Effect of Standardized Management Model on Improving the Quality of Life of Patients with Ankylosing Spondylitis
-
摘要:
目的 运用标准化管理模式对强直性脊柱炎(AS)患者进行系统干预,从而提高患者疾病认知度和生活质量。 方法 本研究选取2018年9月至2019年2月期间住院的100例AS患者为研究对象。按随机分组原则将入组患者分为对照组和实验组各50例,对照组患者提供现有常规护理干预,实验组给予标准化管理模式干预。10个月后将两组患者疾病认知度、生活质量进行比较。 结果 关于疾病认知度和生活质量,对照组干预前后均无明显差异(P < 0.485)。实验组两方面均明显高于干预前(P < 0.05)。 结论 标准化管理模式能显著提高AS患者疾病认知度和生活质量,并且可以有效支持AS患者实现达标治疗,在临床上值得推广。 Abstract:Objective To improve the quality of life of patients, we use systematic intervention with standardized management model to intervene ankylosing spondylitis (AS) to improve the disease awareness and living quality. Methods This study selected 100 patients with ankylosing spondylitis who were hospitalized from September 2018 to February 2019 as the research objects, and they were divided into the control group (50 cases) and the experimental group (50 cases) according to the random grouping principle. During 10 months, the patients in the control group were given routine nursing management, and the patients in the experimental group were given systematic intervention with standardized management model. After 10 months, the two groups were compared. Results The control group had no significant difference in knowledge of disease and quality of life between before and after intervention (P < 0.485). The cognitive status of disease knowledge and quality of life of the experimental group were significantly higher than those in the control group (P < 0.05). Conclusion Systematic intervention with standardized management model can significantly improve the disease awareness and the quality of life of AS patients, and promote their early return to family and society. -
表 1 实验组患者干预前后疾病认知度比较[n(%)]
Table 1. Comparison of disease cognition before and after intervention in the experimental group [n(%)]
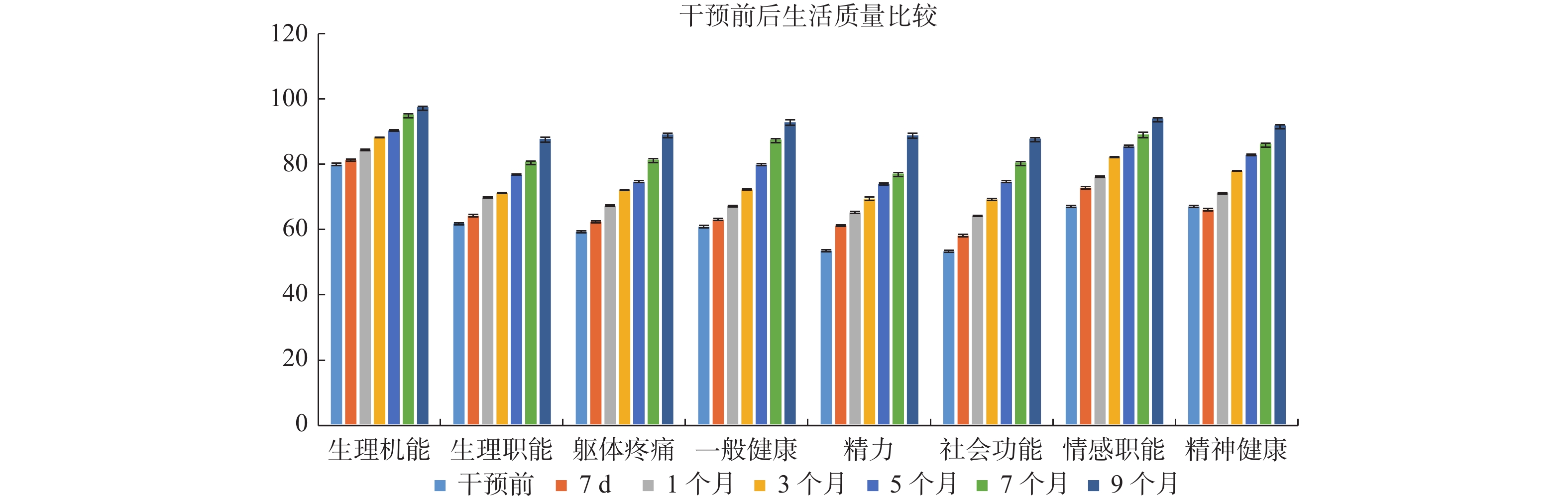
组别 发病诱因 药物疗效观察 疾病活动指标 并发症 功能锻炼 干预前(n = 50) 43(43.00) 23(32.00) 31(31.00) 13(13.00) 37(37.00) 干预后(n = 50) 89(89.00) 92(92.00) 94(94.00) 87(87.00) 93(89.00) 表 2 实验组患者干预前、后生活质量比较(
$\bar x \pm s $ ,分)Table 2. Comparison of quality of life of experimental group patients before and after intervention(
$\bar x \pm s $ , points)项目 n 干预前 7 d 1个月 3个月 5个月 7个月 9个月 生理机能 50 79.91 ± 0.38 81.32 ± 0.31 84.41 ± 0.24 88.23 ± 0.11 90.36 ± 0.21 95.21 ± 0.22 97.53 ± 0.27 生理职能 50 61.82 ± 0.30 64.25 ± 0.35 69.79 ± 0.16 71.23 ± 0.16 76.81 ± 0.19 80.84 ± 0.17 87.81 ± 0.48 躯体疼痛 50 59.31 ± 0.34 62.41 ± 0.31 67.28 ± 0.26 72.11 ± 0.11 74.67 ± 0.28 81.45 ± 0.22 89.17 ± 0.27 一般健康 50 60.91 ± 0.32 63.12 ± 0.33 67.18 ± 0.21 72.26 ± 0.17 79.90 ± 0.26 87.57 ± 0.25 92.90 ± 0.67 精力 50 53.51 ± 0.36 61.23 ± 0.21 65.28 ± 0.27 69.46 ± 0.47 73.96 ± 0.29 77.18 ± 0.22 88.93 ± 0.57 社会功能 50 53.41 ± 0.32 58.13 ± 0.36 64.18 ± 0.14 69.26 ± 0.31 74.69 ± 0.26 80.54 ± 0.23 87.90 ± 0.25 情感职能 50 67.11 ± 0.33 72.83 ± 0.34 76.18 ± 0.27 82.16 ± 0.13 85.50 ± 0.26 89.17 ± 0.62 94.00 ± 0.23 精神健康 50 61.41 ± 0.34 66.13 ± 0.37 71.12 ± 0.24 77.96 ± 0.11 82.90 ± 0.28 86.27 ± 0.22 91.90 ± 0.24 P < 0.05 < 0.05 < 0.05 < 0.05 < 0.05 < 0.05 < 0.05 r 0.913 0.933 0.940 0.954 0.948 0.959 0.980 -
[1] Jeong H, Eun Y H, Kim I Y, et al. Characteristics of hip involve-ment in patients with ankylosing spondylitis in Korea[J]. Korean J Intern Med,2017,32:158-164. doi: 10.3904/kjim.2015.229 [2] Wink F, Arends S, Maas F, et al. High prevalence of hip in-volvement and decrease in inflammatory ultrasound lesions during tumour necrosis factor-alpha blocking therapy in ankylosing spon-dylitis[J]. Rheumatology (Oxford),2019,58:1040-1046. doi: 10.1093/rheumatology/key382 [3] Maatallah K, Mahmoud I, Belghali S, et al. Reparative radiolog-ical changes of hip joint after TNF inhibitors in ankylosing spon-dylitis[J]. Caspian J Intern Med,2018,9:303-305. [4] 郝东梅, 吴范, 高飞, 等. 综合护理干预对强直性脊柱炎患者运动功能的效果分析[J]. 黑龙江科学,2019,10(4):84-85. doi: 10.3969/j.issn.1674-8646.2019.04.040 [5] 吴歆, 徐沪济. 应关注强直性脊柱炎患者身心健康、生活质量和易被忽视的骨质疏松[J]. 诊断学理论与实践,2019,18(1):113-116. [6] 宋雨晴, 陈红. 强直性脊柱炎患者康复护理的研究进展[J]. 中华护理杂志,2016,51(10):1226-1229. doi: 10.3761/j.issn.0254-1769.2016.10.017 [7] 南鹤, 姜珊, 李笑蕾. 强直性脊柱炎患者慢病管理模式的探索及效果研究[J]. 吉林医学,2019,40(7):1650-1652. doi: 10.3969/j.issn.1004-0412.2019.07.124 [8] 胡艺译. 功能锻炼护理对强直性脊柱炎患者康复的影响[J]. 中国社区医师,2019,35(05):159-160. doi: 10.3969/j.issn.1007-614x.2019.05.106 [9] 魏玲, 卞勤英, 李宇飞, 等. 强直性脊柱炎护理措施有效性的预后观察[J]. 中国中医药现代远程教育,2016,14(13):118-119. doi: 10.3969/j.issn.1672-2779.2016.13.054 [10] van der Linden S M, Valkenburg H A, Cat A. Evaluation of diagnostic criteria for ankylosing spondylitis: A Proposal for modification of the New York criteria[J]. Arthritis Rheum,1984,27:361-368. [11] LIANG H, ZHANG H, JI H, et al. Effects of home-based exercise intervention on health-related quality of life for patients with ankylosing spondylitis: a meta-analysis[J]. Clin Rheumatol,2015,34(10):1737-1744. doi: 10.1007/s10067-015-2913-2 [12] 李利平, 孙建萍, 吴红霞. 慢性病患者病耻感的研究现状[J]. 解放军护理杂志,2020,37(3):81-84. [13] 吴燕, 田蓓, 钱君. 冠心病介入术后患者的心理弹性研究进展[J]. 国际病理科学与临床杂志,2020,40(5):1320-1325. [14] 吴清香, 亓英, 周陶, 等. 强直性脊柱炎患者治疗依从性现状及影响因素研究[J]. 中国全科医学,2013,16 (26):3041-3044. doi: 10.3969/j.issn.1007-9572.2013.26.040 [15] DEAN L E, MACFARLANE G J, JONES G T. Differences in the prevalence of ankylosing spondylitis in primary and secondary care: only one-third of patients are managed in rheumatology[J]. Rheumatology(Oxford),2016,55(10):1820-1825. doi: 10.1093/rheumatology/kew228 -






 下载:
下载: