-
摘要:
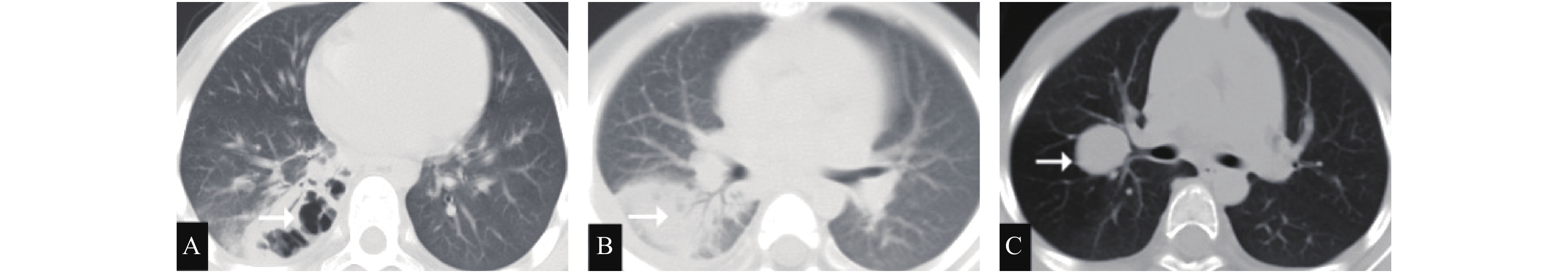
目的 分析儿童坏死性肺炎(NP)的临床特征、治疗方法及预后。 方法 回顾性收集昆明市儿童医院呼吸内科自2017年04月至2020年04月收治住院的46例NP患儿的临床资料,根据病原学分为肺炎支原体坏死性肺炎(MPNP)组和细菌性坏死性肺炎(BNP)组,对比两组的临床表现、实验室检查结果、影像学特征、支气管镜下表现、治疗过程及预后情况。 结果 46例NP病例中MPNP有30例,BMP有16例。MPNP组患儿年龄明显大于BNP组患儿。总发热天数MPNP组和BNP组比较,差异无统计学意义(P = 0.061);有呼吸急促且需要氧疗的比例,BNP组明显大于MPNP组;有呼吸衰竭需要机械辅助通气的比例,两组差异无统计学意义(P = 0.310);实验室检查发现,BNP与MPNP患儿相比白细胞计数、前降钙素(PCT)C反应蛋白(CRP)均高(P = 0.031)。影像学检查发现,MPNP组坏死病灶出现明显晚于BNP组。两组合并胸腔积液比例的差异无统计学意义(P = 0.325)。电子支气管镜检查发现,MPNP患儿气管支气管黏膜、支气管管腔、分泌物性状呈多样性炎性改变。BNP气管支气管黏膜、支气管管腔、分泌物主要呈化脓性改变。两组病例经有效治疗后均好转出院,无死亡病例。两组住院时间的差异无统计学意义(P = 0.362)。两组影像学大部分病灶吸收时间的差异无统计学意义(P = 0.284)。 结论 NP发热时间长,住院时间长,影像学吸收时间长,支气管镜下表现严重且多样化。超过10d以上的发热咳嗽,伴有胸腔积液、CRP大于80 mg/L和米汤样肺泡灌洗液可能是NP发生的危险因素。NP经积极、有效治疗,预后大多良好。 Abstract:Objective To study the clinical characteristics, treatment and prognosis of necrotizing pneumonia (NP) in children. Method The clinical data of 46 patients with NP admitted to the Department of Respiratory Medicine of Kunming Children's Hospital from April 2017 to April 2020 were collected retrospectively. According to the etiological score, the patients were divided into mycoplasma pneumoniae necrotizing pneumonia (MPNP) group and bacterial necrotizing pneumonia (BNP) group. The clinical manifestations, laboratory examination results, imaging features, bronchoscopic manifestations, treatment process and prognosis of the two groups were compared later. Methods Of the 46 NP cases, 30 were MPNP and 16 were BMP. The age of children in MPNP group was significantly higher than that in BNP group. There was no significant difference between the total fever days in MPNP group and the total fever days in BNP group. The proportion of patients with shortness of breath and in need of oxygen therapy was significantly higher in BNP group than that in MPNP group. There was no significant difference between the two groups in the proportion of respiratory failure requiring mechanical ventilation. Laboratory tests showed that BNP had the higher white blood cell count and PCT c-reactive protein (CRP) than MPNP children. Imaging examination showed that the necrotic lesion in MPNP group was significantly later than that in BNP group. There was no significant difference in the proportion of pleural effusion between the two combinations. Electronic bronchoscopy revealed that there were a variety of inflammatory changes in the characteristics of tracheal and bronchial mucosa, bronchial lumen and secretions of MPNP children. The bronchial mucosa, lumen and secretions of BNP were mainly suppurative. After the effective treatment, the two groups of patients improved and were discharged from the hospital without any death. There was no significant difference in length of stay between the two groups. There was no significant difference in the absorption time between the two groups. Conclusion Patients with NP have the long fever, long hospital stay, long imaging absorption, and severe and diverse bronchoscopy. Fever and cough for more than 10 days, pleural effusion, CRP for more than 80 mg/L, and ricin-like alveolar lavage fluid may be the risk factors for NP development. NP has a good prognosis after the active and effective treatment. -
Key words:
- Children /
- Mycoplasma pneumoniae /
- Necrotic pneumonia /
- Bacteria
-
表 1 MPNP组与MPP组研究对象特征的比较(
$\bar x \pm s $ )Table 1. Clincal charateristics of the patients of MPNP and MPP(
$\bar x \pm s $ )组别 MPNP BNP t/χ2 P n 30 16 年龄(岁) 8.4 ± 3.9 3.1 ± 2.2 5.16 0.021 表 2 MPNP组与BNP组临床特征及实验室数据比较(
$\bar x \pm s $ )Table 2. Comparison of clinical characters and laboratory data between MPNP and BNP(
$ \bar x \pm s$ )组别 MPNP BNP t P 发热天数(d) 12.7 ± 3.3 14.5 ± 4.2 0.28 0.061 住院天数(d) 19.20 ± 3.28 21.24 ± 5.16 3.54 0.362 影像学吸收时间(d) 140.00 ± 78.29 13.3 ± 4.8 4.86 0.005 白细胞计数(×109/L) 11.43 ± 3.51 23.52 ± 5.83 0.58 0.024 CRP(mg/L) 81.07 ± 35.89 98.16 ± 61.93 1.83 0.031 前降钙素(PCT) 1.72×63.58 90.38×72.16 2.23 0.042 需氧疗的比例(%) 26.7 87.5 4.72 0.013 需机械通气比例(%) 6.7 18.8 0.27 0.310 -
[1] Nicolaou E V, Bartlett A H. Necrotizing pneumonia[J]. Pediatr Ann,2017,46(2):e65-e68. doi: 10.3928/19382359-20170120-02 [2] 刘祥军, 周怀美, 姜建渝, 等. 儿童坏死性肺炎并致死性大咯血一例[J].中国小儿急救医学,2018,25(10):799-800. [3] 刘金荣, 徐保平, 李惠民, 等. 肺炎链球菌坏死性肺炎20例诊治分析[J].中华儿科杂志,2012,50(6):431-434. [4] Wang Y, Xu D, Li S, et al. Mycoplasma pneumoniae‐associated necrotizing pneumonitis in children[J]. Pediatr Int,2012,54(2):293-297. doi: 10.1111/j.1442-200X.2011.03415.x [5] 费文祎, 罗健. 儿童坏死性肺炎诊治进展[J].临床儿科杂志,2018,36(4):306-310. [6] 张园园, 戴菱曼, 周云连, 等. 儿童细菌性坏死性肺炎与肺炎支原体坏死性肺炎临床特征与预后比较[J].中华儿科杂志,2019,57(8):625-630. [7] Sawicki G S, Lu F L, Valim C, et al. Necrotising pneumonia is an increasingly detected complication of pneumonia in children[J]. Eur Respir J,2008,31(6):1285-1291. doi: 10.1183/09031936.00099807 [8] 杨男, 陈宁, 尚云晓, 等. 儿童坏死性肺炎49例临床分析[J].中华实用儿科临床杂志,2017,32(4):280-283. [9] 曾洪武, 黄文献、陈杰华, 等. 儿童坏死性肺炎的临床特点及胸部HRCT特征[J].放射学实践,2018,33(7):758-761. [10] 李素荣, 牟京辉, 常丽, 等. 肺炎支原体感染所致儿童坏死性肺炎30例胸部CT表现及转归[J].中华儿科杂志,2013,51(3):211-215. [11] 王秀芳, 李伟霞, 张艳丽, 等. 儿童肺炎支原体坏死性肺炎预测指标研究[J].临床儿科杂志,2019,37(6):409-412. doi: 10.3969/j.issn.1000-3606.2019.06.003 [12] 杨魏娜, 刘君辉, 柯玲嗣, 等. 可弯曲支气管镜诊治儿童坏死性肺炎32例临床分析[J].中国实用儿科杂志,2019,34(3):227-229. [13] 立新, 贺亚琼, 刘建滨, 等. 3岁以内婴幼儿肺结核CT诊断[J].放射学实践,2012,27(9):1001-1005. [14] Ceccato A, Cilloniz C, Ranzani O T, et al. Treatment with macrolides and glucocorticosteroids in severe community-acquired pneumonia: A post-hoc exploratory analysis of a randomized controlled trial[J]. PLoS One,2017,12(6):e0178022. [15] Cheng M, Pan Z Y, Yang J, et al. Corticosteroid therapy for severe community-acquired pneumonia: a meta-analysis[J]. Respir Care,2014,59(4):557-563. doi: 10.4187/respcare.03506 [16] 焦安夏, 刘玺诚, 孟晨, 等. 中国儿童难治性肺炎呼吸内镜介入诊疗专家共识[J].中国实用儿科杂志,2019,34(6):449-457. [17] 王来成, 王惠丽, 赵瑜. 经支气管镜注射布地奈德治疗儿童肺炎支原体大叶性肺炎[J].中国实用医药,2016,11(9):168-170. [18] 李伟霞, 王秀芳, 张艳丽, 等. 儿童肺炎支原体性坏死性肺炎37例临床诊治分析[J].中国小儿急救医学,2018,25(9):712-714. -






 下载:
下载: