Lymph Node Metastasis of Mixed Early Gastric Cancer and Its Influence on Prognosis
-
摘要:
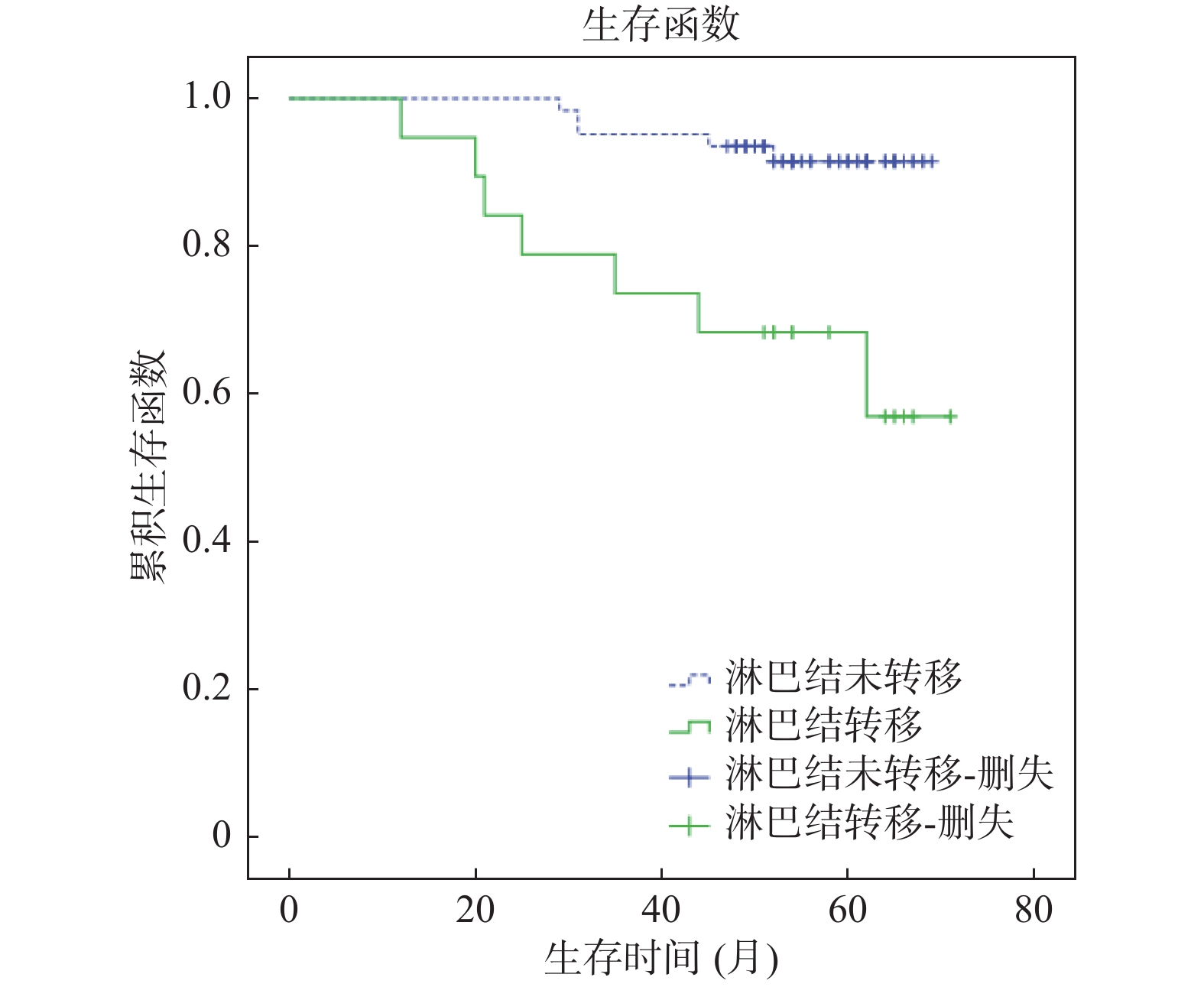
目的 探讨混合型早期胃癌淋巴结转移的规律以及淋巴结转移对远期预后的影响。 方法 选取2014年1月到2016年1月上海交通大学医学院附属苏州九龙医院收治的87例混合型早期胃癌患者作为研究对象,均接受手术治疗。对患者进行随访,观察总生存时间(OS),分析混合型早期胃癌淋巴结转移的规律以及淋巴结转移对OS影响。 结果 87例混合型早期胃癌患者中,20例淋巴结转移,67例未转移,淋巴结转移率为22.99%。淋巴结转移患者肿瘤直径、淋巴管受累率、黏膜下层比例、溃疡型比例高于非淋巴结转移患者,差异有统计学意义(P < 0.05)。Logistic分析结果显示,浸润深度、淋巴管受累、肿瘤大小是混合型组淋巴结转移的影响因素(P < 0.05)。随访时间48~72个月,平均随访时间(62.8±4.8)个月,失访6例,患者3 a生存率为90.1%,5 a生存率为86.4%。Kaplan-Meier法并Log-rank检验显示,混合型组淋巴结转移患者OS短于非淋巴结转移患者(P < 0.05)。Cox分析结果显示,淋巴管受累、淋巴结转移、血管受累、浸润深度是混合型早期胃癌患者生存的独立影响因素(P < 0.05)。 结论 混合型早期胃癌淋巴结转移率高,肿瘤直径大、浸润黏膜下层、淋巴管受累患者淋巴结转移风险增高,且淋巴结转移患者预后差,死亡率高。 Abstract:Objective To investigate the regularity of lymph node metastasis in mixed early gastric cancer and its effect on long-term prognosis. Methods Eighty-seven patients with mixed early gastric cancer admitted to Suzhou Jiulong Hospital, Shanghai Jiaotong University School of Medicine from January 2014 to January 2016 were selected as the research objects. All patients received surgery. The patients were followed up to observe the overall survival time (OS) and the regularity of lymph node metastasis in early gastric cancer and the effect of lymph node metastasis on OS were analyzed. Results Among the 87 patients with mixed early gastric cancer, 20 had lymph node metastasis and 67 had no metastasis. The lymph node metastasis rate was 22.99%. Patients with lymph node metastasis had higher tumor diameter, lymphatic involvement rate, submucosal ratio, and ulcer type than those with non-lymph node metastasis, the differences were statistically significant (P < 0.05). Logistic analysis showed that the depth of infiltration, lymphatic involvement, and tumor size were the influencing factors of lymph node metastasis in Mixed group (P < 0.05). The follow-up time was 48~72 months. The average follow-up time was (62.8 ± 4.8) months. Six patients were lost to follow-up. The 3-year survival rate was 90.1%, and the 5-year survival rate was 86.4%. Kaplan-Meier method and Log-rank test showed that the survival time of patients with lymph node metastasis was shorter than that of patients with non-lymph node metastasis (P < 0.05). Cox analysis showed that lymphatic involvement, lymph node metastasis, vascular involvement, and depth of invasion were independent factors affecting the survival of patients with mixed early gastric cancer (P < 0.05). Conclusions Lymph node metastasis rate of mixed early gastric cancer is high. Patients with large tumor diameter, submucosa, and lymphatic involvement have an increased risk of lymph node metastasis. Patients with lymph node metastasis have a poor prognosis and a high mortality rate. -
Key words:
- Early period /
- Mixed type /
- Lymph node metastasis /
- Overall survival
-
表 1 混合型早期胃癌淋巴结转移与临床病理因素的相关性[n(%)]
Table 1. The correlation between lymph node metastasis of mixed early gastric cancer and clinicopathological factors[n(%)]
项目 淋巴结
转移非淋巴结
转移χ2 P 年龄 0.000 0.986 ≥ 60岁 9(23.08) 30(76.92) < 60岁 11(22.92) 37(77.00) 性别 0.382 0.536 男 11(20.75) 42(79.25) 女 9(26.47) 25(73.53) 浸润深度 8.310 0.004* 黏膜下层 12(41.38) 17(58.62) 黏膜层 8(13.79) 50(86.21) 肿瘤位置 0.035 0.851 上三分之一 7(21.88) 25(78.12) 中下三分之一 13(23.64) 42(76.36) 肿瘤大小 3.942 0.047* ≥ 2.0 cm 9(37.50) 15(62.50) < 2.0 cm 11(17.46) 52(82.54) 淋巴管受累 23.387 < 0.001* 是 14(58.33) 10(41.67) 否 6(9.52) 57(90.48) 血管受累 0.000 0.990 是 6(23.08) 20(76.92) 否 14(22.95) 47(70.15) 溃疡型 6.021 0.014* 是 12(37.50) 20(62.50) 否 8(14.55) 47(85.45) 神经受累 0.492 0.483 是 5(29.41) 12(70.59) 否 15(21.43) 55(78.57) 注:*P < 0.05。 表 2 淋巴结转移的影响因素分析
Table 2. Analysis of influencing factors of lymph node metastasis
项目 OR P 95%CI 浸润深度(黏膜下层/黏膜层) 2.103 0.002 1.661~10.231 淋巴管受累(是/否) 1.556 0.008 1.223~9.324 肿瘤大小(≥ 2.0 cm/< 2.0 cm) 1.521 0.010 1.205~9.221 表 3 Cox单因素分析
Table 3. Single factor analysis of Cox
项目 HR P 95%CI 年龄 1.023 0.102 0.661~1.232 性别 0.859 0.208 0.223~1.324 浸润深度 1.356 0.036 1.035~4.021 肿瘤位置 0.961 0.098 0.882~1.657 肿瘤大小 1.223 0.069 0.884~3.247 淋巴结转移 2.365 0.001 1.339~10.235 淋巴管受累 2.015 0.010 1.225~6.399 血管受累 1.236 0.023 1.023~4.228 溃疡型 0.991 0.125 0.548~2.315 神经受累 0851 0.223 0.442~2.011 表 4 Cox多因素分析
Table 4. Multi-factor analysis of Cox
项目 HR P 95%CI 浸润深度 1.205 0.040 1.055~3.229 淋巴结转移 2.052 0.002 1.139~8.527 淋巴管受累 1.259 0.025 1.105~6.302 血管受累 1.231 0.030 1.023~3.200 -
[1] Rahman R,Asombang A W,Ibdah J A. Characteristics of gastric cancer in Asia[J]. World J Gastroenterol,2014,20(16):4483-4490. doi: 10.3748/wjg.v20.i16.4483 [2] 王昕宇. 主动脉旁淋巴结清扫术在进展期胃癌治疗中的研究进展[J]. 天津医科大学学报,2021,27(1):99-102. [3] 杨亚俊,胡卫敏,史英. 临床病理学因子及生物标记物对早期胃癌淋巴结转移的临床评估价值分析[J]. 现代消化及介入诊疗,2020,25(3):345-349. [4] 梁寒. 远端局部进展期胃癌肠系膜上静脉旁淋巴结(No. 14v)清扫的临床意义[J]. 腹部外科,2020,33(1):1-3. [5] Birkman E M,Mansuri N,Kurki S,et al. Gastric cancer:immunohistochemical classification of molecular subtypes and their association with clinicopathological characteristics[J]. Virchows Arch,2018,472(3):369-382. doi: 10.1007/s00428-017-2240-x [6] 陈丽红,薛蕴菁,段青,等. 不同病理类型和分化程度胃癌宝石CT能谱曲线及CT值的比较[J]. 中华肿瘤杂志,2019,41(5):363-367. [7] 吴俊辉,许美权,温文. 早期胃癌的组织学类型和淋巴结微转移分析[J]. 中国医疗前沿(上半月),2011,6(3):10-11. [8] 陈健,闫滢,钱小军,等. 基于临床病理特征构建胃癌根治术后早期复发风险预测模型[J]. 武警医学,2019,30(9):776-779,783. [9] 王云,张伟锋,司新敏,等. 黏膜内混合型胃癌内镜表现特点的回顾性分析[J]. 中华消化内镜杂志,2019,36(12):944-946. [10] Rocken C. Molecular classification of gastric cancer[J]. Expert Rev Mol Diagn,2017,17(3):293-301. doi: 10.1080/14737159.2017.1286985 [11] 陈建江,赵于天,张晓军,等. 混合型进展期胃癌术后放化疗的 临床观察[J]. 临床肿瘤学杂志,2019,24(12):1130-1133. [12] Bausys R,Bausys A,Vysniauskaite I,et al. Risk factors for lymph node metastasis in early gastric cancer patients:Report from Eastern Europe country- Lithuania[J]. BMC Surg,2017,17(1):108. doi: 10.1186/s12893-017-0304-0 [13] 宋红杰,唐建荣,张逸强. 早期胃癌诊断中NBI技术与放大内镜的应用效果对比[J]. 实用癌症杂志,2019,34(4):637-639. [14] 早期胃癌内镜治疗利与弊[J]. 中国实用外科杂志, 2019, 39(5): 470-472. [15] 张文静,吴克俭,谭宁平. 早期胃癌淋巴结转移的危险因素及预后分析[J]. 中国中西医结合消化杂志,2020,28(5):331-337. [16] 张竞尧,田艳涛,王成锋,等. 早期胃癌内镜黏膜下剥离术后腹腔镜补救手术的临床分析[J]. 北京医学,2020,42(4):279-282. [17] 白斌,蔡慧,聂明明,等. 影响早期胃癌淋巴结转移相关因素分析[J]. 中国实用外科杂志,2019,39(5):476-479. [18] 郝丽莉. 早期胃癌的临床病理特征及发生淋巴结转移的危险因素研究[J]. 中国现代药物应用,2021,15(4):13-15. [19] 崔金朵,丁伟群,钟良,等. 早期胃癌淋巴结转移的影响因素分析[J]. 中华消化内镜杂志,2019,36(11):839-842. [20] 庄阳辉,康争春,王海棠,等. 早期胃癌淋巴结转移差异表达基因分析[J]. 中国临床医学,2019,26(4):555-560. [21] 东强,曲丽洁,张宏,等. 双能量CT碘值对进展期胃癌病理组织类型及浆膜外脂肪侵犯的诊断价值[J]. 现代医学,2019,47(9):1099-1104. [22] 李彦,刘会永. 早期胃癌在白光内镜下的特征及其与病理类型的关系[J]. 实用癌症杂志,2018,33(2):290-293. [23] 庞博然,朱正伦,李琛,等. 早期低分化胃癌淋巴结转移危险因素分析[J]. 中华胃肠外科杂志,2019,22(5):446-450. [24] 刘朋伟,何池义. 混合型早期胃癌淋巴结转移危险因素分析[J]. 皖南医学院学报,2020,39(3):238-241. [25] 武颖超,谢淼,蔡云龙,等. 早期胃癌淋巴结转移规律及其预后分析[J]. 中华普通外科杂志,2019,34(7):561-564. doi: 10.3760/cma.j.issn.1007-631X.2019.07.001 [26] 周潮平,汤代彬,汪大田,等. 单中心186例早期胃癌区域淋巴结转移特征与预后分析[J]. 中国普通外科杂志,2019,28(10):1221-1227. [27] Mikami K,Hirano Y,Futami K,et al. Expansion of lymph node metastasis in mixed-type submucosal invasive gastric cancer[J]. Asian J Surg,2018,41(5):462-466. doi: 10.1016/j.asjsur.2017.04.004 [28] Chen Y C,Fang W L,Wang R F,et al. Clinicopathological variation of lauren classification in gastric cancer[J]. Pathol Oncol Res,2016,22(1):197-202. doi: 10.1007/s12253-015-9996-6 [29] 徐俊,张恩勇,罗天航,等. 早期胃混合型印戒细胞癌的临床病理因素分析[J]. 实用肿瘤学杂志,2016,30(5):414-419. [30] 徐策. 腹腔镜与开腹胃癌根治术治疗早期胃癌的预后与生存率分析[J]. 中国现代普通外科进展,2019,22(6):450-453. [31] 况丽平,詹晓芬,赵勇强,等. 潮汕地区902例胃癌原发病灶中表皮生长因子受体2表达及其临床意义[J]. 实用医学杂志,2017,33(20):3452-3454. [32] 高洪宇,张明,魏玉哲,等. BorrmannⅣ型胃癌生物学行为特点及预后[J]. 中华普通外科杂志,2011,26(1):65-66. -






 下载:
下载: