Feasibility Analysis of the NOSAS Score as A Screening Tool for Obstructive Sleep Apnea in the Physical Examination Population
-
摘要:
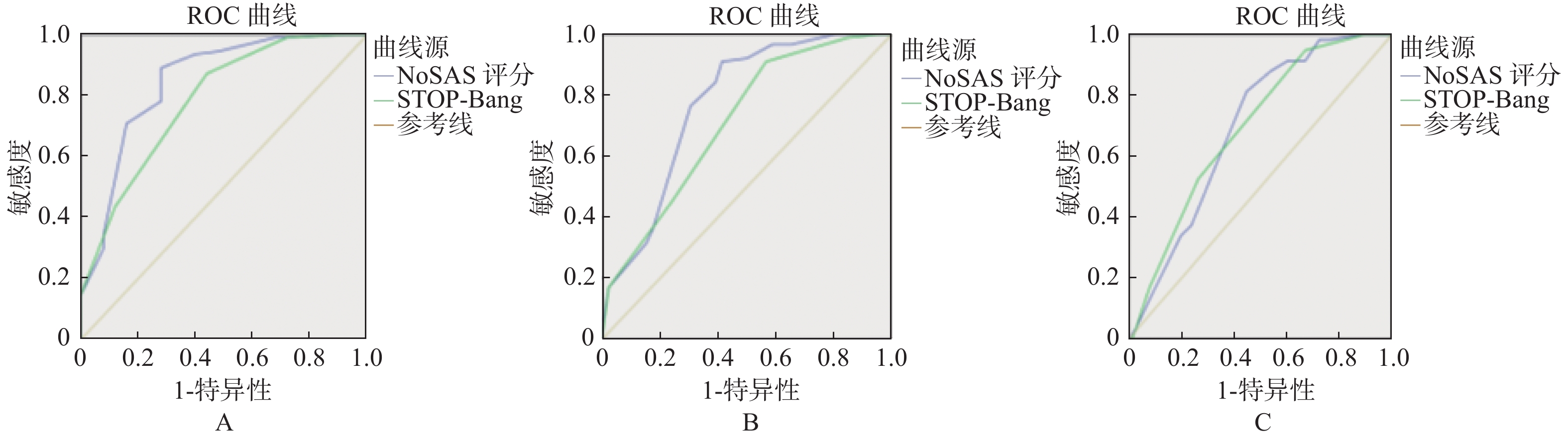
目的 比较NOSAS评分与STOP-Bang问卷的预测值,对体检人群使用NOSAS评分作为OSAHS初步筛查工具的可行性进行探讨。 方法 回顾性分析2018年1月至2019年8月来北京航天总医院健康管理中心疑似OSAHS患者135例的多导睡眠图(PSG)监测结果,包括NOSAS评分及STOP-Bang问卷各项目及患者资料。按呼吸暂停低通气指数(AHI)分组。计算NOSAS评分和Stop-Bang问卷的敏感度、特异性、阳性预测值和阴性预测值,并绘制ROC曲线。比较2个评分筛查OSAHS的价值。 结果 在135例患者中,男性占75.6%,女性占24.4%。以AHI ≥ 5次/h、15次/h、30次/h为诊断标准,NOSAS评分敏感度和特异性分别为:0.891和0.720、0.910和0.587、0.814和0.553;STOP-Bang问卷的敏感性和特异性分别为:0.873和0.560、0.910和0.435、0.949和0.329。当以AHI ≥ 5次/h、15次/h、30次/h为诊断标准,NOSAS评分ROC曲线下面积分别为:0.847、0.773、0. 693,差异有统计学意义(P < 0.001);STOP-Bang问卷的ROC曲线下面积分别为:0.784、0.711、0.694,差异有统计学意义(P < 0.001)。以AHI为5次/h、15次/h及30次/h为临界点时,NOSAS评分ROC曲线下面积大于或等于STOP-Bang问卷评分。NOSAS评分具有良好的预测价值。 结论 NOSAS评分作为一种简单有效的初筛工具,在健康体检人群可有效的帮助医师快速筛查OSAHS患病高风险者。 -
关键词:
- 阻塞性睡眠呼吸暂停 /
- OSAHS /
- NOSAS评分 /
- STOP-Bang问卷
Abstract:Objective To compare the predictive value of NoSAS score and STOP-Bang questionnaire score, and evaluate the feasibility of NoSAS score screening for OSAHS in physical examination population. Methods Retrospective analysis of the polysomnography (PSG) monitoring results of 135 patients with suspected OSAHS in our health management center was made from January 2018 to August 2019, including the NOSAS score and the Stop Bang Questionnaire and patient information. Grouped by apnea-hypopnea index (AHI), the sensitivity, specificity, positive predictive value and negative predictive value of NOSAS score and Stop-Bang questionnaire score were calculated, and ROC curves were drawn so as to compare the effectiveness of two scores which screened OSAHS. Result Of the 135 patients, 75.6% were male and 24.4% were female. Using AHI ≥ 5 events/h, AHI ≥ 15 events/h and AHI ≥ 30 events/h as the diagnostic criteria, the sensitivity and specificity of NOSAS scores were: 0.891 and 0.720, 0.910 and 0.587, 0.814, and 0.553; The sensitivity and specificity of STOP-Bang questionnaire were 0.873 and 0.560, 0.910 and 0.435, 0.949 and 0.329, respectively. When AHI ≥ 5 events/h, AHI ≥ 15 events/h and AHI ≥ 30 events / h were used as diagnostic criteria, the areas under ROC curveofthe NoSAS score were 0.847, 0.773 and 0.693, the difference was statistically significant (P < 0.001); the areas under the ROC curve of the STOP-Bang questionnaire were 0.784, 0.711, 0.694 and the differences were statistically significant (P < 0.001). When AHI is 5 events/h, 15 events/h and 30 events/h as the critical points, the area under the NOSAS score ROC curve is greater than or equal to the STOP-Bang questionnaire score. The NOSAS score has good predictive value. Conclusion As a simple and effective initial screening tool, the NOSAS score can effectively help physicians quickly screen OSAHS patients in physical examination population. -
表 1 北京航天总医院135例患者资料(
$\bar x \pm s$ )Table 1. Beijing aerospace general hospital 135 patient data (
$ \bar x \pm s$ )项目 正常组 轻度OSAHS组 中度OSAHS组 重度OSAHS组 P 例数 25 21 30 59 男性(n) 14 16 26 46 吸烟[n(%)] 6(24) 9(42.9) 16(53.3) 32(54.2) 0.064 年龄(岁) 48.4 ± 12.3 50.1 ± 10.7 53.8 ± 10.9 50.1 ± 10.9 0.311 BMI(kg/m2) 25.64 ± 4.25 26.88 ± 4.27 26.37 ± 5.56 28.77 ± 3.59 < 0.001 颈围(cm) 38.10 ± 4.49 39.82 ± 4.83 41.22 ± 3.53 42.65 ± 3.4 < 0.001 睡前收缩压(mmHg) 131.56 ± 15.65 129.29 ± 12.66 131.30 ± 13.24 134.64 ± 14.54 0.418 醒后收缩压(mmHg) 129.24 ± 15.65 131.00 ± 15.15 133.90 ± 14.16 140.88 ± 14.12 0.003* AHI(次/h) 2.39 ± 1.51 8.84 ± 2.48 21.37 ± 4.07 51.07 ± 19.96 < 0.001 最长呼吸暂停时间(s) 19.84 ± 22.62 30.45 ± 16.78 43.57 ± 20.70 64.75 ± 30.47 < 0.001 最低夜间血氧饱和度(%) 87.56 ± 6.27 85.90 ± 4.33 81.03 ± 6.95 69.22 ± 11.59 < 0.001 NoSAS(分) 5.44 ± 3.82 9.00 ± 3.65 10.93 ± 3.25 11.39 ± 2.64 < 0.001 STOP-Bang(分) 2.20 ± 1.15 3.14 ± 0.91 3.30 ± 1.09 3.64 ± 0.83 < 0.001 *P < 0.05。 表 2 NOSAS评分和STOP-Bang问卷在AHI ≥ 5次/h时的预测值
Table 2. Predictive value of NOSAS score and STOP-Bang questionnaire at AHI ≥ 5 events /h
量表 曲线下面积(95%CI) 敏感度(95%CI) 特异性(95%CI) 阳性预测值(95%CI) 阴性预测值(95%CI) NOSAS 0.847(77.5~90.3) 0.891(81.7~94.2) 0.720(50.6~87.9) 0.933(88.2~96.3) 0.60(45.5~73.0) STOP-Bang 0.784(70.5~85.0) 0.873(79.6~92.9) 0.560(34.9~75.6) 0.897(84.8~93.2) 0.50(35.4~64.6) 表 3 NOSAS评分和STOP-Bang问卷在AHI ≥ 15次/h时的预测值
Table 3. Predictive value of NOSAS score and STOP-Bang questionnaire at AHI ≥ 15 events /h
量表 曲线下面积(95%CI) 敏感度(95%CI) 特异性(95%CI) 阳性预测值(95%CI) 阴性预测值(95%CI) NOSAS 0.773(69.3~84.1) 0.910(83.1~96.0) 0.587(43.2~73.0) 0.810(75.0~85.8) 0.771(62.5~87.2) STOP-Bang 0.711(62.6~78.5) 0.910(83.1~96.0) 0.435(28.9~58.9) 0.757(70.6~80.2) 0.714(54.4~84.0) 表 4 NOSAS评分和STOP-Bang问卷在AHI ≥ 30次/h时的预测值
Table 4. Predictive value of NOSAS score and STOP-Bang questionnaire at AHI ≥ 30 events /h
量表 曲线下面积(95%CI) 敏感度(95%CI) 特异性(95%CI) 阳性预测值(95%CI) 阴性预测值(95%CI) NOSAS 0.693(60.8~77.0) 0.814(69.1~90.3) 0.553(43.4~66.7) 0.585(51.7~65.1) 0.792(68.3~87.1) STOP-Bang 0.694(60.8~77.0) 0.949(85.9~98.9) 0.329(22.5~44.6) 0.523(48.1~56.5) 0.893(72.6~96.3) -
[1] 中华医学会. 成人阻塞性睡眠呼吸暂停基层诊疗指南(实践版·2018)[J]. 中华全科医师杂志,2019,18(1):21-29. doi: 10.3760/cma.j.issn.1671-7368.2019.01.007 [2] 何权瀛. 肥胖对呼吸系统的危害及对策[J]. 中华健康管理学杂志,2011,5(6):321-322. doi: 10.3760/cma.j.issn.1674-0815.2011.06.001 [3] 中国超重/肥胖医学营养治疗专家共识编写委员会. 中国超重/肥胖医学营养治疗专家共识(2016年版)[J]. 糖尿病天地:临床,2016,10(9):395-398. [4] 赵忠新. 睡眠医学[M]. 北京: 人民卫生出版社, 2016: 79. [5] 中华医学会呼吸病学分会睡眠呼吸障碍学组. 阻塞性睡眠呼吸暂停低通气综合征诊治指南(2011年修订版)[J]. 中华结合呼吸杂志,2012,35(1):9-12. [6] Marti-Snler H,Hirntsu C,Marques-Vidal P,et al. The NoSASscore for screening of sleep -disordered breathing:Aderivationandvalidation study[J]. Lancet Respir Med,2016,4(9):742-748. doi: 10.1016/S2213-2600(16)30075-3 [7] Chung F,Yegneswaran B,Liao P,et al. STOP questionnaire:a toolto screen patients for obstructive sleep apnea[J]. Anesthesiology,2008,108(5):812-821. doi: 10.1097/ALN.0b013e31816d83e4 [8] Berry R B,Budhiraja R,Gottlieb D J,et al. Rules for scoring respiratory events in sleep:update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events[J]. J Clin Sleep Med,2012,8(5):597-619. doi: 10.5664/jcsm.2172 [9] 何权瀛. 阻塞性睡眠呼吸暂停的病理生理变化及其临床意义[J]. 中华全科医师杂志,2019,18(7):700-702. doi: 10.3760/cma.j.issn.1671-7368.2019.07.021 [10] 罗金梅,肖毅. 一种简便易行的筛查阻塞性睡眠呼吸暂停低通气综合征的问卷:STOP-Bang问卷[J]. 中华结核和呼吸杂志,2013,38(11):868-870. doi: 10.3760/cma.j.issn.1001-0939.2013.11.025 [11] 潘悦达,王东博,韩德民. 我国成人阻塞性睡眠呼吸暂停低通气综合征患病率的Meta分析[J]. 医学信息,2019,22(7):73-77. doi: 10.3969/j.issn.1006-1959.2019.07.022 [12] Oktay Arslan B, Uçar ZZ, Batum ö, et al. Validation of the NOSAS score for screening sleep-disordered breathing: A sleep clinic- based study in Turkey[J]. Turk J Med Sci,2021,51(1):319-327. [13] 卿思敏,陈日垦,刘恒,等. NoSAS评分与四种量表评估阻塞性睡眠呼吸暂停低通气综合征的应用价值比较[J]. 中华结合和呼吸杂志,2018,41(3):213-219. [14] Peng M,Chen R,Cheng J,et al. Application value of the NoSAS score for screening sleep disordered breathing[J]. J Thorac Dis,2018,10(8):4774-4781. doi: 10.21037/jtd.2018.07.46 [15] Tan A,Hong Y,Tan L W L,et al. Validation of NoSAS score for screening of sleep-disordered breathing in a multiethnic Asian population[J]. Sleep Breath,2017,21(4):1033-1038. doi: 10.1007/s11325-016-1455-4 [16] Coutinho Costa J,Rebelo-Marques A,Machado J N,et al. Validation of NOSAS(Neck,Obesity,Snoring,Age,Sex)score as a screening tool for obstructivesleep apnea:Analysis in a sleep clinic[J]. Pulmonology,2019,25(5):263-270. doi: 10.1016/j.pulmoe.2019.04.004 [17] Cheng Hong,Riken Chen,Simin Qing,et al. Validation of the NoSASscore for the screening of sleep-disordered breathing:ahospital-based retrospective study in China[J]. J Clin Sleep Med,2018,14(2):191-197. doi: 10.5664/jcsm.6930 [18] Duarte R L M,Magalhães-da-Silveira F J,Oliveira-E-Sá T S,et al. Predictingobstructive sleep apnea in patients with insomnia:A comparativestudy with four screening instruments[J]. Lung,2019,197(4):451-458. doi: 10.1007/s00408-019-00232-5 -






 下载:
下载: