Effect of Osteoking on Bone Density and Bone Biomechanics of Tree Shrews in a Postmenopausal Osteoporotic Fracture Model
-
摘要:
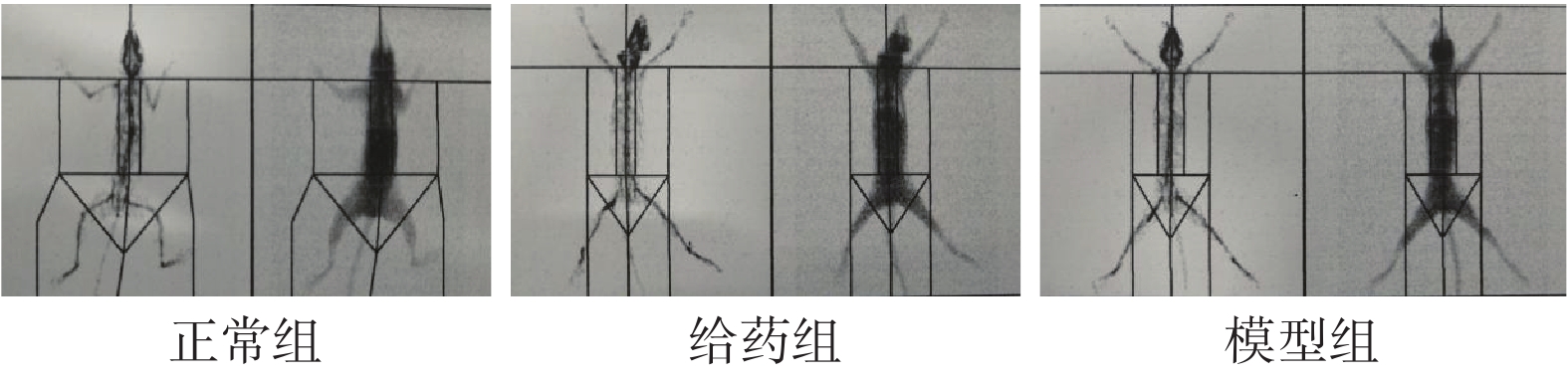
目的 研究恒古骨伤愈合剂对绝经后骨质疏松性骨折(OPF)模型树鼩骨密度及骨生物力学的影响。 方法 雌性滇西亚种树鼩双侧卵巢及子宫切除术建立骨质疏松(OP)模型,180 d后,对树鼩进行骨密度(BMD)测定,将20只OP模型造模成功的树鼩随机平均分为给药组(3 mL/kg)、模型组(等体积0.9%氯化钠溶液)。10只仅切除同体积大网膜树鼩分为正常组(等体积0.9%氯化钠溶液)。将给药组和模型组树鼩进行右侧后肢胫骨骨折术建立OPF模型。给药组每2天给药1次,连续给药90 d,其余组给予同剂量的生理盐水。处死树鼩后,进行双能X射线吸收法检测实验以及股骨三点弯曲实验。 结果 与正常组比较,给药组和模型组全身(含头部)、腰 + 盆骨、颈椎-尾椎、左骨盆、右骨盆、腰椎、腰 + 骶骨、全身(不含头部)BMD均有不同程度显著降低,差异有统计学意义(P < 0.05);与模型组比较,给药组全身(含头部)、腰 + 盆骨、颈椎-尾椎、左骨盆、腰椎、腰 + 骶骨BMD均有显著提升,差异有统计学意义(P < 0.05),而右骨盆、全身(不含头部)BMD无统计学差异( P > 0.05)。骨生物力学方面,与正常组相比,给药组能量吸收能力显著提升,而最大载荷和结构刚度无统计学差异( P > 0.05);模型组最大载荷、结构刚度、能量吸收能力均有显著降低,差异均有统计学意义(P < 0.05);与给药组相比,模型组最大载荷、结构刚度、能量吸收能力均有显著降低,差异均有统计学意义(P < 0.05)。 结论 恒古骨伤愈合剂对OPF模型树鼩的BMD和骨生物力学方面均有改善作用。 Abstract:Objective To observe the effect of osteoking on bone density and bone biomechanics in a postmenopausal osteoporotic fracture(OPF)model tree shrew. Methods Female western Yunnan subspecies tree shrews were subjected to bilateral ovariectomy and hysterectomy to establish an osteoporosis(OP)model, and after 180 days, bone density(BMD)was measured in tree shrews, and 20 OP modeling successes were randomly and equally divided into administration(3 mL/kg)and model groups(equal volume of 0.9% sodium chloride solution). Ten tree shrews with the same volume of large omentum removed were divided into normal groups(equal volume of 0.9% sodium chloride solution). The tree shrews in the drug-administered and model groups were subjected to right hindlimb tibial fracture surgery to establish the OPF model. The administration group was given one dose of saline every 2 d for 90 d, and the remaining group was given the same dose of saline. Results Compared with the normal group, the BMD of whole body(including head), lumbar + pelvic, cervical-caudal, left pelvis, right pelvis, lumbar spine, lumbar + sacral, and whole body(excluding head)were significantly reduced to different degrees in the administered and model groups, and the differences were statistically significant(P < 0.05). Compared with the model group, the BMD of the whole body(including the head), lumbar + pelvic, cervical-caudal, left pelvis, lumbar spine, and lumbar + sacral were significantly increased in the administration group, and the differences were statistically significant(P < 0.05), while the BMD of the right pelvis and whole body(excluding the head)were not statistically different. In terms of bone biomechanics, energy absorption was significantly increased in the administered group compared to the normal group, while maximum load and structural stiffness were not statistically difference; the maximum load, structural stiffness, and energy absorption capacity of the model group were all significantly reduced, and the differences were statistically significant(P < 0.05). The maximum load, structural stiffness, and energy absorption capacity of the model group were all significantly reduced compared to the drug-administered group, and the differences were statistically significant(P < 0.05). Conclusion Osteoking can improve both BMD and bone biomechanics in the OPF model of tree shrew. -
Key words:
- Osteoking /
- Tree shrew /
- Osteoporosis /
- Bone density /
- Bone biomechanics
-
表 1 各组树鼩骨密度比较结果[(
$\bar x \pm s$ ),g/cm2]Table 1. Comparison of bone density of tree shrews in each group[(
$\bar x \pm s$ ),g/cm2]区域 正常组(n = 10) 给药组( n = 10) 模型组( n = 10) 全身(含头部) 0.103 ± 0.012 0.097 ± 0.005* 0.087 ± 0.005**.# 腰 + 盆骨 0.097 ± 0.004 0.088 ± 0.003** 0.083 ± 0.004**.# 颈椎−尾椎 0.096 ± 0.003 0.084 ± 0.004** 0.078 ± 0.005**.## 左骨盆 0.099 ± 0.011 0.087 ± 0.006** 0.082 ± 0.004**.# 右骨盆 0.098 ± 0.005 0.091 ± 0.004* 0.088 ± 0.005** 腰椎 0.096 ± 0.002 0.090 ± 0.004** 0.083 ± 0.005**.# 腰 + 骶骨 0.093 ± 0.006 0.087 ± 0.004* 0.081 ± 0.005**.# 全身(不含头部) 0.092 ± 0.003 0.084 ± 0.004* 0.082 ± 0.004** 与正常组比较,*P < 0.05,**P < 0.01;与给药组比较,#P < 0.05,##P < 0.01。 表 2 各组树鼩骨生物力学特性统计分析结果[(
$\bar x \pm s$ ),n = 10]Table 2. Results of statistical analysis of the biomechanical properties of tree shrew bone in each group[(
$\bar x \pm s$ ),n = 10]项目 正常组 给药组 模型组 最大载荷(N) 50.13 ± 7.75 47.75 ± 4.43 41.31 ± 4.43**.## 结构刚度(N/mm) 72.52 ± 19.76 76.63 ± 6.42 53.18 ± 7.99**.## 能量吸收能力(N/mm) 53.64 ± 12.21 59.95 ± 9.81* 41.52 ± 8.32**.## 与正常组比较,*P < 0.05,**P < 0.01;与给药组比较,##P < 0.01。 -
[1] Cheng C,Wentworth K,Shoback D M. New frontiers in osteoporosis therapy[J]. Annual Review of Medicine,2020,71(1):277-288. doi: 10.1146/annurev-med-052218-020620 [2] Body J J. How to manage postmenopausal osteoporosis?[J]. Acta Clinica Belgica,2011,66(6):443-447. [3] 崔伟,刘成林. 基础骨生物力学(一)[J].中国骨质疏松杂志,1997,3(04):82-85. [4] 王运林,匡德宣,马朝霞,等. 去卵巢法骨质疏松树鼩模型的建立[J].中国实验动物学报,2015,23(06):562-566. doi: 10.3969/j.issn.1005-4847.2015.06.003 [5] Fan Y,Huang Z Y,Cao C C,et al. Genome of the Chinese tree shrew[J]. Nature Communications,2013,4(2):66-78. [6] 贾杰,代解杰. 树鼩在生物医学研究中的优势与挑战[J].实验动物与比较医学,2019,039(001):3-8. [7] 武羽洁,袁鑫,角建林,等. 两种方法建立树鼩骨质疏松模型的比较实验研究[J].医学研究杂志,2019,48(08):51-54. [8] 吴婷婷,屈会化,胡丽娜,等. 基于树鼩体表面积的树鼩与人类及其它实验动物等效剂量换算系数的测算[J].中华中医药杂志,2015,30(01):203-205. [9] Sipos W,Pietschmann P,Rauner M,et al. Pathophysiology of osteoporosis[J]. Wiener Medizinische Wochenschrift,2009,159(9-10):230-234. doi: 10.1007/s10354-009-0647-y [10] 李凤山,李恩,张晓晴,等. 补肾方药对去卵巢大鼠骨灰重和骨生物力学影响的实验研究[J].内蒙古中医药,2017,36(16):129-130. doi: 10.3969/j.issn.1006-0979.2017.16.128 [11] Labbe E N,Symes S A,Raymond D E,et al. The Rorschach butterfly,understanding bone biomechanics prior to using nomenclature in bone trauma interpretations[J]. Forensic Science International,2019,299(04):187-194. [12] 邸倩,邱明才,张鑫,等. 吡格列酮对链脲佐菌素诱导的糖尿病大鼠骨生物力学性能的影响[J].山西医科大学学报,2017,48(09):926-929. [13] 孙岩,陈冉,王小琦,等. 恒古骨伤愈合剂对去势雌性大鼠骨质疏松模型的影响[J].中国骨质疏松杂志,2016,22(12):1513-1515+1539. doi: 10.3969/j.issn.1006-7108.2016.12.003 [14] Dai L,Wu H,Yu S,et al. Effects of osteoking on osteoporotic rabbits[J]. Molecular Medicine Reports,2015,12(1):1066-1074. doi: 10.3892/mmr.2015.3551 [15] 张慧杰,王小琦,孙岩,等. 恒古骨伤愈合剂初步分离及其促骨形成活性的评价[J].中华中医药杂志,2018,33(04):1512-1515. [16] 郑红,李进涛,赵宏斌,等. 恒古骨伤愈合剂促进骨细胞增殖缓解骨质疏松症树鼩的分子机制[J].中药药理与临床,2017,33(04):133-136. [17] 王素彬,赵宏斌,胡敏,等. 恒古骨伤愈合剂对骨质疏松性骨折兔骨密度及DKK-1蛋白的影响[J].中国中西医结合杂志,2015,35(08):1000-1003. doi: 10.7661/CJIM.2015.08.1000 [18] 蒙锡波,邓丽丽. 恒古骨伤愈合剂联合活血补肾汤治疗激素性股骨头坏死疗效及对骨密度的影响[J].现代中西医结合杂志,2018,27(01):82-85. [19] 袁鑫,武羽洁,角建林,等. 彝药恒古骨伤愈合剂的药理作用和临床应用[J].中国现代应用药学,2019,36(03):372-376. [20] 赵宏斌,胡敏,王维琦,等. 恒古骨伤愈合剂对激素性坏死股骨头内VEGF基因表达的影响[J].中国骨伤,2007,20(11):757-759. [21] 吴建飞,占日新. 恒古骨伤愈合剂对兔骨折愈合的影响[J].临床合理用药杂志,2017,10(27):13-14. -






 下载:
下载: