Comparative Study of Two Surgical Procedures for Osteoporotic Delayed Vertebral Collapse
-
摘要:
目的 探讨迟发性骨质疏松椎体塌陷有效治疗方法。 方法 选取研究纳入2013年3月至2018年3月期间入住解放军联勤保障部队九二〇医院,不伴有神经症状的迟发性骨质疏松椎体塌陷患者,接受经后路内固定联合椎体成形术(PFV组)或经皮穿刺椎体后凸成形术(PKP组)。比较两组患者围手术期临床结果和影像学参数及远期并发症。 结果 术后PFV组伤椎前缘高度和局部Cobb角恢复显著优于PKP组(P < 0.001)。术后1周VAS评分和ODI值评分PKP组均优于PFV组(P = 0.03)。PFV组术后发生相邻椎体骨折1例(4%),钉棒内固定松动2例(8%)。PKP组4例(18%)术后发生严重后凸畸形,2例出现神经症状,行2次手术治疗。 结论 迟发性骨质疏松椎体塌陷的手术治疗,PFV和PKP均能取得满意的临床疗效,PKP适用于单椎体且脊柱矢状面无明显改变的患者,而PFV更适用于脊柱矢状位明显改变的迟发性骨质疏松椎体塌陷患者。 -
关键词:
- 迟发性骨质疏松椎体塌陷 /
- 后路内固定联合椎体成形术 /
- 经皮穿刺椎体后凸成形术
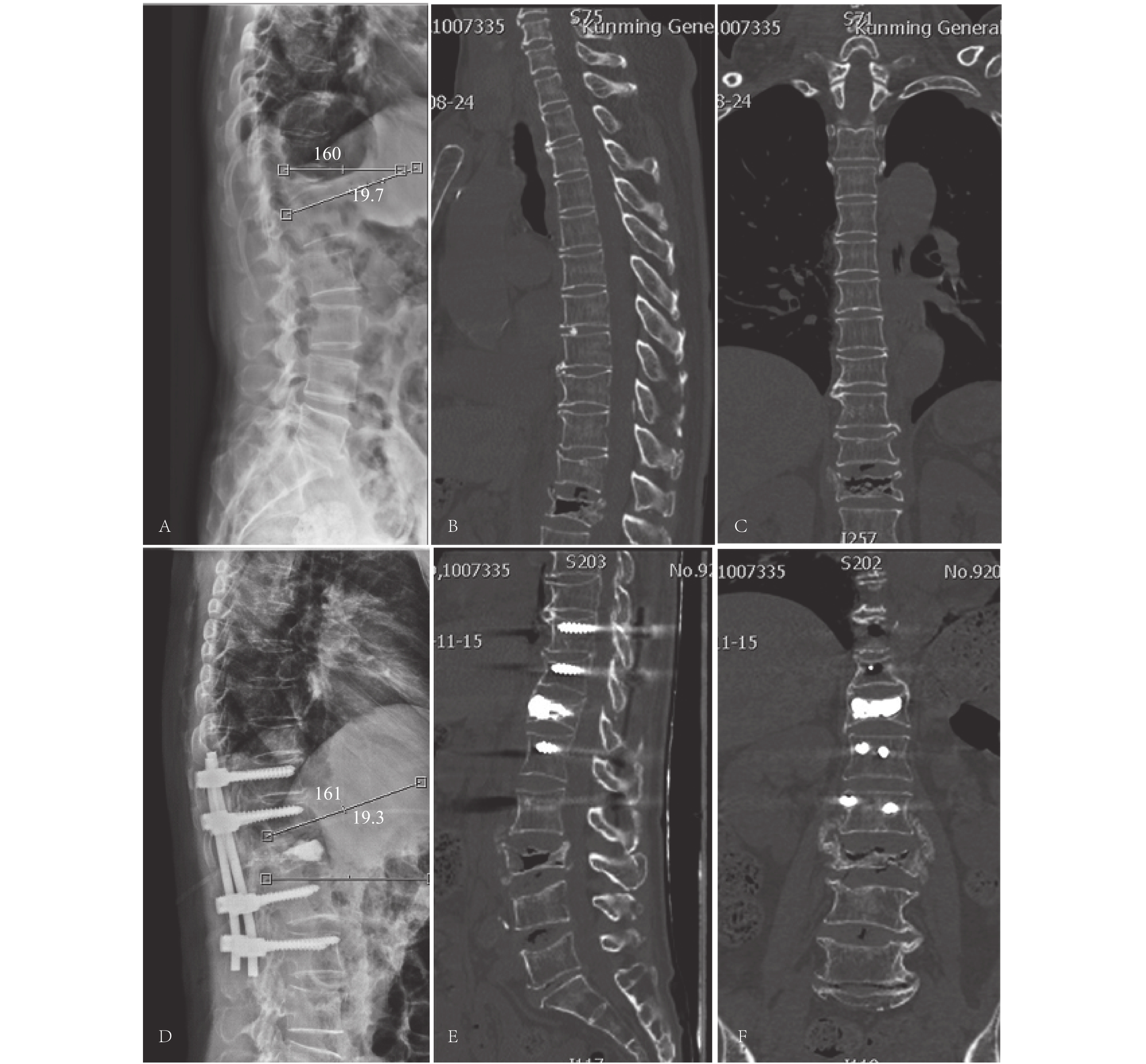
Abstract:Objective To explore the effective treatment for osteoporotic delayed vertebral collapse. Methods Between March 2013 and March 2018, a total of 46 patients with osteoporotic delayed vertebral fracture with no or mild neurological symptoms were enrolled in our hospitals. 24 patients underwent posterior fixation with vertebroplasty(PFV group), and 22 patients underwent percutaneous balloon kyphoplasty(PKP group). The clinical results, imaging parameters and long-term complications were compared between the two groups. Results Postoperative PFV group had significantly higher vertebrae height and local Cobb angle recovery than PKP group(P < 0.001). The VAS score and ODI score in the PKP group were better than those in the PFV group(P = 0.03). There was no significant difference between the two groups at the last follow-up(P = 0.28). In the PFV group, 3 cases(12.5%)had adjacent vertebral fractures, 3 cases(16.7%)had internal fixation loosening, and 1 case(4.5%)had revision surgery. In the PKP group, 4 cases had severe kyphosis, 2 cases had neurological symptoms, and 2 cases underwent revision surgery. Conclusions Both PFV and PKP for delayed osteoporosis vertebral collapse can achieve satisfactory clinical results. PFVB is indicated for patients with a significant change in the sagittal position of the spine, whereas PKP is suitable for a single vertebral body and no significant changes in the sagittal plane of the spine. -
表 1 两组患者基本资料的比较[(
$\bar x \pm s$ ),n = 24]Table 1. Comparison of basic data of patients in 2 groups [(
$\bar x \pm s $ ),n = 24]项目 PFV组 PKP组 P 纳入病例 24 22 性别(男/女) 11/13 8/14 年龄(岁) 65.4 ± 2.3 67.8 ± 2.3 0.35 病史(月) 8.2 ± 2.3 7.6 ± 1.9 0.24 骨折节段 T11 5 3 0.18 T12 10 8 0.16 L1 8 9 0.98 L2 1 2 0.88 随访时间(月) 18 ± 6.0 20 ± 4.0 0.41 PFV:后路内固定联合骨水泥术;PKP:经皮穿刺椎体后凸成形术。 表 2 两组患者术前术中参数比较[(
$\bar x\pm s$ ),n = 24]Table 2. Comparison of preoperative and intraoperative parameters between the two groups[(
$\bar x\pm s$ ),n = 24]项目 PFV组 PKP组 P 手术时间(min) 123.6 ± 35(97~162) 26.3 ± 16(20~50) 0.00 术中出血(mL) 320.1 ± 60(280~380) 35.0 ± 16.4(13~51) 0.00 术中辐射时间(min) 7.5 ± 1.9(4~8) 6.2 ± 1.2(6.2~8.5) 0.14 住院时间(d) 12 ± 3.4 4 ± 2.6 < 0.00 住院费用(万元) 7.7 ± 2.3(4.6~5.8) 3.8 ± 1.7(3.2~4.5) < 0.01 表 3 手术前后椎体高度,局部Cobb角的变化(
$\bar x\pm s$ )Table 3. Changes in vertebral body height and local cobb angle before and after surgery (
$\bar x\pm s$ )项目 PFV 组 PKP组 P Cobb角(°) 术前 20.7 ± 9.8 19.7 ± 10.4 0.91 术后1周 10.4 ± 1.1 15.3 ± 4.6 0.02 术后6个月 10.1 ± 1.2 15.4 ± 3.5 0.02 术后1 a 11.0 ± 1.4 15.2 ± 1.2 0.02 末次随访 11.3 ± 5.1 15.8 ± 4.7 0.02 矫正 17.3 ± 1.2 13.5 ± 3.1 0.03 矫正丢失 3.1 ± 0.3 6.2 ± 0.5 0.001 t 8.63 2.01 P 0.001 0.08 椎体前缘高度(%) 术前 15.8 ± 6.3 17.3 ± 4.5 0.89 术后1周 23.4 ± 3.8 19.3 ± 5.7 0.03 术后6个月 23.4 ± 1.1 19.3 ± 5.8 0.03 术后1 a 23.2 ± 5.4 18.5 ± 3.9 0.03 末次随访 23.3 ± 5.1 18.4 ± 2.2 0.03 t 7.63 1.33 P 0.00 0.19 表 4 2组术前术后ODI评分[(
$\bar x\pm s$ ),%]Table 4. The preoperative and postoperative ODI scores between the 2 groups「(
$\bar x\pm s$ ),%」组别 术前 术后1周 术后6个月 术后12个月 末次随访 F P PFV组 52.3 ± 3.8 23.1 ± 1.6 16.5 ± 2.9 17.9 ± 2.5 17.5 ± 5.7 105.24 < 0.01 PKP组 55.5 ± 1.7 15.4 ± 2.3 17.1 ± 0.4 18.2 ± 1.5 18.8 ± 2.9 144.87 < 0.01 t 0.833 5.98 0.94 0.82 0.79 P 1.051 0.01 1.04 1.67 2.82 表 5 2组术前术后VAS评分[(
$\bar x\pm s$ ),n = 24]Table 5. Two groups of VAS scores before and after surgery [(
$\bar x\pm s$ ),n = 24]组别 术前 术后1周 术后6个月 术后12个月 末次随访 F P PFV组 7.1 ± 0.6 4.2 ± 0.33 3.5 ± 1.8 2.8 ± 2.7 3.6 ± 1.5 156.89 < 0.01 PKP组 7.5 ± 0.8 1.4 ± 0.57 2.1 ± 0.4 2.1 ± 0.8 2.5 ± 0.9 167.31 < 0.01 t 0.246 8.32 1.76 0.98 1.05 P 0.89 0.00 0.28 0.16 0.34 表 6 术中、后并发症(n = 24)
Table 6. Intraoperative and postoperative complications(n = 24)
项目 PFV 组 PKP 组 P 围手术期(n) 下肢静脉血栓 2 0 0.03 伤口延迟愈合 1 0 0.08 肺部感染 0 0 1.00 骨水泥渗漏 0 1 0.09 术后(n) 内固定松动 2 0 0.06 临近椎体骨折 1 0 0.08 腰背部残余痛 2 3 0.14 严重后凸畸形 0 4 0.01 神经功能损伤 0 4 0.02 二次手术 2 2 0.09 -
[1] Harada A,Matsuyama Y,Nakano T,et al. Nationwide survey of current medical practices for hospitalized elderly with spine fractures in Japan[J]. J Orthop Sci,2010,15(1):79-85. doi: 10.1007/s00776-009-1411-2 [2] Hoshino M,Nakamura H,Terai H,et al. Factors affecting neurological deficits and intractable back pain in patients with insufficient bone union following osteoporotic vertebral fracture[J]. Eur Spine J,2009,18(9):1279-1286. doi: 10.1007/s00586-009-1041-6 [3] Tsujio T,Nakamura H,Terai H,et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion:A prospective multicenter study[J]. Spine,2011,36(15):1229-1235. doi: 10.1097/BRS.0b013e3181f29e8d [4] Kim Y C,Kim Y H,Ha K Y. Pathomechanism of intravertebral clefts in osteoporotic compression fractures of the spine[J]. Spine J,2013,14(6):659-666. [5] Kim D Y,Lee S H,Jang J S,et al. Intravertebral vacuum phenomenon in osteoporotic compression fracture:report of 67 cases with quantitative evaluation of intravertebral instability[J]. J Neurosurg,2004,100(1):24-31. doi: 10.3171/jns.2004.100.1.0024 [6] Ito Y,Hasegawa Y,Toda K,et al. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture[J]. Spine J,2002,2(2):101-106. doi: 10.1016/S1529-9430(01)00165-6 [7] Kanayama M,Ishida T,Hashimoto T,et al. Role of major spine surgery using Kaneda anterior instrumentation for osteoporotic vertebral collapse[J]. J Spinal Disord Tech,2010,23(1):53-66. doi: 10.1097/BSD.0b013e318193e3a5 [8] Sudo H,Ito M,Kaneda K,et al. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits[J]. Spine J,2013,13(12):1726-1732. doi: 10.1016/j.spinee.2013.05.041 [9] Uchida K,Nakajima H,Yayama T,et al. Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine:comparisons with posterior surgery without vertebroplasty and anterior surgery:clinical article[J]. J Neurosurg,2010,13(5):612-621. [10] Suk S I,Kim J H,Lee S M,et al. Anterior-posterior surgery versus posterior closing wedge osteotomy in post-traumatic kyphosis with neurologic compromised osteoporotic fracture[J]. Spine(Phila Pa 1976),2003,28(1):2170-2175. [11] Klotzbuecher C M,Ross P D,Landsmen P B,el at. Patients with prior fractures have an increased risk of future fracture:a summary of the literature and statistical synthesis[J]. J Bone Miner Res,2000,15(4):721-739. [12] Matsuyama Y,Goto M,Yoshihara H,et al. Vertebral reconstruction with biodegradable calcium phosphate cement in the treatment of osteoporotic vertebral compression fracture using instrumentation[J]. J Spinal Disord Tech,2004,17(4):291-296. doi: 10.1097/01.bsd.0000097253.54459.a6 [13] Zhang X,Hu W,Yu J,et al. An effective treatment option for kümmell disease with neurological deficits:modified transpedicular subtraction and disc osteotomy combined with long-segment fixation[J]. Spine,2016,41(15):923-930. doi: 10.1097/BRS.0000000000001467 [14] 吴晓淋,相宏飞,张国庆,等. 骨质疏松性椎体骨折椎体成形术术后处理策略和内固定翻修适应症研究[J]. 中华创伤骨科杂志,2019,21(8):649-657. doi: 10.3760/cma.j.issn.1671-7600.2019.08.002 [15] Lee S H,Kim E S,Eoh W. Cement augmented anterior reconstruction with short posterior instrumentation:a less invasive surgical option for Kummell's disease with cord compression[J]. J Clin Neurosci,2011,18(4):509-514. doi: 10.1016/j.jocn.2010.07.139 [16] Hsieh J Y,Wu C D,Wang T M. Reduction of the domino effect in osteoporotic vertebral compression fractures through short-segment fixation with intravertebral expandable pillars compared to percutaneous kyphoplasty:a case control study[J]. BMC Musculoskelet Disord,2013,2(14):1471-2474. [17] Huang Y S,Hao D J,Wang X D,et al. Long-segment or bone cement-augmented short-segment fixation for kummell disease with neurologic deficits a comparative cohort study[J]. World Neurosurg,2018,116(8):1079-1086. [18] Kim H S,Heo D H. Percutaneous pedicle screw fixation with polymethylmethacrylate augmentation for the treatment of thoracolumbar intravertebral pseudoarthrosis associated with kummell's osteonecrosis[J]. Biomed Res Int,2016,16(10):1104-2209. [19] Machino M,Yukawa Y,Ito K,et al. Posterior/anterior combined surgery for thoracolumbar burst fractures—posterior instrumentation with pedicle screws and laminar hooks,anterior decompression and strut grafting[J]. Spinal Cord,2010,49(4):573-579. -






 下载:
下载: