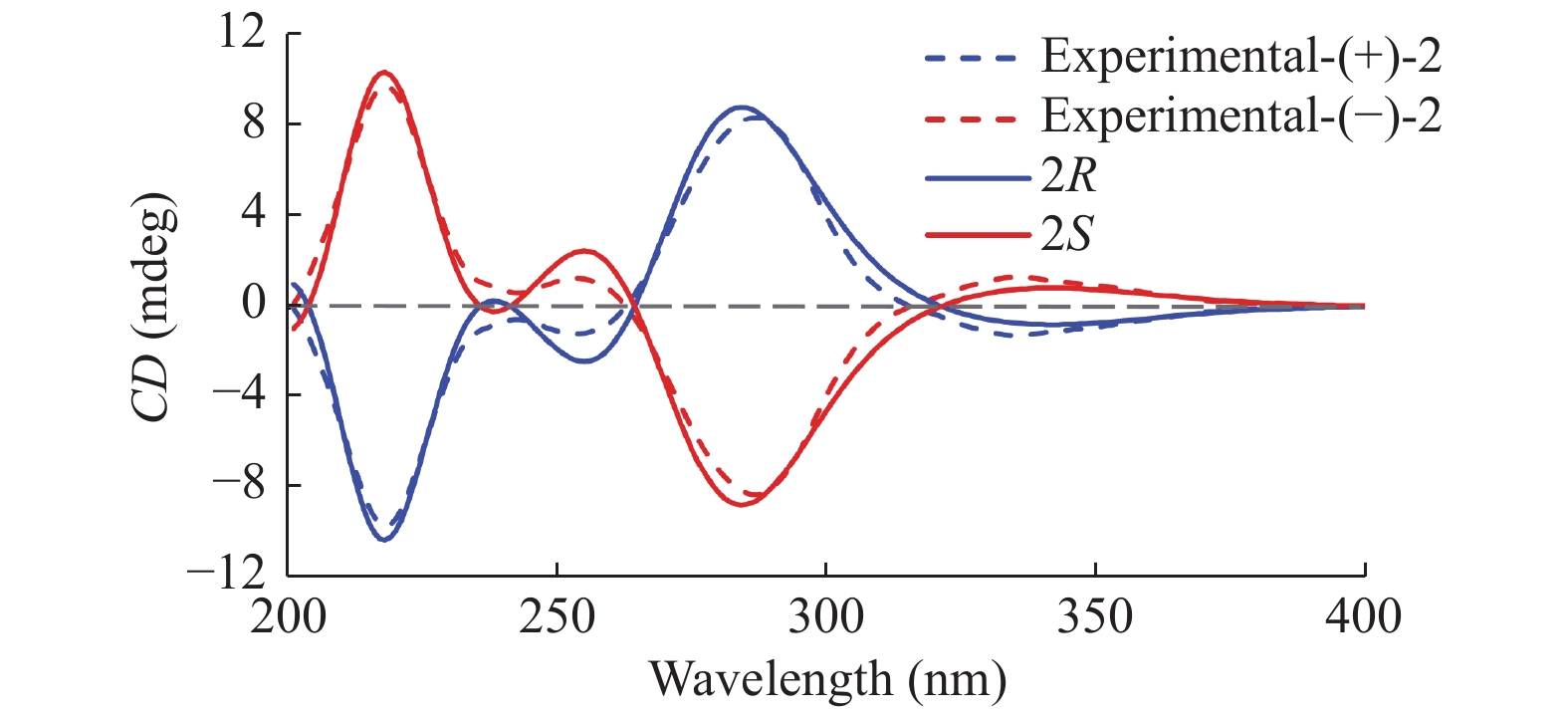
化合物2:淡黄色粉末C17H16O4;negative ESI-MSm/z283 [M -H]-; [α] +21.5 (c = 0.14, MeOH) for (+)-2, [α] -21.4 (c = 0.14, MeOH) for (-)-2; ECD (MeOH) λmax (Δε)220 (-3.20), 242 (-0.19), 254 (-0.41), 287 (+2.79), 338 (-0.43) nm for (+)-2, ECD (MeOH) λmax (Δε)220 (+3.20), 237 (+0.19), 256 (+0.41), 287 (+2.79), 338 (+0.43) nm for (-)-2; 1H NMR (CDCl3, 500 MHz) δ: 2.01 (3H, s, CH3-6), 2.86 (1H, dd, J = 17.1, 3.1 Hz, H-3b), 3.04 (1H, dd, J = 17.1, 12.7 Hz, H-3a), 3.86 (3H, s, OCH3-7), 5.42 (1H, dd, J = 12.7, 3.1 Hz, H-2), 6.10 (1H, s, H-8), 7.36~7.48 (5H, m, H-2'-H-6'), 12.12 (1H, s, OH-5); 13C NMR data (CDCl3, 125 MHz)δ: 78.5 (C-2), 43.5 (C-3), 196.3 (C-4), 162.4 (C-5), 105.0 (C-6), 166.0 (C-7), 92.3 (C-8), 158.9 (C-9), 102.9 (C-10), 139.0 (C-1'), 125.9 (C-2'), 128.8 (C-3'), 128.6 (C-4'), 128.8 (C-5'), 125.9 (C-6'), 7.6 (6-Me), 55.9 (7-OMe). 13C NMR data显示其与化合物1高度相似,主要区别在于多了一个甲氧基的信号。化合物2与文献[11]报道的化合物5-羟基-7-甲氧基-6-甲基二氢黄酮数据基本一致。经进一步手性拆分并结合ECD计算结果 (图6) 分别确定(+)-2 {[α] +21.5 (c = 0.14, MeOH)} 和(-)-2{[α]-21.4 (c = 0.14, MeOH)}的绝对构型分别为2R和2S。
化合物3:淡黄色粉末C17H16O4; negative ESI-MS m/z269 [M ‒H]‒; [α] ‒20.8 (c = 0.12, MeOH); 1H NMR (CDCl3, 500 MHz)δ: 2.82 (1H, dd, J = 17.2, 3.1Hz, H-3b), 3.08 (1H, dd, J = 17.2, 13.1Hz, H-3a), 3.80 (3H, s, OCH3-7), 5.41 (1H, dd, J = 13.1, 3.1 Hz, H-2), 6.06 (1H, d, J = 2.3Hz, H-6), 6.08 (1H, d, J = 2.3Hz, H-8), 7.37~7.47 (5H, m, H-2'‒H-6'), 12.03 (1H, s, OH-5); 13C NMR data (CDCl3, 125 MHz)δ: 79.3 (C-2), 43.4 (C-3), 195.8 (C-4), 164.2 (C-5), 95.2 (C-6), 168.0 (C-7), 94.3 (C-8), 162.8 (C-9), 103.2 (C-10), 138.4 (C-1'), 126.2 (C-2'), 128.9 (C-3'), 128.9 (C-4'), 128.9 (C-5'), 126.2 (C-6'), 55.7(7-OMe)。以上数据与文献报道的(2S)-乔松酮[11,12]数据基本一致。通过与化合物1的比旋光值对比而判定其绝对构型为2S。
化合物4:淡黄色粉末C17H16O4; negative ESI-MS m/z283 [M ‒H]‒; [α]+38.5 (c = 0.16, MeOH) for (+)-4,[α]‒38.6 (c = 0.16, MeOH) for (‒)-4;ECD (MeOH) λmax (Δε) 218 (‒3.45), 243 (‒0.17), 254 (‒0.41), 289 (+3.00), 338 (‒0.44) nm for (+)-4, ECD (MeOH) λmax (Δε) 218 (+3.45), 243 (+0.17), 254 (+0.41), 289 (‒3.00), 338 (+0.44) nm for (‒)-4; 1H NMR (CDCl3, 500 MHz) δ: 2.01 (3H, s, CH3-6), 2.84 (1H, dd, J = 3.1, 3.1 Hz, H-3b), 3.04 (1H, dd, J = 3.1, 3.1 Hz, H-3a), 3.86 (3H, s, OCH3-7), 5.42 (1H, dd, J = 3.1, 3.1 Hz, H-2), 6.10 (1H, s, H-6), 7.42 (5H, m, H-2'‒H-6'), 12.12 (1H, s, OH-5); 13C NMR data (CDCl3, 125 MHz)δ: 78.5 (C-2), 43.4 (C-3), 196.3 (C-4), 162.4 (C-5), 92.2 (C-6), 166.0 (C-7), 104.9 (C-8), 158.8 (C-9), 102.8 (C-10), 138.9 (C-1'), 125.8 (C-2'), 128.8 (C-3'), 128.5 (C-4'), 128.8 (C-5'), 125.8 (C-6'), 55.9 (7-OMe), 7.5 (8-Me)。以上数据与文献报道的(±)-5-羟基-7-甲氧基-8-甲基二氢黄酮[13-14]数据基本一致。
化合物5:淡黄色粉末C17H16O4; negative ESI-MS m/z283 [M ‒H]‒; [α]‒41.5 (c = 0.18, MeOH) for (‒)-5;ECD (MeOH) λmax (Δε) 208(‒0.93), 219 (‒3.42), 243 (‒0.35), 254 (‒0.41), 292 (+3.21), 338 (‒0.54) nm for (+)-5, ECD (MeOH) λmax (Δε) 208 (+0.93), 219 (+3.42), 243 (+0.35), 254 (+0.41), 292 (‒3.21), 338 (+0.54) nm for (‒)-5; 1H NMR (Pyridine-d5, 500 MHz) δ: 2.39 (3H, s, CH3-6), 2.92 (1H, J = 17.0, 2.6 Hz, H-3a), 3.33 (1H, J = 17.0, 13.0 Hz, H-3b), 5.49 (1H, dd, J = 13.0, 2.6 Hz, H-2), 7.10 (1H, d, J = 8.1 Hz, H-5'), 7.27 (1H, d, J = 8.1 Hz, H-6'), 7.52 (1H, s, H-2'), 13.03 (1H, s, OH-5); 13C NMR data (Pyridine-d5, 125 MHz)δ:79.9 (C-2), 43.6 (C-3), 196.6 (C-4), 162.3 (C-5), 105.0 (C-6), 166.3 (C-7), 95.1 (C-8), 161.6 (C-9), 102.7 (C-10), 130.9 (C-1'), 115.4 (C-2'), 147.5 (C-3'), 147.9 (C-4'), 116.5 (C-5'), 118.8 (C-6'), 7.7 (6-Me)。以上数据与文献报道的(±)-6-甲基-圣草酚[15-16]数据基本一致。
通过与化合物2的测试ECD图谱对比,(+)-4/(+)-5和(‒)-4/(‒)-5的绝对构型分别确定为2R和2S,见图7。
以广谱抗肿瘤药喜树碱 (CPT) 为阳性对照,评价了以上化合物对4种人肿瘤细胞株 (HCT116、CCRF-CEM、DU145和A549)的细胞毒活性。结果显示化合物(±)-2对HCT116和DU145有一定的活性,IC50值分别为(41.84 ± 3.66) μΜ和(13.54 ± 1.15) μΜ;而化合物3对DU145的具有显著的细胞毒活性,IC50值为(4.56 ± 0.42) μΜ。
3. 讨论
从岗松中分离得到5个二氢黄酮类化合物,通过NMR和MS数据分析以及ORD和ECD计算确定了它们的结构及其绝对构型,其中化合物1、3和5为首次从该植物中分离得到。化合物3对DU145的具有显著的细胞毒活性,IC50值为4.56 μM。从自然界中得到的手性天然产物通常被认为是以光学纯形式生物合成的[17],但是已有大量的外消旋体或富含对映体的混合物已从自然来源报道[18]。有趣的是,岗松中的二氢黄酮类成分分别以光学纯 (1和3)、外消旋体 (4)和不对等对映体 (2和5)三种形式存在,此发现为二氢黄酮对映体的生物合成途径提供了一定证据。尽管比旋光值在一定程度上是判定光学纯单体绝对构型的重要指标之一[18],但在实际科学研究过程中,不对等对映体的实测值实际上是由对映体过量部分产生的,从而产生误判。因此,对于天然手性产物的立体异构体组成的评价理应引起更多的关注。
-
表 1 研究对象人口学特征的统计描述[n(%)]
Table 1. Statistical description of the demographic characteristics of the study population [n(%)]
变量 分类 男性(n = 255) 女性(n = 349) 总和(n = 604) 年龄(岁) 中青年(< 65岁) 114(44.71) 167(47.85) 281(46.52) 老年(≥65岁) 141(55.29) 182(52.15) 323(53.48) 民族 汉族 102(40.00) 207(59.31) 309(51.16) 彝族 153(60.00) 142(40.69) 295(48.84) 居住地 城市 15(5.88) 19(5.44) 34(5.63) 农村 240(92.12) 330(94.56) 570(94.37) 婚姻状况 未婚 3(1.18) 5(1.43) 8(1.32) 已婚/同居 232(90.98) 291(83.38) 523(86.59) 离异 3(1.18) 2(0.57) 5(0.83) 丧偶 17(6.67) 51(14.61) 68(11.26) 文化程度 小学及以下 112(43.92) 248(71.06) 360(59.60) 初中 120(47.06) 86(24.64) 206(34.11) 高中/中专/五年制大专 17(6.67) 12(3.44) 29(4.80) 大学(专科/本科) 6(2.35) 3(0.86) 9(1.49) 保险类型 未参加,自费 2(0.78) 4(1.15) 6(0.99) 城镇职工医保 17(6.67) 8(2.29) 25(4.14) 城镇居民医保 144(56.47) 148(42.41) 292(48.34) 新农村合作医保 89(34.90) 188(53.87) 277(45.86) 商业医保 0(0.00) 1(0.29) 1(0.17) 公费医疗 3(1.18) 0(0.00) 3(0.50) 经济状况 好 25(9.80) 31(8.88) 56(9.27) 中 177(69.41) 249(71.35) 426(70.53) 差 53(20.78) 69(19.77) 122(20.20) 表 2 不同人口学特征患者的PRO得分比较($ \bar x \pm s $)
Table 2. Comparison of PRO scores among patients with different demographic characteristics($ \bar x \pm s $)
变量 分类 PRO总分(分) t/F P 年龄(岁) 中青年(< 65岁) 75.48 ± 7.67 6.162 < 0.001* 老年(≥65岁) 71.78 ± 7.08 性别 男性 74.30 ± 7.40 2.196 0.028* 女性 72.93 ± 7.67 民族 汉族 73.83 ± 9.04 1.067 0.286 彝族 73.17 ± 5.67 居住地 城市 77.19 ± 7.97 2.935 0.003* 农村 73.29 ± 7.51 婚姻状况 未婚 72.85 ± 6.48 0.241 0.867 已婚/同居 73.60 ± 7.69 离异 73.78 ± 6.54 丧偶 72.81 ± 7.02 文化程度 小学及以下 72.15 ± 7.83 13.117 < 0.001* 初中 74.90 ± 6.61 高中/中专/五年制大专 78.89 ± 6.39 大学(专科/本科) 78.58 ± 7.13 保险类型 未参加,自费 74.26 ± 4.21 0.610 0.692 城镇职工医保 74.02 ± 6.45 城镇居民医保 73.06 ± 5.93 新农村合作医保 73.94 ± 9.11 商业医保 — 公费医疗 74.07 ± 11.17 经济状况 好 79.57 ± 8.84 30.857 < 0.001* 中 73.59 ± 6.54 差 70.42 ± 8.61 *P < 0.05。 表 3 体力活动时长、睡眠质量、体重控制与高血压患者PRO之间的关系
Table 3. Relationship between physical activity duratio,sleep quality,weight control,and PRO in hypertensive patients
统计指标 体力活动时长
(0 min作为参照)睡眠质量
(一般作为参照)体重控制
(不控制作为参照)0~30 min 30 min~1 h 1~2 h ≥2 h 好 差 运动 饮食 运动+饮食 其他方式 总人群 B
(95%CI)0.777
(−0.952,2.506)1.298
(−0.451,3.046)1.702
(−0.753,4.157)6.551
(2.611,10.491)1.870
(0.449,3.291)−0.665
(−2.539,1.209)2.216
(−0.073,4.505)−4.873
(−7.860,−1.887)1.904
(0.383,3.424)−7.105
(−12.211,−1.999)β 0.047 0.079 0.063 0.132 0.101 −0.027 0.073 −0.120 0.094 −0.102 P 0.378 0.146 0.174 0.001 0.010 0.486 0.058 0.001 0.014 0.006 男性 B
(95%CI)1.142
(−1.686,3.971)0.700
(−1.969,3.369)2.854
(−0.778,6.487)7.189
(0.828,13.550)2.487
(0.418,4.556)0.562
(−2.339,3.463)4.586
(1.036,8.136)−5.302
(−9.802,−0.802)2.963
(0.580,5.346)−8.302
(−15.104,−1.501)β 0.065 0.045 0.119 0.151 0.141 0.022 0.153 −0.142 0.147 −0.143 P 0.427 0.606 0.123 0.027 0.019 0.073 0.012 0.021 0.015 0.017 女性 B
(95%CI)0.963
(−1.296,3.222)2.346
(−0.055,4.748)1.803
(−1.594,5.199)7.782
(2.554,13.011)0.278
(−1.54,2.131)−2.478
(−4.684,−0.272)1.305
(−1.703,4.313)−3.902
(−8.044,0.239)1.944
(−0.015,3.903)−5.054
(−12.815,2.706)β 0.060 0.138 0.061 0.154 0.015 −0.107 0.043 −0.090 0.096 −0.062 P 0.402 0.055 0.297 0.004 0.768 0.028 0.394 0.065 0.052 0.201 中青年 B
(95%CI)3.151
(0.528,5.775)1.980
(−0.669,4.628)2.972
(−0.596,6.539)7.518
(3.014,12.023)2.289
(0.464,4.114)0.184
(−2.789,3.156)2.097
(−1.123,5.317)−4.638
(−8.632,−0.644)1.455
(−0.865,3.775)−5.987
(−14.083,2.110)β 0.190 0.113 0.111 0.209 0.137 0.007 0.074 −0.129 0.072 −0.082 P 0.019 0.142 0.102 0.001 0.014 0.903 0.201 0.022 0.218 0.147 老年 B
(95%CI)−1.079
(−3.381,1.223)0.639
(−1.699,2.978)1.012
(−2.363,4.387)11.717
(−3.106,26.539)0.383
(−1.724,2.491)−2.351
(−4.469,−0.232)2.513
(−0.758,5.784)−4.156
(−8.766,0.455)2.372
(0.380,4.365)−7.753
(−14.177,−1.329)β −0.070 0.043 0.040 0.094 0.019 −0.113 0.081 −0.093 0.123 −0.124 P 0.357 0.591 0.555 0.121 0.721 0.030 0.132 0.077 0.020 0.018 注:模型在校正年龄、性别、居住地、文化程度、经济状况、吸烟、饮酒、水果频率、睡眠质量、体力活动频率、体力活动方式(体重控制、睡眠质量或体力活动时长)的基础上校正了并发症、病程、服药情况、用药方式。 表 4 高血压患者睡眠质量、体重控制在体力活动时长及PRO间的中介效应分析
Table 4. Mediation effect analysis of sleep quality and weight control on the relationship between physical activity duration and PRO in hypertensive patients
变量 PRO PRO 体重控制 睡眠质量 B t P B t P B t P B t P 体力活动时长 1.081 3.596 < 0.001* 1.260 4.207 < 0.001* −0.237 −3.372 0.001* −0.061 −2.545 0.011* 睡眠质量 −1.710 −3.384 < 0.001* 体重控制 −0.315 −1.831 0.068 R2 0.118 0.095 0.023 0.046 F 15.924 21.087 4.705 9.546 *P < 0.05。 表 5 总效应、直接效应及中介效应分解表
Table 5. Total effect,direct effect,and mediation effect decomposition table
效应 效应值 Boot标准误 Boot(95%CI) 相对效应值% 总效应 1.260 0.300 (0.672,1.848) 100.00 直接效应 1.081 0.278 (0.537,1.617) 85.80 睡眠质量 0.104 0.058 (0.016,0.239) 8.27 体重控制 0.075 0.049 (−0.01,0.168) 5.93 注:Boot 标准误、Boot CI 下限和 Boot CI 上限分别指通过偏差矫正的百分位 Bootstrap 法估计的间接效应的标准误差、95% 置信区间的下限和上限。 -
[1] Desai A N. High Blood Pressure[J]. JAMA,2020,324(12):1254-1255. doi: 10.1001/jama.2020.11289 [2] Li Z,Cao L M,Zhou Z Y,et al. Factors influencing the progression from prehypertension to hypertension among Chinese middle-aged and older adults: A 2-year longitudinal study[J]. BMC Public Health,2023,23(1):339. doi: 10.1186/s12889-022-14410-3 [3] US Food and Drug Administration. Guidance for industry: Patient-reported outcome measures: Use in medical product development to support labeling claims: draft guidance [J]. Health and Quality of Life Outcomes,2006,4 (1): 79. [4] 厉柯轩,蔡媛媛,谢舒,等. 我国患者报告结局研究热点分析[J]. 中华护理教育,2023,20(9):1113-1118. [5] 史钊,窦蕾,李顺平. 国内外患者报告结局的应用现状与研究进展[J]. 中国全科医学,2023,26(4):401-408. [6] 彭丽霞,张勇. 高血压患者报告结局的研究现状[J]. 保健医学研究与实践,2021,18(1):100-104. doi: 10.11986/j.issn.1673-873X.2021.01.023 [7] 李明哲,田一川,王成龙,等. 身体活动和睡眠对中老年人腰背痛的独立和联合影响研究[J]. 中国全科医学,2024,27(23):2869-2874. [8] Zhou L L,Feng W,Xiang N,et al. Association between physical activity dimensions and the risk of hypertension among middle and older adults: A cross-sectional study in China[J]. Frontiers in Public Health,2022,10:995755. doi: 10.3389/fpubh.2022.995755 [9] Byambasukh O,Snieder H,Corpeleijn E. Relation between leisure time,commuting,and occupational physical activity with blood pressure in 125 402 adults: The lifelines cohort[J]. Journal of the American Heart Association,2020,9(4):e014313. doi: 10.1161/JAHA.119.014313 [10] Koh Y S,Asharani P V,Devi F,et al. Benefits of leisure-related physical activity and association between sedentary time and risk for hypertension and type 2 diabetes[J]. Annals of the Academy of Medicine,Singapore,2023,52(4):172-181. [11] 唐顺定. 高血压患者报告的临床结局研究及MCID制定 [D]. 昆明: 昆明医科大学,2021. [12] 中国高血压防治指南(2018年修订版) [J]. 中国心血管杂志,2019,24(1): 24-56. [13] Tofighi B,Abrantes A,Stein M D. The role of technology-based interventions for substance use disorders in primary care: A review of the literature[J]. Med Clin North Am,2018,102(4):715-731. doi: 10.1016/j.mcna.2018.02.011 [14] Patel M L,Hopkins C M,Brooks T L,et al. Comparing self-monitoring strategies for weight loss in a smartphone app: Randomized controlled trial[J]. JMIR Mhealth Uhealth,2019,7(2):e12209. doi: 10.2196/12209 [15] Payne R S,Piernas C,Aveyard P,et al. A mobile health salt reduction intervention for people with hypertension: Results of a feasibility randomized controlled trial[J]. JMIR Mhealth Uhealth,2021,9(10):e26233-e26233. doi: 10.2196/26233 [16] 唐顺定,万崇华,宋莹,等. 高血压患者报告的临床结局测定量表的应用考评[J]. 昆明医科大学学报,2022,43(3):60-66. [17] 许珊,张书迎,谢文涵,等. 生活方式与心血管代谢性共病发生发展轨迹的关联研究[J]. 现代预防医学,2024,51(12):2113-2120. [18] Montoya A K, Hayes A F. Two-condition within-participant statistical mediation analysis: A path-analytic framework[J]. Psychol Methods,2017,22(1):6-27. [19] Hiroshi K,Tatsuhiko A,Ayano T,et al. Features of and preventive measures against hypertension in the young[J]. Hypertension Research,2019,42(7):935-948. doi: 10.1038/s41440-019-0229-3 [20] Andi A,Edi P,Lukman N. The correlation between body mass index,physical activity and blood pressure with quality of life in elderly hypertension[J]. Formosa Journal of Science and Technology,2023,2(5):1191-1214. doi: 10.55927/fjst.v2i5.4021 [21] Eliana R M,Beatriz N. Physical activity and its relationship with health-related quality of life in type II diabetics[J]. Exercise and Quality of Life,2022,14(2):5-12. doi: 10.31382/eqol.221201 [22] 唐颖,覃玲玉,吕高名,等. 基于行为改变整合理论的健康教育对老年高血压患者血压控制及生命质量的影响[J]. 河北医药,2024,46(21):3346-3349. [23] 罗晓梅. 宁夏吴忠扁担沟镇高血压患者的控制率及相关影响因素分析 [D]. 宁夏:宁夏医科大学,2021. [24] Neto O L ,Tavares O D D V ,Nascimento D P A Â,et al. Analysis of the levels of physical activity in the quality of life of elderly patients with hypertension[J]. Global Journal of Health Science,2020,12(4):138. [25] Wu W W,Wang W R,Gu Y H,et al. Sleep quality,sleep duration,and their association with hypertension prevalence among low-income oldest-old in a rural area of China: A population-based study[J]. Journal of Psychosomatic Research,2019,127(12):109848. [26] 张艳平. 观察老年高血压患者睡眠时间及睡眠质量与血压变异性的相关性[J]. 世界睡眠医学杂志,2022,9(5):833-835. doi: 10.3969/j.issn.2095-7130.2022.05.017 [27] 孙尧,郑明明,程燕. 高龄高血压患者血压达标情况及影响因素分析[J]. 中国循证心血管医学杂志,2016,8(4):448-450. [28] Thalia W,Andriana K D. Poor sleep quality in post menopause woman[J]. Science Midwifery,2023,11(1):76-84. doi: 10.35335/midwifery.v11i1.1197 [29] Izabella U,Karolina H. M,Bartosz U,et al. The relationship between sleep disturbances and quality of life in elderly patients with hypertension [J]. Clinical Interventions in Aging,2019,14:155-165. [30] 王洪丹. 老年人睡眠、体力活动对健康的影响研究 [D]. 吉林: 吉林大学,2023. [31] Barbagelata A F.,Vizcarra E D. Quality of life is impaired among older adults with obstructive sleep apnea hypopnea syndrome despite disease severity[J]. Sleep Medicine,2013,14(S1):e300-e300. [32] Hossein S,Amir S. Sleep-related breathing disorders and quality of life[J]. Sleep Medicine Clinics,2006,1(4):519-525. doi: 10.1016/j.jsmc.2006.10.003 [33] Signal T L,Gale J,Gander P H. Sleep measurement in flight crew: Comparing actigraphic and subjective estimates to polysomnography[J]. Aviation,Space,and Environmental Medicine,2005,76(11):1058-1063. [34] Lauderdale D S,Knutson K L,Yan L L,et al. Self-reported and measured sleep duration: how similar are they?[J]. Epidemiology (Cambridge,Mass. ),2008,19(6):838-845. doi: 10.1097/EDE.0b013e318187a7b0 [35] 郑柳燕,徐兴燕,蔡莹莹,等. 福州市社区居民睡眠特征与正常高值血压的关系[J]. 中华高血压杂志,2023,31(3):264-272. [36] 张莉,郭奕瑞,杨艳,等. 健康体检人群运动与睡眠质量的关系[J]. 江苏医药,2022,48(1):56-60. -







 下载:
下载:

 下载:
下载: 
