Value of Fragmented QRS in Predicting Prognosis of Patients after Cardiac Resynchronization Therapy
-
摘要:
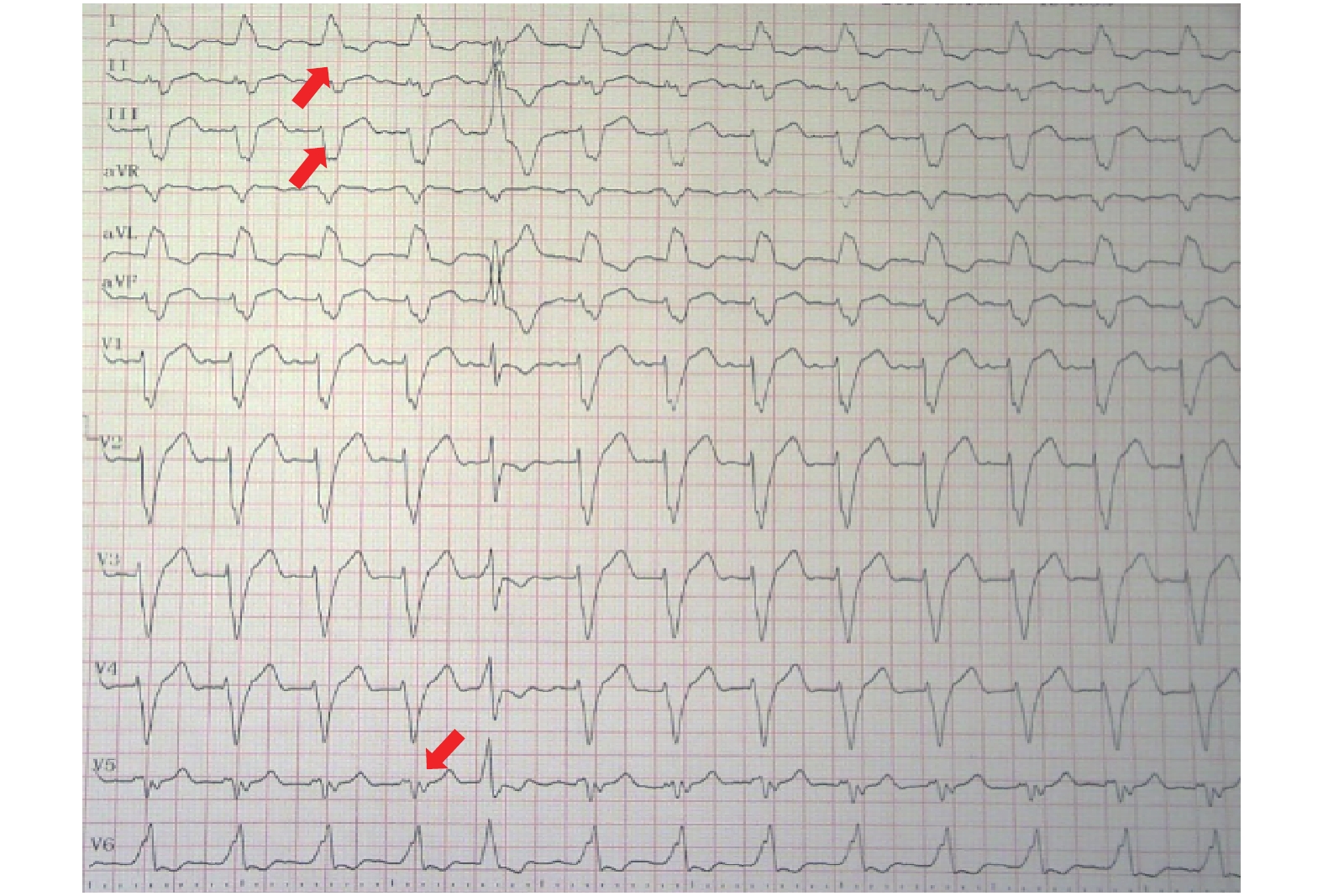
目的 研究CRT植入前后碎裂QRS(fragmented QRS,fQRS)特征与CRT应答之间的关系。 方法 纳入2016年1月至2018年12月昆明医科大学第一附属医院心脏内科接受CRT植入的心力衰竭患者,分别采集患者CRT植入前和植入后6个月的12导联心电图及超声心动图图像并分析其与CRT应答的关系。 结果 研究纳入108例患者(其中男性78例,占总人数的72.2%),平均年龄(56.5±11.9)岁。共有75例患者(69.4%)对CRT有应答,左室射血分数显著增加[从(30.71±1.92)~(50.61±2.57),P < 0.001],左室舒张末容积显著(LVESV)降低[从(195.26±78.79)~(156.55±84.44), P < 0.001]。CRT植入后,有应答患者心电图中有fQRS导联的数量未改变[CRT植入前后分别为(6.25±2.68) vs (6.03±2.54), P= 0.571],无应答者心电图中fQRS导联数量显著增加[CRT植入前后分别为(6.18±2.20) vs (7.36±2.61),P= 0.013]。多因素Logistic分析显示,QRS时限的降低和CRT植入后fQRS导联数量的减少是CRT应答的独立预测因子。 结论 CRT植入后含fQRS导联的数量增加是CRT无应答的独立预测因子,除QRS宽度及形态以外的心电图特征有助于评估在心力衰竭患者是否适合接受CRT植入。 Abstract:Objestive To investigate the association between characteristics of Fragmented QRS(fQRS)before and after CRT implantation and response to CRT. Methods Patients with heart failure planned for CRT were enrolled. The 12-lead ECGs before and after CRT were analyzed. The presence of fQRs was confirmed according to the definition in previous studies. Echocardiography imagines were obtained before and 6 months after the CRT implantation. Results The study included 108 patients(78 male, 72.2%)with a mean age of 56.5 ± 11.9 years. Totally 75 patients(69.4%)responded to CRT with significantly increased mean LVEF(from 30.71±1.92 to 50.61±2.57, P < 0.001)and decreased LVESV(from 195.26±78.79 to 156.55±84.44, P < 0.001). After CRT implantation, the number of leads with fQRS remained unchanged in responders(6.25±2.68 vs. 6.03±2.54, P= 0.57 before and after CRT respectively)but increased in non-responders(6.18±2.20 vs.7.36±2.61, P = 0.013 before and after CRT respectively). In the multivariate logistic analysis, a decreased number of leads with fQRS and shortened QRS duration immediately after CRT implantation was found to be a predictor of response to CRT. Conclusions In patients undergoing CRT, new fQRS as well as an increased number of leads with fQRS in 12-lead ECG immediately after CRT implantation predicts non-response to CRT and may help in the decision making in heart failure patients. -
Key words:
- Cardiac resynchronization therapy /
- Fragmented QRS /
- Non-response
-
表 1 患者基线情况(
$\bar x \pm s$ )Table 1. Baseline characteristics of study population(
$\bar x \pm s$ )项目 数值 年龄(岁) 56.5 ± 11.9 男性[n(%)] 78(72.2) 缺血性疾病[n(%)] 21(19.4) 高血压[n(%)] 31(28.7) 糖尿病[n(%)] 23(21.3) 房颤[n(%)] 9(8.3) 药物[n(%)] RAS抑制剂 105(97.2) β受体阻滞剂 104(96.3) MCRA 95(88.0) RAS:肾素-血管紧张素系统;MCRA:盐皮质激素受体拮抗剂。 表 2 根据CRT应答情况分组患者基线特征比较(
$\bar x \;\pm\; s$ )Table 2. Baseline characteristic of CRT patients according to response of CRT(
$\bar x \;\pm \;s$ )项目 有应答者(n = 75) 无应答者(n = 33) χ2/t P 男性[n(%)] 57(76.0) 21(63.6) 1.746 0.186 年龄(岁) 57.44 ± 11.29 54.45 ± 13.32 1.201 0.232 缺血性心肌病 9(12.0) 12(36.3) 8.684 0.003* LBBB 42(56.0) 18(54.5) 0.020 0.889 QRS宽度(ms) 157.32 ± 26.71 153.82 ± 22.30 0.658 0.512 NYHA[n(%)] 0.631 0.427 II 28(37.5) 15(45.5) III-IV 47(62.5) 18(54.5) LVEDD(mm) 70.64 ± 9.06 69.27 ± 6.17 0.789 0.432 LAD(mm) 44.72 ± 8.47 42.82 ± 4.64 1.210 0.229 LVEF(%) 30.68 ± 8.06 28.82 ± 8.27 1.086 0.282 LVESV(mL) 199.28 ± 85.53 187.18 ± 50.63 0.755 0.452 LVEDV(mL) 289.76 ± 95.17 261.45 ± 64.53 1.556 0.123 fQRS导联数目 5.76 ± 2.99 6.18 ± 2.20 0.728 0.469 LBBB:左束支传导阻滞;NYHA:纽约心功能分级;LVEDD:左心室舒张末期内径;LVESD:左心室收缩末期内径;LAD:左心房内径;LVEF:左心室射血分数;LVESV:左心室收缩末期容积;LVEDV:左心室舒张末期容积。*P < 0.05。 表 3 CRT前后超声心动图和心电图参数的比较(
$\bar x \;\pm \;s$ )Table 3. Comparison of echocardiographic and electrographic parameters before and after CRT(
$\bar x\; \pm \;s$ )指标 有应答 无应答 之前 之后 P 之前 之后 P LVEF(%) 30.71 ± 1.92 50.61 ± 2.57 < 0.001* 28.83 ± 1.27 26.28 ± 1.55 0.005* LVESV(mL) 195.26 ± 78.79 156.55 ± 84.44 < 0.001* 187.18 ± 50.63 214.73 ± 64.38 < 0.001* QRS宽度(ms) 162.09 ± 22.09 145.87 ± 22.30 < 0.001* 153.82 ± 22.30 164.64 ± 22.22 0.036* 有fQRS的导联数目 6.25 ± 2.68 6.03 ± 2.54 0.571 6.18 ± 2.20 7.36 ± 2.61 0.013* 采用配对t检验比较CRT前后表中的参数。LVEF:左心室射血分数;LVESV:左心室收缩末体积。*P < 0.05。 表 4 与CRT应答相关变量的Logistic回归分析
Table 4. Logistic regression of factors associated with CRT response.
项目 OR 95% CI P 病因学 扩张性心肌病 16.359 3.324~80.508 0.001 缺血性心肌病 1 年龄(每增加10岁) 1.72 1.00~2.96 0.050 基线LVEF(每增加10%) 5.72 1.95~16.79 0.002 基线LVEDV(每增加10 mL) 1.15 1.06~1.25 0.001 术后QRS宽度变化(每增加10 ms) 0.55 0.39~0.76 < 0.001 术后fQRS导联数量变化(每增加1) 0.798 0.642~0.993 0.043 CI:可信限;LVEF:左心室射血分数;LVESV:左心室舒张末体积;fQRS:碎裂QRS波。 -
[1] Normand C, Linde C, Singh J, Dickstein K. Indications for Cardiac Resynchronization Therapy: A Comparison of the Major International Guidelines. JACC Heart Fail 2018; 6(4): 308-316. doi: 10.1016/j.jchf.2018.01.022 [2] Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology(ESC). Developed with the special contribution of the Heart Failure Association(HFA)of the ESC. Eur J Heart Fail 2016; 18(8): 891-975. doi: 10.1002/ejhf.592 [3] Leclercq C, Burri H, Curnis A, et al. Cardiac resynchronization therapy non-responder to responder conversion rate in the more response to cardiac resynchronization therapy with MultiPoint Pacing(MORE-CRT MPP)study: results from Phase I. Eur Heart J 2019; 40(35): 2979-2987. doi: 10.1093/eurheartj/ehz109 [4] Sohaib SM, Chen Z, Whinnett ZI, et al. Meta-analysis of symptomatic response attributable to the pacing component of cardiac resynchronization therapy. Eur J Heart Fail 2013; 15(12): 1419-1428. doi: 10.1093/eurjhf/hft139 [5] Daubert C, Behar N, Martins RP, Mabo P, Leclercq C. Avoiding non-responders to cardiac resynchronization therapy: a practical guide. Eur Heart J 2017; 38(19): 1463-1472. [6] Das MK, Suradi H, Maskoun W, et al. Fragmented wide QRS on a 12-lead ECG: a sign of myocardial scar and poor prognosis. Circ Arrhythm Electrophysiol 2008; 1(4): 258-68. doi: 10.1161/CIRCEP.107.763284 [7] Das MK. Can fragmented QRS help in risk-stratifying patients with coronary artery disease and a relatively preserved ejection fraction? Heart Rhythm 2012; 9(6): 936-937. doi: 10.1016/j.hrthm.2012.01.017 [8] Chanavuth K, Pattara R, Poemlarp M, et al. Baseline fragmented QRS is associated with increased all-cause mortality in heart failure with reduced ejection fraction: A systematic review and meta-analysis[J]. Annals of noninvasive electrocardiology : the official journal of the International Society for Holter and Noninvasive Electrocardiology, Inc 2019; 24(2): e12597. doi: 10.1111/jce.13139 [9] Igarashi M, Tada H, Yamasaki H, et al. Fragmented QRS Is a Novel Risk Factor for Ventricular Arrhythmic Events After Receiving Cardiac Resynchronization Therapy in Nonischemic Cardiomyopathy[J]. J Cardiovasc Electrophysiol 2017; 28(3): 327-335. doi: 10.1111/anec.12186 [10] Chanavuth K, Pattara R, Poemlarp M, et al. Baseline fragmented QRS is associated with increased all-cause mortality in heart failure with reduced ejection fraction: A systematic review and meta-analysis. Annals of noninvasive electrocardiology: the official journal of the International Society for Holter and Noninvasive Electrocardiology, Inc 2019; 24(2): e12597. doi: 10.1111/anec.12597 [11] Das MK, El Masry H. Fragmented QRS and other depolarization abnormalities as a predictor of mortality and sudden cardiac death. Curr Opin Cardiol 2010; 25(1): 59-64. doi: 10.1097/HCO.0b013e328333d35d [12] Chung ES, Leon AR, Tavazzi L, et al. Results of the Predictors of Response to CRT (PROSPECT) trial. Circulation 2008; 117(20): 2608-2616. doi: 10.1161/CIRCULATIONAHA.107.743120 [13] A NS, A RC. Is CRT response rate all about patient selection? International journal of cardiology 2018; 270: 183-184. doi: 10.1016/j.ijcard.2018.06.079 [14] Rickard J, Michtalik H, Sharma R, et al. Predictors of response to cardiac resynchronization therapy: A systematic review. Int J Cardiol 2016; 225: 345-352. doi: 10.1016/j.ijcard.2016.09.078 [15] Lawin D, Stellbrink C. Change in indication for cardiac resynchronization therapy? Eur J Cardiothorac Surg 2019; 55(Suppl 1): i11-i6. [16] Vernooy K, van Deursen CJ, Strik M, Prinzen FW. Strategies to improve cardiac resynchronization therapy. Nat Rev Cardiol 2014; 11(8): 481-493. doi: 10.1038/nrcardio.2014.67 [17] Chew DS, Wilton SB, Kavanagh K, et al. Fragmented QRS complexes after acute myocardial infarction are independently associated with unfavorable left ventricular remodeling. J Electrocardiol 2018; 51(4): 607-612. doi: 10.1016/j.jelectrocard.2018.04.004 [18] Amir A, Amir T, Zahra E. Diffuse fragmented QRS as an index of extensive myocardial scar. Indian pacing and electrophysiology journal 2010; 10(1): 67-68. [19] Mohamed H, Lamaan A, Bilal S, Jo M, K DM. Fragmented QRS complexes on 12-lead ECG: a marker of cardiac sarcoidosis as detected by gadolinium cardiac magnetic resonance imaging. Annals of noninvasive electrocardiology: the official journal of the International Society for Holter and Noninvasive Electrocardiology, Inc 2009; 14(4): 319-326. doi: 10.1111/j.1542-474X.2009.00320.x [20] Luc L, Alexandre C, Olivier C, et al. Relationship between fragmented QRS and no-reflow, infarct size, and peri-infarct zone assessed using cardiac magnetic resonance in patients with myocardial infarction. The Canadian journal of cardiology 2014; 30(2): 204-210. doi: 10.1016/j.cjca.2013.11.026 [21] Das MK, Maskoun W, Shen C, et al. Fragmented QRS on twelve-lead electrocardiogram predicts arrhythmic events in patients with ischemic and nonischemic cardiomyopathy. Heart Rhythm 2010; 7(1): 74-80. doi: 10.1016/j.hrthm.2009.09.065 [22] Diaz-Infante E, Mont L, Leal J, et al. Predictors of lack of response to resynchronization therapy. Am J Cardiol 2005; 95(12): 1436-1440. doi: 10.1016/j.amjcard.2005.02.009 [23] Rickard J, Zardkoohi O, Popovic Z, et al. QRS fragmentation is not associated with poor response to cardiac resynchronization therapy[J]. Ann Noninvasive Electrocardiol 2011; 16(2): 165-171. doi: 10.1111/j.1542-474X.2011.00424.x [24] Hu YR, Hua W, Yang SW, et al. Predictors of non-response to cardiac resynchronization therapy implantation in patients with class I indications: the markedly dilated left ventricular end-diastolic dimension and the presence of fragmented QRS. J Geriatr Cardiol 2019; 16(7): 514-521. -






 下载:
下载: