Correlation between Anxiety Depression Symptoms of Patients with Chronic Obstructive Pulmonary Disease and CAT Score
-
摘要:
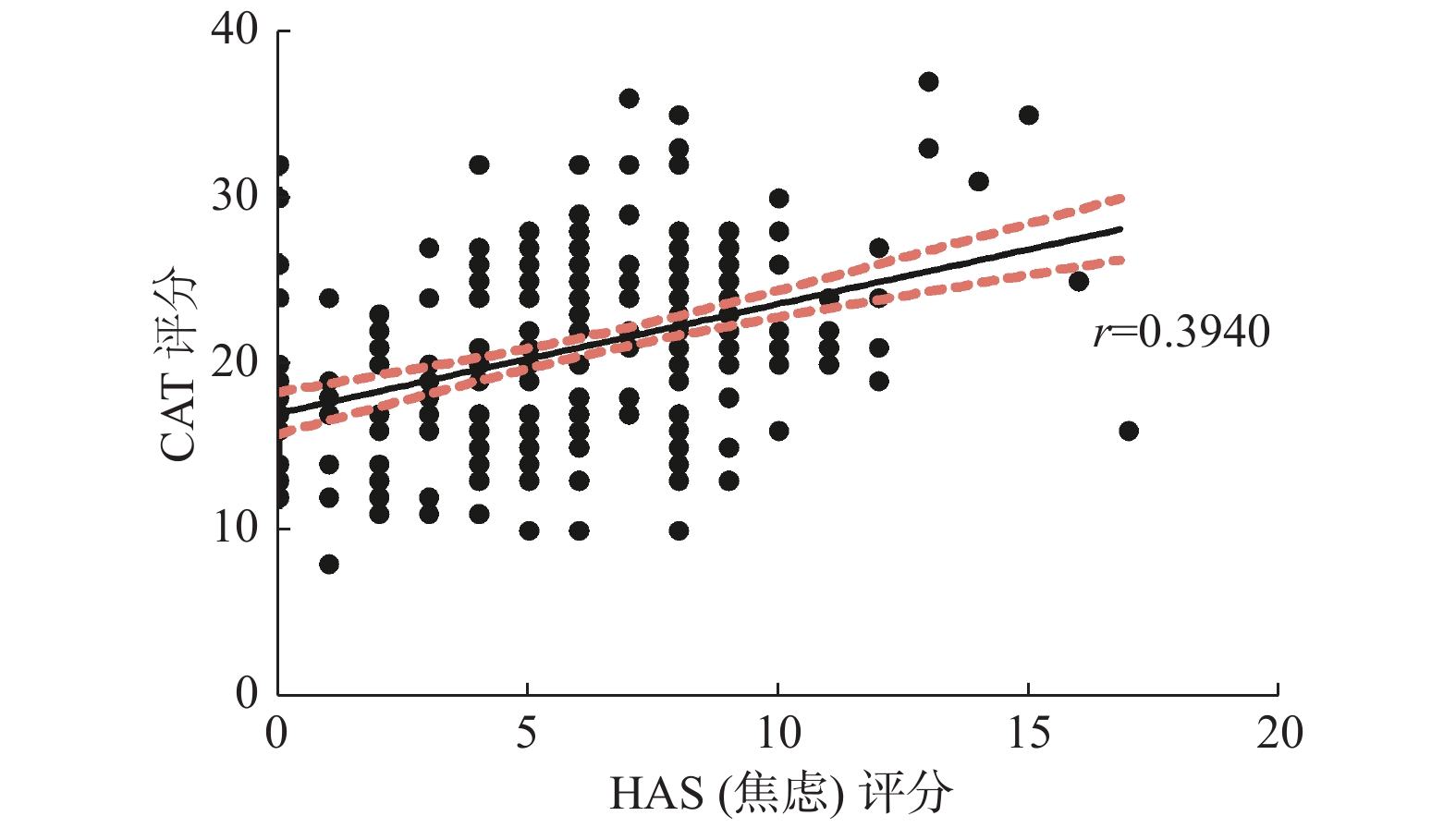
目的 评价慢性阻塞性肺疾病(慢阻肺)患者中焦虑和/或抑郁的发生率及相关危险因素,并探讨慢阻肺患者焦虑抑郁症状与CAT评分的相关关系,为慢阻肺患者的负性情绪干预提供科学依据。 方法 选择于2019年7月至2019年10月晋宁区第二人民医院、昆明市第一人民医院收治的慢阻肺患者313例,利用医院焦虑抑郁量表(HADS)和慢性阻塞性肺疾病评估(CAT)进行问卷调查并记录患者相关资料,使用SPSS24.0软件进行统计分析。 结果 纳入研究的312例患者中,COPD合并焦虑者占比49.2%(154例),合并抑郁者占比37.2%(116例),同时合并焦虑和抑郁者占比22.8%(71例)。COPD合并焦虑与患者的医疗费用支付方式、住院次数、是否有并发症以及CAT评分有关(P < 0.05),合并抑郁与患者的住院次数以及CAT评分有关( P < 0.05)。CAT评分与焦虑抑郁相互影响,随着焦虑抑郁严重程度的递进,COPD患者的CAT评分随之升高。 结论 慢阻肺合并焦虑抑郁的患病率较高,且住院次数频繁和CAT评分相对较高是其高危因素。焦虑抑郁分级程度与患者病情严重程度呈正相关。 Abstract:Objective To evaluate the incidence and risk factors for anxiety and/or depression in patients with chronic obstructive pulmonary disease(COPD), and to explore the correlation between the anxiety depression symptoms and CAT score of patients with COPD; to provide scientific evidence for the negative emotion intervention of COPD patients in the future. Methods A total of 313 patients with COPD were enrolled in this study from the Second People's Hospital of Jinning District and the First Hospital of Kunming from July 2019 - October 2019. We used the Hospital Anxiety and Depression Scale(HADS)and COPD Assessment Test(CAT)to conduct the questionnaire survey and collect data of the patients, and then use SPSS 24.0 for analysis. Results Among the 312 patients, COPD patients with anxiety accounted for 49.2%(154 cases), COPD with depression accounted for 37.2%(116 cases), COPD with both anxiety and depression accounted for 22.8%(71 cases). COPD patients with anxiety were associated with paying method of medical expenditure, hospitalization frequency, complications and CAT score(P < 0.05), and patients with depression were associated with hospitalization frequency and CAT score( P < 0.05). CAT score and anxiety depression symptoms are interrelated. Conclusion The prevalence of COPD complicated with anxiety and depression is high. And frequent hospitalization and CAT scores are the high risk factors. The degree of anxiety and depression was positively correlated with the severity of the patient's condition. -
Key words:
- Chronic obstructive pulmonary disease /
- Anxiety /
- Depression /
- Relevant factor /
- CAT score
-
表 1 不同特征COPD患者同焦虑、抑郁发生率比较[n(% )]
Table 1. Comparison of the incidence of anxiety and depression among patients with different characteristics of COPD[n(%)]
项目 合计 焦虑发生情况 抑郁发生情况 焦虑组 非焦虑组 χ2 P 抑郁组 非抑郁组 χ2 P 性别 1.466 0.226 0.644 0.422 男 227(73.0) 107(48.2) 115(51.8) 82(36.4) 143(63.6) 女 84(27.0) 47(56.0) 37(44.0) 34(41.5) 48(58.5) 年龄/岁 1.322 0.724 0.811 0.847 ≤60 87(27.9) 46(53.5) 40(46.5) 32(37.2) 54(62.8) 60~69 88(28.2) 44(51.2) 42(48.8) 33(38.4) 53(61.6) 70~79 80(25.6) 39(50.0) 39(50.0) 27(34.6) 51(65.4) ≥80 57(18.3) 25(43.9) 32(56.1) 24(42.1) 33(57.9) 民族 0.210 0.647 3.799 0.051 汉族 305(98.4) 151(50.3) 149(49.7) 112(37.3) 188(62.7) 少数民族 5(1.6) 2(40.0) 3(60.0) 4(80.0) 1(20.0) 婚姻状况 0.033 0.857 0.228 0.633 初婚 263(84.3) 130(50.4) 128(49.6) 96(37.2) 162(62.8) 其他 49(15.7) 24(49.0) 25(51.0) 20(40.8) 29(59.2) BMI/(kg/m2) 0.922 0.631 1.174 0.556 < 18.5 8(2.6) 3(37.5) 5(62.5) 2(25.0) 6(75.0) 18.5~24.9 216(70.4) 110(51.6) 103(48.4) 83(39.2) 129(60.8) ≥25 83(27.0) 39(47.6) 43(52.4) 28(34.1) 54(65.9) 文化程度 1.266 0.737 0.656 0.883 初中及以下 154(49.7) 76(50.3) 75(49.7) 55(36.4) 96(63.6) 高中/中专 143(46.1) 73(51.8) 68(48.2) 55(39.0) 86(61.0) 大专/本科 9(2.9) 4(44.4) 5(55.6) 4(44.4) 5(55.6) 研究生及以上 4(1.3) 1(25.0) 3(75.0) 1(25.0) 3(75.0) 居住地 0.015 0.903 1.176 0.186 城镇 258(84.3) 130(51.0) 125(49.0) 93(36.6) 161(63.4) 农村 48(16.7) 23(50.0) 23(50.0) 22(46.8) 25(53.2) 职业 0.695 0.404 2.446 0.118 在职人员 91(29.7) 47(53.4) 41(46.6) 40(44.4) 50(55.6) 离退休人员 216(70.4) 103(48.1) 111(51.9) 74(34.9) 138(65.1) 家庭经济来源 0.968 0.325 0.403 0.525 稳定 68(66.7) 44(64.7) 24(35.3) 30(44.8) 37(55.2) 不稳定 34(33.3) 18(54.5) 15(45.5) 17(51.5) 16(48.5) 平均月收入(元) 1.369 0.504 2.336 0.311 2 000以下 34(11.0) 18(56.3) 14(43.8) 17(50.0) 17(50.0) 2 000~5000 143(46.1) 74(52.1) 68(47.9) 50(36.2) 88(63.8) 5000以上 133(42.9) 61(46.6) 70(53.4) 49(36.8) 84(63.2) 医疗费用支付方式 11.099 0.004 5.858 0.053 自费 28(9.1) 15(57.7) 11(42.3) 14(51.9) 13(48.1) 居民医保/农村合作医疗 116(37.7) 44(38.3) 71(61.7) 35(30.4) 80(69.6) 省/市职工医保 164(53.3) 94(58.0) 68(42.0) 67(41.6) 94(58.4) 住院次数 13.449 0.001 40.757 < 0.001 2次及以下 180(59.8) 76(42.9) 101(57.1) 41(23.0) 137(77.0) 3~5次 91(30.2) 60(66.7) 30(33.3) 54(60.0) 36(40.0) 5次以上 30(10.0) 15(51.7) 14(48.3) 17(58.6) 12(41.4) 是否有并发症 6.691 0.035 1.834 0.400 是 68(22.15) 40(61.5) 25(38.5) 29(44.6) 36(55.4) 否 239(77.85) 109(46.4) 126(53.6) 84(35.7) 151(64.3) 表 2 COPD患者罹患焦虑或抑郁以及同时患焦虑抑郁的分布情况[n(%)]
Table 2. The distribution of anxiety/depression,anxiety and depression in patients with COPD[n(%)]
焦虑抑郁程度 患病情况 焦虑 抑郁 同时焦虑抑郁 轻度 134(87.01) 82(70.69) 60(84.51) 中度 16(10.39) 29(25.00) 7(9.86) 重度 4(2.60) 5(4.31) 4(5.63) 合计 154(49.2) 116(37.2) 71(22.8) 表 3 焦虑抑郁程度与CAT评分分级关系比较[n(%)]
Table 3. Comparison of the relationship between anxiety/depression and CAT level[n(%)]
HADS评分(分) Mean ± SD(分) CAT评分(分) G P 轻度影响(0~10) 中度影响(11~20) 重度影响(21~30) 极重度影响(31~40) HAS(焦虑)评分 无(0~7) 22.22 ± 5.72 4(2.6) 89(58.6) 52(34.2) 7(4.6) 0.557 < 0.001 轻度(8~10) 22.76 ± 3.82 1(0.7) 33(24.6) 97(72.4) 3(2.2) 中重度(11~21) 26.62 ± 1.12 0(0.0) 4(20.0) 11(55.0) 5(25.0) 总计 21.42 ± 5.28 6(1.6) 126(41.2) 160(52.3) 15(4.9) HDS(抑郁)评分 无(0~7) 22.32 ± 5.71 4(2.1) 93(50.8) 87(43.5) 7(3.7) 0.274 < 0.001 轻度(8~10) 22.85 ± 3.96 0(0.0) 20(24.7) 57(70.4) 4(4.9) 中重度(11~21) 25.13 ± 3.85 1(2.9) 6(17.6) 22(64.7) 5(14.7) 总计 21.51 ± 5.31 5(1.6) 123(40.2) 162(52.9) 16(5.2) 表 4 焦虑抑郁程度对CAT评分影响的多因素Logistic回归分析
Table 4. Multivariate Logistic regression analysis of the influence of anxiety and depression degree on CAT score
项目 Model1 Model2 Model3 P OR(95%CI) P OR(95%CI) P OR(95%CI) 焦虑程度 无 / 1(ref) / 1(ref) / 1(ref) 轻度 < 0.001 5.892(3.404,10.200) < 0.001 5.817(3.334,10.151) < 0.001 4.432(2.575,7.627) 中重度 0.004 7.020(1.889,26.094) 0.005 6.681(1.789,24.950) < 0.001 6.256(1.665,23.505) 抑郁程度 无 / 1(ref) / 1(ref) / 1(ref) 轻度 < 0.001 4.112(2.189,7.726) < 0.001 4.806(2.468,9.357) < 0.001 3.463(1.802,6.653) 中重度 0.001 6.462(2.138,19.537) 0.001 6.832(2.242,20.815) < 0.001 3.918(1.550,9.901) Model1:不调整;
Model2:调整年龄、性别、民族;
Model3:调整年龄、性别、民族、医疗费用支付方式、住院次数、是否有并发症。 -
[1] Struik F M,Sprooten R T,Kerstjens H A,et al. Nocturnal non-invasive ventilation in COPD patients with prolonged hypercapnia after ventilatory support for acute respiratory failure:A randomised,controlled,parallel-group study[J]. Thorax,2014,69(9):826-834. doi: 10.1136/thoraxjnl-2014-205126 [2] López-Campos J L,Soler-Cataluña J J,Miravitlles M. Global strategy for the diagnosis,management,and prevention of chronic obstructive lung disease 2019 report:Future challenges[J]. Arch Bronconeumol,2020,56(2):65-67. doi: 10.1016/j.arbres.2019.06.001 [3] 王小仁. 慢性阻塞性肺疾病患者家庭功能、社会支持、心理状态及生存质量现况调查及相关性研究[D]. 广州: 南方医科大学硕士学位论文, 2016. [4] Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010[J]. Lancet, 2012, 380(9859): 2095-2128. [5] Zhovanyk N V,Tovt-Korshynska M I. Interaction between clinical and psychological changes among patients with chronic obstructive pulmonary disease and pulmonary tuberculosis co-morbidity[J]. Wiad Lek,2019,72(4):635-638. doi: 10.36740/WLek201904125 [6] 陈亚红. 2020年GOLD慢性阻塞性肺疾病诊断、治疗及预防全球策略解读[J].中国医学前沿杂志(电子版),2019,11(12):32-50. [7] 张小娥,张彩莲. 慢性阻塞性肺疾病流行病学及疾病经济负担研究进展[J].中国慢性病预防与控制,2017,25(06):472-476. [8] Yang G,Wang Y,Zeng Y,et al. Rapid health transition in China,1990-2010:Findings from the global burden of disease study 2010[J]. Lancet,2013,381(9882):1987-2015. doi: 10.1016/S0140-6736(13)61097-1 [9] 崔亚楠,陈平,陈燕. 2018年版慢性阻塞性肺疾病全球倡议诊断及处理和预防策略解读[J].中华结核和呼吸杂志,2018,41(03):236-239. doi: 10.3760/cma.j.issn.1001-0939.2018.03.019 [10] Rabe K F,Watz H. Chronic obstructive pulmonary disease[J]. Lancet,2017,389(10082):1931-1940. doi: 10.1016/S0140-6736(17)31222-9 [11] 李希,谭双香,胡瑞成,等. 慢性阻塞性肺疾病合并焦虑/抑郁的相关因素[J].临床与病理杂志,2019,39(02):307-313. [12] 柳青,李风雷. 慢性阻塞性肺疾病患者焦虑和抑郁情绪调查分析[J].现代医院,2019,19(06):933-936. doi: 10.3969/j.issn.1671-332X.2019.06.045 [13] 齐佳华,王红阳. 慢性阻塞性肺疾病合并焦虑、抑郁的情况调查[J].华北理工大学学报(医学版),2018,20(02):118-122. [14] Kessler R C,Nelson C B,McGonagle K A,et al. Comorbidity of DSM-III-R major depressive disorder in the general population:results from the US national comorbidity survey[J]. Br J Psychiatry Suppl,1996(30):17-30. [15] 陈华萍,尹燕,贺斌峰,等. 慢性阻塞性肺疾病合并焦虑抑郁的临床分析[J].中华肺部疾病杂志(电子版),2019,12(06):677-681. doi: 10.3877/cma.j.issn.1674-6902.2019.06.002 [16] 丁静怡. 慢性阻塞性肺疾病合并焦虑抑郁的相关因素分析[J].临床肺科杂志,2018,23(04):690-693. doi: 10.3969/j.issn.1009-6663.2018.04.029 [17] 肖仁森. 稳定期慢性阻塞性肺病患者焦虑、抑郁发生及与急性加重相关因素分析[D]. 南昌: 南昌大学硕士论文, 2019. [18] Hyun M K,Lee N R,Jang E J,et al. Effect of inhaled drugs on anxiety and depression in patients with chronic obstructive pulmonary disease:A prospective observational study[J]. Int J Chron Obstruct Pulmon Dis,2016,2016(11):747-754. [19] Singh G,Zhang W,Kuo Y F,et al. Association of psychological disorders with 30-day readmission rates in patients with COPD[J]. Chest,2016,149(4):905-915. doi: 10.1378/chest.15-0449 [20] 张庆,徐爱晖. CAT评分与mMRC评分对慢性阻塞性肺疾病患者病情评估比较[J].临床肺科杂志,2018,23(12):2156-2159. doi: 10.3969/j.issn.1009-6663.2018.12.006 [21] 焦涛. 慢性阻塞性肺疾病患者焦虑抑郁状况调查[D]. 合肥: 安徽医科大学硕士论文, 2013. [22] 赵冲. CAT、mMRC、CCQ、SGRQ四种评分系统在COPD患者肺功能及生活质量评价中的价值与差异[J].临床肺科杂志,2018,23(11):2060-2064. doi: 10.3969/j.issn.1009-6663.2018.11.031 -






 下载:
下载: