Effect of Ulinastatin Combined with Continuous Renal Replacement Therapy in Treatment of Severe Burn Patients and Its Influence on Inflammatory Factors and 28-day all-cause Mortality
-
摘要:
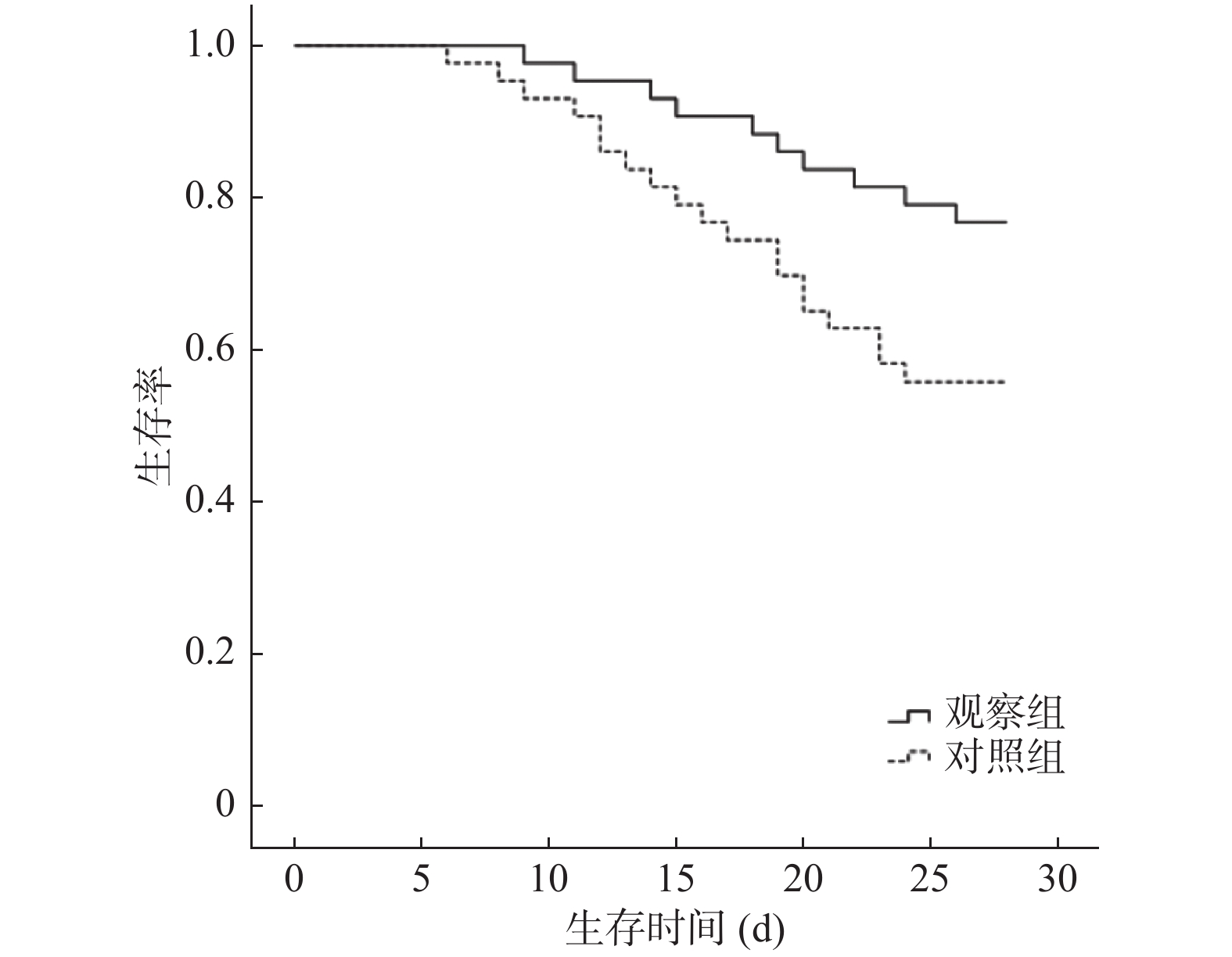
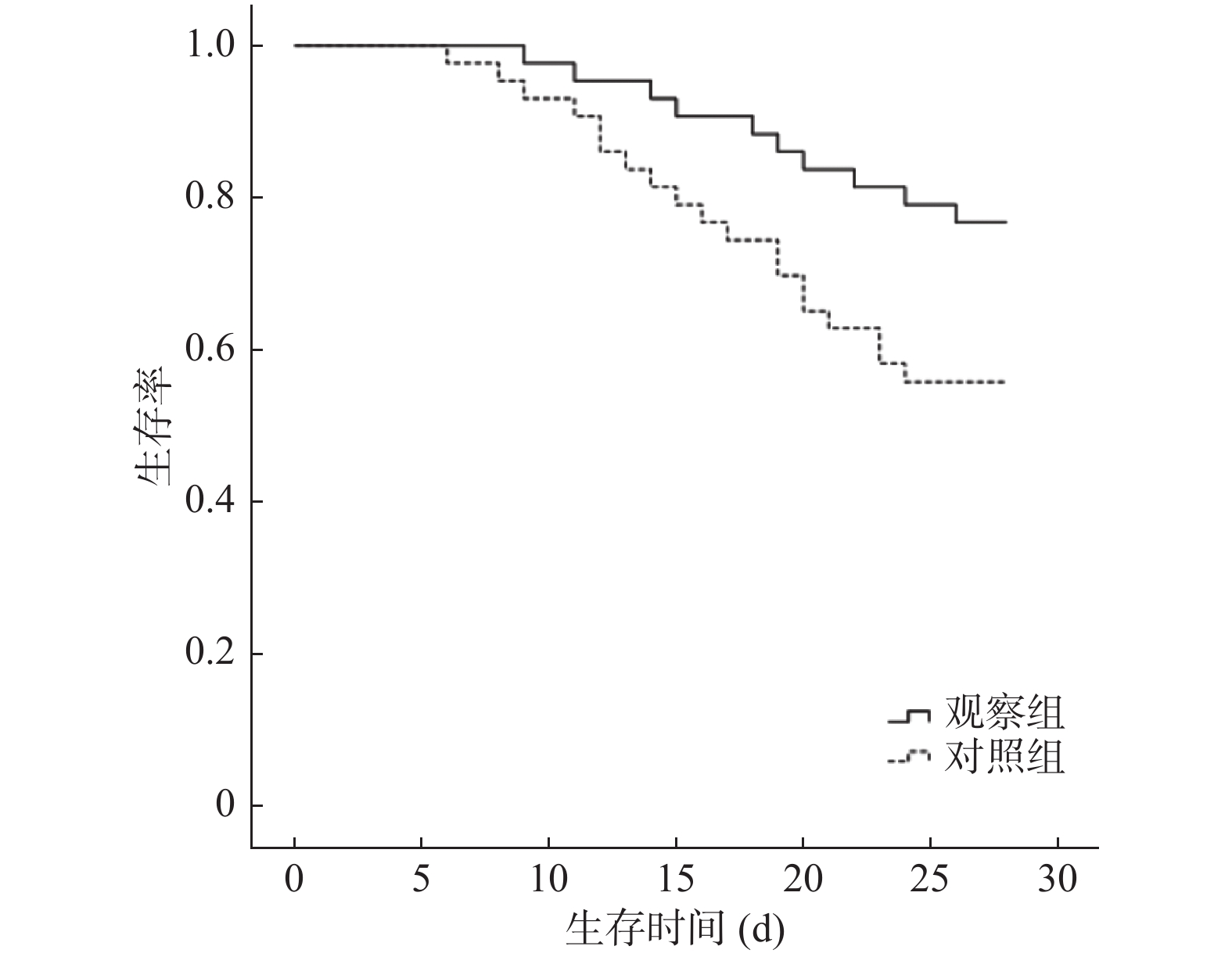
目的 探讨乌司他丁联合连续性肾脏替代疗法(CRRT)治疗重症烧伤对炎症因子、28 d全因死亡率的影响。 方法 选取昆明医科大学第二附属医院2017年1月至2019年8月收治的重症烧伤患者86例,按随机数表法分为CRRT组与乌司他丁联合CRRT组,每组43例。CRRT组:常规治疗+CRRT,乌司他丁联合CRRT组:在CRRT组基础上联合乌司他丁,连续7 d。比较两组治疗前、治疗7 d后的危重评分(APACHEⅡ评分、SOFA评分、Marshall评分)、血清炎症因子(TNF-α、IL-6、IL-8)、抗生素和血管活性药物的使用时间、机械通气时间及28 d全因死亡率。绘制Kaplan-Meier生存曲线分析两组患者的28 d生存情况。 结果 治疗前,两组患者的APACHEⅡ评分、SOFA评分、Marshall评分的差异无统计学意义(P > 0.05)。两组患者治疗7 d后的各项评分均明显低于治疗前(P < 0.05)。乌司他丁联合CRRT组患者治疗7 d后的APACHEⅡ评分、SOFA评分、Marshall评分显著低于CRRT组(P < 0.05)。治疗前,两组患者血清TNF-α、IL-6、IL-8的差异无统计学意义(P > 0.05)。治疗7 d后,两组患者血清TNF-α、IL-6、IL-8均低于治疗前(P < 0.05)。乌司他丁联合CRRT组患者治疗7 d后的血清TNF-α、IL-6、IL-8显著低于CRRT组(P < 0.05)。乌司他丁联合CRRT组和CRRT组的28 d全因死亡率的比较差异有统计学意义(23.26% vs 44.19%,P < 0.05)。 结论 乌司他丁联合CRRT治疗重度烧伤患者可降低APACHEⅡ、SOFA及Marshall评分、血清TNF-α、IL-6、IL-8水平及28 d全因死亡率,缩短治疗时间,有效性和安全性较高。 Abstract:Objective To explore the effect of ulinastatin combined with continuous renal replacement therapy(CRRT)on inflammatory factors and 28-day all-cause mortality in severe burns. Methods A selection of 86 patients with severe burns admitted to the Second Affiliated Hospital of Kunming Medical University from January 2017 to August 2019 were divided into CRRT group and Ulinastatin combined CRRT group according to the random number table, with 43 cases in each group. CRRT group: conventional treatment + CRRT, ulinastatin combined with CRRT group: combined with ulinastatin on the basis of CRRT group for 7 consecutive days. Compare the critical scores(APACHEⅡ score, SOFA score, Marshall score), serum inflammatory factors(TNF-α, IL-6, IL-8), antibiotics and vasoactive drugs before treatment and 7 days after treatment between the two groups. The duration of mechanical ventilation and 28-day all-cause mortality. The Kaplan-Meier survival curve was drawn to analyze the 28-day survival of the two groups of patients. Results Before treatment, there was no significant difference in APACHEⅡ, SOFA, and Marshall scores between the two groups of patients(P > 0.05). The scores of the two groups of patients after 7 days of treatment were significantly lower than those before treatment(P < 0.05). The APACHEⅡ, SOFA, and Marshall scores of the patients in the Ulinastatin combined CRRT group were significantly lower than those in the CRRT group after 7 days of treatment(P < 0.05). Before treatment, the differences in serum TNF-α, IL-6 and IL-8 between the two groups were not statistically significant(P > 0.05). After 7 days of treatment, serum TNF-α, IL-6 and IL-8 of the two groups were lower than before treatment(P < 0.05). The serum TNF-α, IL-6 and IL-8 of patients in the ulinastatin combined CRRT group were significantly lower than those in the CRRT group after 7 days of treatment(P < 0.05). There was a statistically significant difference in 28-day all-cause mortality between the ulinastatin combined CRRT group and the CRRT group(23.26% vs 44.19%, P < 0.05). Conclusion Ulinastatin combined with CRRT in the treatment of severe burn patients can reduce APACHEⅡ, SOFA and Marshall scores, serum TNF-α, IL-6, IL-8 levels and 28-day all-cause mortality, shorten the treatment time, and have better efficacy and high safety. -
表 1 两组基线资料比较(
$\bar x \pm s$ )Table 1. Comparison of baseline data between the two groups(
$\bar x \pm s$ )组别 n 性别(男/女) 年龄(岁) 烧伤至入院时间(h) 烧伤面积(%) Ⅱ度 Ⅲ度 乌司他丁联合CRRT组 43 25/18 46.57 ± 8.49 4.35 ± 1.41 39.89 ± 7.68 15.32 ± 2.74 CRRT组 43 23/20 48.73 ± 7.84 3.99 ± 1.25 40.41 ± 8.33 14.98 ± 2.59 χ2/t 0.189 1.226 1.253 0.301 0.591 P 0.664 0.224 0.214 0.764 0.556 表 2 两组APACHEⅡ评分、SOFA评分、Marshall评分比较[(
$\bar x \pm s$ ),分]Table 2. Comparison of APACHEⅡ,SOFA and Marshall scores between the two groups[(
$\bar x \pm s$ ),points]组别 n APACHEⅡ评分 SOFA评分 Marshall评分 治疗前 治疗7 d 治疗前 治疗7 d 治疗前 治疗7 d 乌司他丁联合CRRT组 43 32.98 ± 4.43 19.46 ± 2.63* 11.85 ± 2.29 7.38 ± 1.60* 12.02 ± 2.10 6.75 ± 1.94* CRRT组 43 33.08 ± 4.76 22.02 ± 2.81* 12.14 ± 2.53 9.08 ± 1.91* 11.88 ± 2.04 8.22 ± 2.09* t 0.101 4.362 0.557 4.474 0.314 3.380 P 0.920 0.001 0.579 0.000 0.755 0.001 与治疗前相比,*P < 0.05。 表 3 两组血清TNF-α、IL-6、IL-8的比较(
$\bar x \pm s$ )Table 3. Comparison of serum TNF-α,IL-6 and IL-8 between the two groups(
$\bar x \pm s$ )组别 n TNF-α(μg/mL) IL-6(pg/mL) IL-8(pg/mL) 治疗前 治疗7 d 治疗前 治疗7 d 治疗前 治疗7 d 乌司他丁联合CRRT组 43 3.30 ± 0.59 1.24 ± 0.34* 22.27 ± 3.99 8.78 ± 2.36* 2.29 ± 0.49 1.11 ± 0.35* CRRT组 43 3.33 ± 0.55 1.49 ± 0.30* 22.58 ± 4.14 10.54 ± 2.55* 2.35 ± 0.52 1.45 ± 0.39* t 0.244 3.615 0.398 3.222 0.551 4.255 P 0.808 0.001 0.692 0.001 0.583 0.001 与治疗前相比,*P < 0.05。 表 4 两组患者治疗相关指标的比较[(
$\bar x \pm s$ ),d]Table 4. Comparison of treatment-related indicators between the two groups[(
$\bar x\pm s$ ),d]组别 n 抗生素使用时间 血管活性药物使用时间 机械通气时间 乌司他丁联合CRRT组 43 8.47 ± 1.96 4.86 ± 0.89 5.65 ± 1.77 CRRT组 43 9.52 ± 2.34 6.01 ± 1.53 6.88 ± 1.90 t 2.266 3.256 3.106 P 0.027* 0.002* 0.003* *P < 0.05。 -
[1] 唐洪泰,朱峰. 危重烧伤后的急性应激反应[J].中华烧伤杂志,2017,33(11):657-659. doi: 10.3760/cma.j.issn.1009-2587.2017.11.001 [2] 黄兆丹,周姓良,陈燕河,等. 双机换管法对连续性肾脏替代治疗患者上机血流动力学的影响[J].昆明医科大学学报,2018,39(9):65-68. [3] Liu W,Chai J K. Influences of ulinastatin on acute lung injury and time phase changes of coagulation parameters in rats with burn-blast combined injuries[J]. Chin J burns,2018,34(1):32-39. [4] Zhang X,Zhu Z,Jiao W,et al. Ulinastatin treatment for acute respiratory distress syndrome in China:a meta-analysis of randomized controlled trials[J]. BMC Pulm Med,2019,19(1):196-199. doi: 10.1186/s12890-019-0968-6 [5] He F,Song Y,Ying W J,et al. Effects of Ulinastatin on myocardial oxidative stress and inflammation in severely burned rats[J]. Eur Rev Med Pharmacol Sci,2018,22(17):5719-5728. [6] Otsuki K,Kawabata I,Matsuda Y,et al. Randomized trial of the efficacy of intravaginal ulinastatin administration for the prevention of preterm birth in women with a singleton pregnancy and both cervical shortening and inflammation of lower genital tract[J]. J Obstet Gynaecol Res,2019,45(1):86-95. doi: 10.1111/jog.13796 [7] 程晓迎,王磊. APACHEⅡ评分联合尿中性粒细胞明胶酶相关载脂蛋白检测对脓毒症合并急性肾损伤的预测价值[J].临床误诊误治,2020,33(6):57-62. doi: 10.3969/j.issn.1002-3429.2020.06.014 [8] 吴燕丽,邢柏. 序贯器官衰竭评估评分对脓毒症患者红细胞输注的预测价值[J].中国急救医学,2019,39(10):987-991. doi: 10.3969/j.issn.1002-1949.2019.10.014 [9] 赵鹏飞,付小萌,王超,等. 多器官功能障碍综合征诊断标准及评分系统现状[J].临床和实验医学杂志,2013,12(8):630-636. doi: 10.3969/j.issn.1671-4695.2013.08.032 [10] 王树英. 脂肪干细胞移植联合乌司他丁对急性肠缺血再灌注损伤的影响[J].中国组织工程研究,2018,22(29):4601-4606. doi: 10.3969/j.issn.2095-4344.0995 [11] 穆盛田,唐洁,阎东莉,等. 乌司他丁通过抑制氧化应激反应改善TNF-α引起的人肺微血管内皮细胞屏障功能障碍[J].中国医科大学学报,2020,49(1):52-57. [12] 郭远波,王研,张登文,等. 乌司他丁对异氟烷介导的大鼠海马神经元凋亡的影响[J].南方医科大学学报,2019,39(7):850-854. [13] 王东,徐岚,谈鹰,等. 乌司他丁对感染性休克患者的脏器保护作用及感染标志物的影响研究[J].中华医院感染学杂志,2017,27(7):1474-1476. [14] Li S,Yang W,Zhou L,et al. Vascular permeability and hemodynamic effects of ulinastatin on organs affected by shock during early burn injury[J]. Am J Emerg Med,2019,37(2):249-253. doi: 10.1016/j.ajem.2018.05.038 [15] Rhodes A,Evans L E,Alhazzani W,et al. Surviving sepsis campaign:International guidelines for management of sepsis and septic shock:2016[J]. Intensive Care Med,2017,43(3):304-377. doi: 10.1007/s00134-017-4683-6 -





 下载:
下载: