Effects of Different Ventilation Modes on PaO2 and Lactic Acid in Arterial Blood of Upper and Lower Limbs in Rectal Cancer Patients under Trendelenburg Posture
-
摘要:
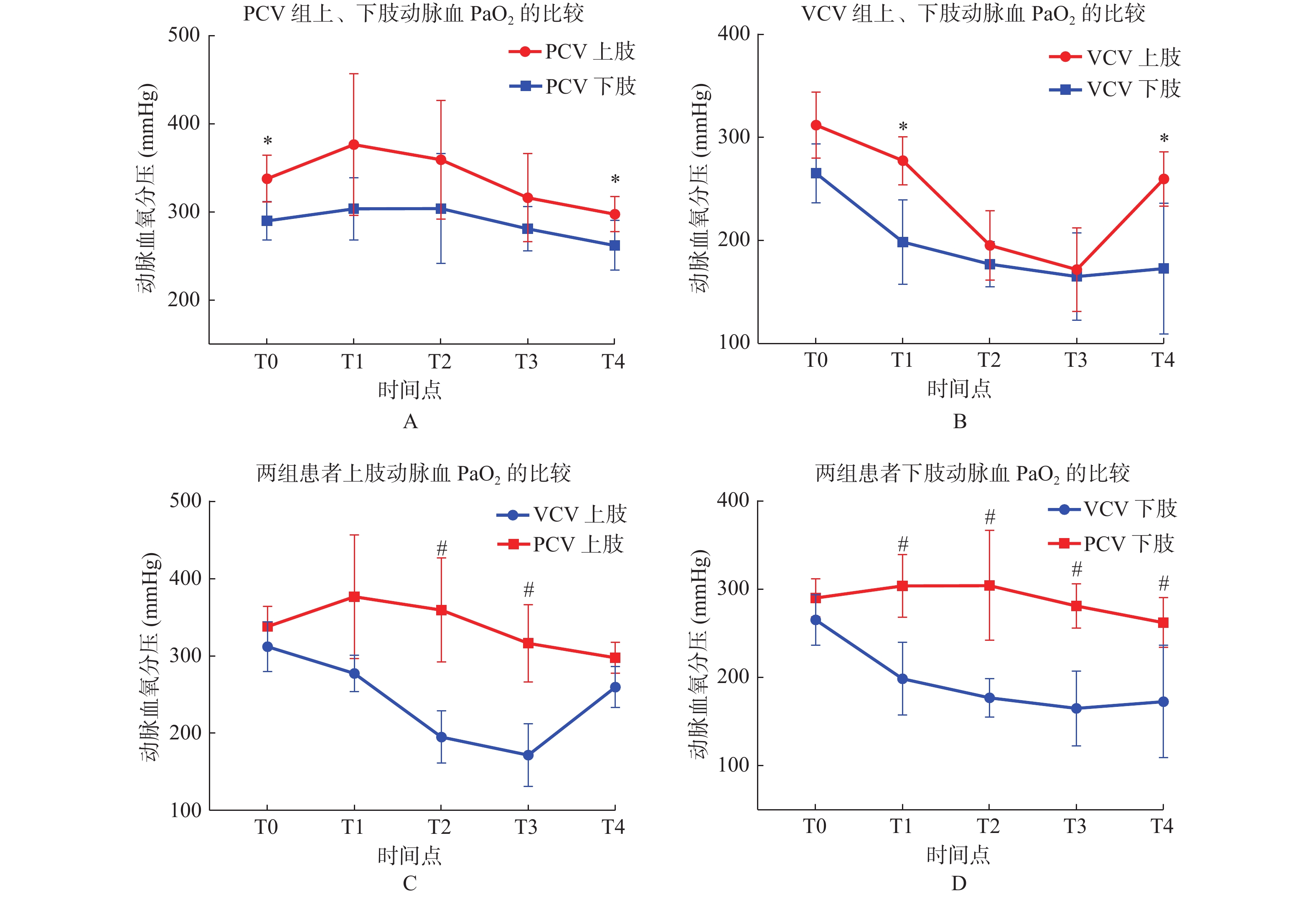
目的 探讨Trendelenburg体位下不同通气模式对直肠癌患者围术期上、下肢动脉PaO2、及血乳酸的变化,为合理实施围术期机体功能保护策略提供依据及参考。 方法 选择40例行择期腹腔镜下直肠癌根治术患者,随机数字法分成2组:容量控制通气组(VCV组);压力控制通气组(PCV组),每组20例,观察比较Trendelenburg体位下2种通气模式对直肠癌患者不同时间点同侧上下肢动脉血PaO2及血乳酸值的变化。 结果 2组患者上肢动脉血氧分压较下肢高,VCV组T1、T4时,上、下肢动脉氧分压,差异有统计学意义(P < 0.05);PCV组T0、T4时,上、下肢动脉氧分压,差异有统计学意义(P < 0.05)。PCV组患者上下肢动脉血氧分压均较VCV组高,2组T2、T3时,上肢动脉氧分压,差异有统计学意义(P < 0.05);2组T1-4时,下肢动脉氧分压,差异有统计学意义(P < 0.05)。与T0时点比较,VCV组上肢T2-4时点,氧分压明显下降,下肢T1-4时点,动脉氧分压明显下降,差异有统计学意义(P < 0.05);PCV组上、下肢在T5时点,动脉氧分压下降,差异有统计学意义(P < 0.05)。2组患者上肢动脉血乳酸较下肢低,VCV组T2、T4时,上、下肢动脉血乳酸值,差异有统计学意义(P < 0.05);PCV组T3时,上、下肢动脉血乳酸值,差异有统计学意义(P < 0.05)。PCV组患者上下肢动脉血乳酸均较VCV组低,PCV组T0、T2、T3时,下肢动脉血乳酸明显低于VCV组,差异有统计学意义(P < 0.05)。与T0时点比较,2组上、下肢T1-4时点,动脉血乳酸均升高,差异有统计学意义(P < 0.05)。 结论 围术期采用PCV通气模式,在提高动脉血PaO2及降低血乳酸值,改善组织灌注方面更具优势,对下肢改善效果更为突出,能够减轻Trendelenburg体位对患者机体的不利影响。 -
关键词:
- Trendelenburg体位 /
- 通气模式 /
- 动脉血氧分压 /
- 乳酸
Abstract:Objective To investigate the changes of upper and lower limb artery PaO2 and blood lactic acid in rectal cancer patients with different ventilation modes in Trendelenburg position during perioperative period, so as to provide basis and reference for the reasonable implementation of perioperative body function protection strategy. Methods Forty patients underwent elective laparoscopic radical resection of rectal cancer were randomly divided into two groups: volume control ventilation group (VCV group, 20 cases) and pressure control ventilation group (PCV group, 20 cases). In each group, the changes of PaO2 and blood lactic acid in the ipsilateral upper and lower limbs of patients with rectal cancer at different time points were observed and compared under Trendelenburg position. Results The PaO2 of the upper limbs was higher than that of the lower limbs in the two groups. In the VCV group, there was statistically significant difference in PaO2 in the arteries of upper and lower limbs at T1 and T4 (P < 0.05). In PCV group, there was statistically significant difference in PaO2 of upper and lower limb arteries at T0 and T4 (P < 0.05). PaO2 in the upper and lower extremity arterial blood of PCV group was higher than that of VCV group, and the difference of PaO2 in the upper extremity artery at T2 and T3 between the two groups was statistically significant (P < 0.05).The difference of lower limb artery PaO2 between the two groups at T1-4 was statistically significant (P < 0.05). Compared with T0 time point, PaO2 in the upper extremity of VCV group was significantly decreased at T2-4 time point, and that in the lower extremity of VCV group was significantly decreased at T1-4 time point, the difference was statistically significant (P < 0.05). In the PCV group, the upper and lower limbs arterial PaO2 decreased at T5, and the difference was statistically significant (P < 0.05). The levels of arterial lactic acid in upper limbs were lower than those in lower limbs in 2 groups, and there was statistical significance in the values of arterial lactic acid in upper and lower limbs in VCV group at T2 and T4 (P < 0.05). There was statistically significant difference in arterial lactic acid value of upper and lower limbs in PCV group at T3 (P < 0.05). The arterial lactic acid in the upper and lower limbs of the PCV group was lower than that of the VCV group, and the arterial lactic acid in the lower limbs of the PCV group was significantly lower than that of the VCV group at T0, T2 and T3, with statistical significance (P < 0.05). Conclusion PCV ventilation mode in perioperative period has more advantages in improving arterial blood PaO2, reducing blood lactic acid, improving tissue perfusion. The advantages of PCV were more prominent in the lower limbs which can reduce the adverse effect of Trendelenburg posture on patients. -
表 1 2组患者一般资料比较(
$\bar x \pm s $ )Table 1. Comparison of general information of two groups (
$\bar x \pm s $ )项目 VCV组 PCV组 χ2/t P 例数(n) 20 20 − − 年龄(岁) 53.67 ± 5.96 54.21 ± 4.86 0.1449 0.8856 性别(男/女) 14/6 15/5 0.0125 0.7232 体重(kg) 65.80 ± 7.20 68.07 ± 8.55 0.3946 0.4952 体重指数(kg/m2) 21.82 ± 2.31 22.01 ± 2.46 0.4876 0.4354 气腹压力(mmHg) 12.05 ± 2.13 12.53+1.78 0.2968 0.7654 气腹时间(min) 125.67 ± 15.56 120.32 ± 19.21 0.3013 0.156 表 2 2组患者不同时间点上、下肢动脉血氧分压的比较[(
$\bar x \pm s$ ),mmHg]Table 2. Comparison of arterial PaO2 of upper and lower limbs in two groups at different time points [(
$\bar x \pm s$ ),mmHg]组别 项目 部位 T0 T1 T2 T3 T4 VCV组 PaO2 上肢 312.12 ± 32.07 277.34 ± 23.33 195.12 ± 33.73a 171.45 ± 40.52a 259.69 ± 26.36a 下肢 265.20 ± 28.60 198.50 ± 41.10*a 177.00 ± 21.78a 165.00 ± 42.41a 172.65 ± 63.65*a PCV组 PaO2 上肢 338.01 ± 26.54 376.75 ± 80.14 359.59 ± 67.21# 316.51 ± 50.03# 297.75 ± 19.87a 下肢 290.25 ± 21.76* 303.75 ± 35.40# 304.25 ± 62.33# 281.25 ± 25.10# 262.25 ± 28.19*#a 组内与上肢比较,*P < 0.05;与VCV组比较,#P < 0.05;与T0比较,aP < 0.05。 表 3 2组患者不同时间点上、下肢动脉血乳酸的比较[(
$\bar x \pm s$ ),mmHg]Table 3. Comparison of blood lactic acid in upper and lower extremity arteries at different time points between the two groups [(
$\bar x \pm s$ ),mmHg]组别 部位 T0 T1 T2 T3 T4 VCV组 上肢 1.22 ± 0.16 1.95 ± 0.25a 2.08 ± 0.27a 2.75 ± 0.52a 2.69 ± 0.56a 下肢 1.45 ± 0.20 2.27 ± 0.41a 2.75 ± 0.38*a 3.50 ± 0.75a 3.65 ± 0.65*a PCV组 上肢 0.90 ± 0.14 1.50 ± 0.24a 1.83 ± 0.47a 2.26 ± 0.53a 2.25 ± 0.51a 下肢 1.15 ± 0.26# 1.87 ± 0.40a 2.35 ± 0.43*#a 2.75 ± 0.52#a 3.05 ± 0.619*a 组内与上肢比较,*P < 0.05;与VCV组比较,#P < 0.05;与T0比较,aP < 0.05。 -
[1] Shibata R,Sato K,Pimentel D R,et al. Adiponectin protects against myocardial ischemia-reperfusion injury through AMPK and COX-2-dependent mechanisms[J]. Nature Medicine,2005,11(10):1096-1103. doi: 10.1038/nm1295 [2] 吴耀滨,谭艺平,朱海滨,等. PCV-VG和VCV模式对Trendelenburg体位下腹腔镜手术通气功能的影响研究[J]. 岭南现代临床外科,2020,20(4):512-516. doi: 10.3969/j.issn.1009-976X.2020.04.024 [3] 朱泽飞,孙振涛,杨贯宇,等. 长时间CO2气腹和Trendelenburg体位对中老年患者直肠癌根治术中脑氧饱和度的影响[J]. 临床麻醉学杂志,2020,36(2):152-155. [4] 李铁,王曙光,刘永诚. 腹腔镜胆囊切除术中气腹压力不同对人体肝脏功能的影响[J]. 中华肝胆外科杂志,2001,7(7):387-390. doi: 10.3760/cma.j.issn.1007-8118.2001.07.001 [5] 王斌. 长时间腹腔镜手术腹腔脏器缺血/再灌注损伤与防治的临床研究[D]. 西安: 第四军医大学硕士学位论文, 2017. [6] He X,Bi X Y,Wang H,et al. Progress in calcium regulation in myocardial and vascular ischemia-reperfusion injury[J]. Sheng Li Xue Bao[Acta physiologica Sinica],2012,64(3):321. [7] 张云亮,李皓,米卫东,等. Trendelenburg体位下人工气腹对老年患者局部脑氧饱和度及颅内压影响的研究[J]. 北京医学,2019,41(8):637-640. [8] 邓立云,王原芬,赵嘉训. 低位硬膜外麻醉上下肢SPO2监测的临床观察[J]. 山西医药杂志,2000,2(29):136-137. [9] 孙树俊,姜艳华,刘海梅,等. Trendelenburg体位人工气腹对压力控制通气预设气道压改变引起呼吸力学指标变化的影响[J]. 实用医学杂志,2018,34(2):209-211. doi: 10.3969/j.issn.1006-5725.2018.02.012 [10] 姚静,代元大,林财珠. 不同通气模式对Trendelenburg体位腹腔镜手术患者PaO2和PaCO2的影响[J]. 临床麻醉学杂志,2016,4(34):347-350. [11] 熊继君,阳子华,蒋洪宇. Trendelenburg体位对腹腔镜直肠癌患者的影响[J]. 广东医药,2016,4(37):587-590. [12] 赵兵,张在旺,李景娅,等. 不同体位腹腔镜手术对肥胖患者呼吸循环功能的影响[J]. 医学理论与实践,2019,32(16):2592-2594. [13] 王情,冯艳婕,张仙儒,等. 不同气腹压力及截石位改变速度对妇科腹腔镜手术患者循环和气血的影响[J]. 中国妇幼保健,2017,32(19):4639-4642. [14] 谢淑华,耿立成,高涛,等. 不同角度头低位对腹腔镜直肠癌根治术中患者呼吸力学和脑循环胡影响[J]. 中华麻醉学杂志,2014,8(34):959-961. [15] 王瀚冰,李广华,高伟,等. 单肺通气时应用PEEP和CPAP对开胸手术患者呼吸功能的影响[J]. 哈尔滨医科大学学报,2020,54(6):621-624. [16] 徐明霞,张静,赵婉璐,等. 呼气末正压肺保护性通气策略在超重患者腹腔镜手术中的应用[J]. 中国医师杂志,2020,22(5):674-677. doi: 10.3760/cma.j.cn431274-20190320-00302 -






 下载:
下载: