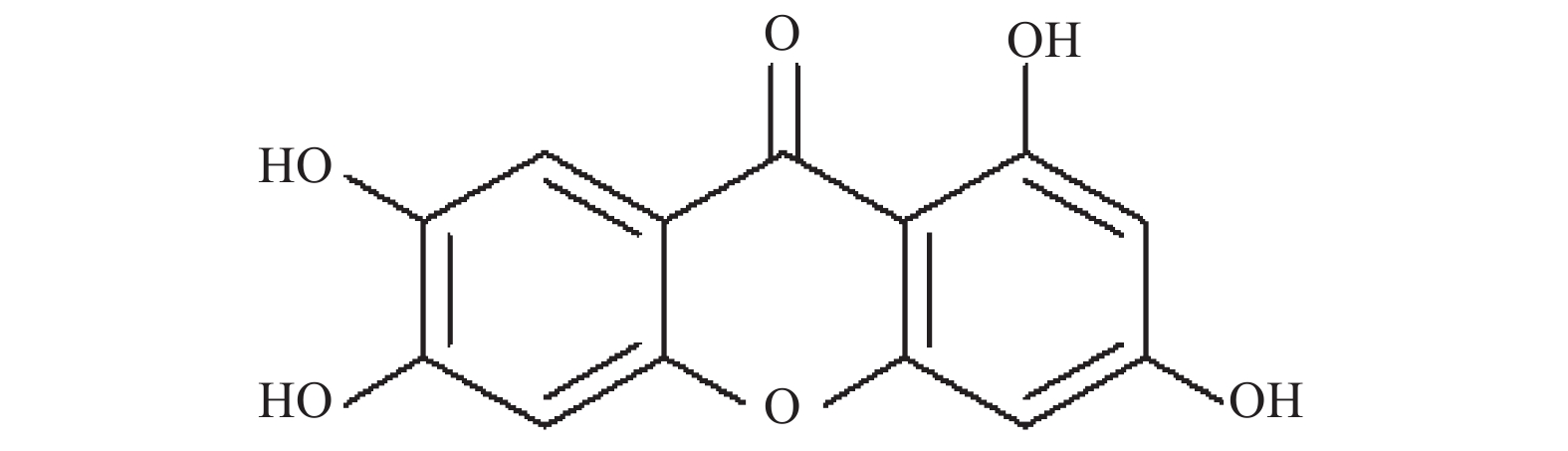
Effect of Norathyriol on Uric Acid Excretion Indicators in Hyperuricemic Nephropathy Rats
-
摘要:
目的 研究芒果苷元对尿酸性肾病大鼠尿酸排泄指标的影响。 方法 用腺嘌呤加氧嗪酸钾诱导成尿酸性肾病大鼠模型,在此模型上共给药28 d,测定24 h尿量、尿尿酸、尿肌酐、血尿酸、血肌酐及体重,并计算心肝脾肾指数及尿酸排泄指标:尿酸排泄分数(FEUA)、24 h尿酸排泄量(24 h UUA)、肌酐清除率(Ccr)、尿酸清除率(Cur)、肾小球尿酸负荷率(FLur)、单位肾小球滤过尿酸排泄(EurGF)、尿尿酸/尿肌酐(UUA/Ucr)。 结果 芒果苷元各剂量组均能显著降低尿酸性肾病大鼠血尿酸水平(P < 0.05),2.0 mg/kg芒果苷元组给药7 d后24 h UUA(P < 0.05)、给药14 d后 Uv(P < 0.05,P < 0.01)以及给药28 d后FEUA和Cur显著增加(P < 0.05)。 结论 芒果苷元能影响尿酸性肾病大鼠肾脏排泄尿酸的敏感指标FEUA和Cur。 Abstract:Objective To study the effect of norathyriol on uric acid excretion indicators in hyperuricemic nephropathy (HN) rats induced by adenine and potassium oxazinate. Method Sixty male SD rats were randomly divided into normal group, model group, norathyriol 1.0, 2.0, 4.0 mg/kg group, positive control benzbromarone 12.5 mg/kg group, each group of 10, according to 20 mL/kg volume were given respectively adenine (0.1 g/kg) and potassium oxonate (1.5 g/kg) suspension after 1 hour, and according to 10 ml/kg volume were given the test drug was administered once a day for 28 days. The gain weight of the rats was monitored weekly, and the urine was collected for 24 hours in themetabolic cage at 7, 14, 21 and 28 days after the administration. The urine volume, urine uric acid and urine creatinine were measured. At the end of the experiment, blood uric acid, serum creatinine and organ weight were measured. Uric acid excretion indicators were calculated: The fractional excretion of uric acid (FEUA), the amount of 24 h uric acid excretion (24 h UUA), creatinine clearance (CCr), uric acid clearance (Cur), glomerular load of uric acid (FLur), excretion of uric acid per volume of glomerular filtration (EurGF) and ratio of urinary uric acid to creatinine. Results Norathyriol groups significantly reduced the level of serum uric acid in rats with hyperuricemic nephropathy. After 7 days of administration of 2.0 mg/kg norathyriol, 24 h UUA significantly increased (P < 0.05). After 14 days and 28 days of administration of 2.0 mg/kg norathyriol, FEUA and Cur significantly increased (P < 0.05, P < 0.01). Conclusion Norathyriol could affect FEUA and Cur, the sensitive indicators of uric acid excretion of rats with hyperuricemic nephropathy. -
表 1 芒果苷元对尿酸性肾病大鼠24 h 尿量的影响[(
$ \bar x \pm s$ ),n = 10]Table 1. Effect of norathyriol on 24 h urine volume (UV) in hyperuricemic nephropathy rats [(
$ \bar x \pm s$ ),n = 10]组别 剂量
(mg/kg)24 h尿量(mL) 7 d 14 d 21 d 28 d 正常 0.5%CMC-Na 16.40 ± 4.68 15.31 ± 4.07 23.33 ± 11.09 13.12 ± 4.64 模型 0.5%CMC-Na 17.35 ± 5.41 22.80 ± 5.88## 33.35 ± 7.20# 32.00 ± 7.91## 芒果苷元 1.0 22.60 ± 6.02 28.88 ± 4.97##* 34.98 ± 8.21# 28.27 ± 7.02## 2.0 21.30 ± 7.02 27.23 ± 7.92## 35.80 ± 7.80## 29.33 ± 9.62## 4.0 18.73 ± 5.16 26.25 ± 7.92## 30.13 ± 7.70 28.75 ± 8.76## 苯溴马隆 12.5 19.33 ± 4.62* 27.28 ± 7.52## 35.15 ± 9.59# 34.23 ± 8.84## 与模型组比较,*P < 0.05;与正常组比较,#P < 0.05,##P < 0.01。 表 2 芒果苷元对尿酸性肾病大鼠尿尿酸水平的影响[(
$ \bar x \pm s$ ),n = 10]Table 2. Effect of norathyriol on the level of urine uric acid (UUA) in hyperuricemic nephropathy rats [(
$ \bar x \pm s$ ),n = 10]组别 剂量
(mg/kg)尿酸水平(mmol/L) 7 14 21 28 d 正常 0.5%CMC-Na 0.79 ± 0.16 0.87 ± 0.26 0.45 ± 0.19 0.99 ± 0.28 模型 0.5%CMC-Na 1.45 ± 0.39## 1.14 ± 0.35 0.68 ± 0.17# 1.74 ± 0.91# 芒果苷元 1.0 1.16 ± 0.23## 1.13 ± 0.35 0.64 ± 0.26 1.36 ± 0.41# 2.0 1.66 ± 0.98# 1.11 ± 0.37 0.69 ± 0.27# 1.88 ± 1.19# 4.0 2.02 ± 1.53# 1.27 ± 0. 60 0.59 ± 0.24 1.47 ± 0.35## 苯溴马隆 12.5 1.37 ± 0.54## 1.34 ± 0.52# 0.58 ± 0.13 1.59 ± 0.86 与模型组比较,*P < 0.05;与正常组比较,#P < 0.05,##P < 0.01。 表 3 芒果苷元对尿酸性肾病大鼠24 h 尿酸排泄量的影响[(
$ \bar x \pm s$ ),n = 10]Table 3. Effect of norathyriol on 24 h uric acid excretion (24UUA) in hyperuricemic nephropathy rats [(
$ \bar x \pm s$ ),n = 10]组别 剂量
(mg/kg)24 h 尿酸排泄量(mmol) 7 14 21 28 正常 0.5%CMC-Na 12.99 ± 2.44 14.41 ± 3.59 8.81 ± 1.66 12.61 ± 4.33 模型 0.5%CMC-Na 24.67 ± 9.28## 31.68 ± 21.32# 29.52 ± 21.55# 58.25 ± 37.37## 芒果苷元 1.0 26.19 ± 7.87## 32.74 ± 11.85## 24.00 ± 15.78# 39.81 ± 19.60## 2.0 35.47 ± 6.96##* 36.10 ± 24.98# 26.06 ± 16.23## 57.48 ± 35.51## 4.0 37.54 ± 29.81# 39.73 ± 25.26## 18.53 ± 11.46# 43.64 ± 21.14## 苯溴马隆 12.5 26.32 ± 9.30## 37.15 ± 19.09# 20.26 ± 7.38## 57.09 ± 34.97## 与模型组比较,*P < 0.05;与正常组比较,#P < 0.05,##P < 0.01。 表 4 芒果苷元对尿酸性肾病大鼠尿肌酐的影响[(
$ \bar x \pm s$ ),n = 10]Table 4. Effect of norathyriol on urine creatinine (UCr) in hyperuricemic nephropathy rats [(
$ \bar x \pm s$ ),n = 10]组别 剂量
(mg/kg)尿肌酐(mmol/L) 7 14 21 28 d 正常 0.5%CMC-Na 3.74 ± 0.49 4.52 ± 2.00 3.55 ± 2.32 4.70 ± 1.31 模型 0.5%CMC-Na 4.32 ± 1.29 4.07 ± 1.46 3.04 ± 0.65 2.97 ± 0.83## 芒果苷元 1.0 3.47 ± 0.85 3.29 ± 0.66 2.42 ± 0.66 2.83 ± 0.51## 2.0 3.61 ± 0.86 3.83 ± 1.11 2.97 ± 0.71 2.73 ± 0.51## 4.0 3.78 ± 0.72 3.69 ± 0.76 2.67 ± 1.11 3.08 ± 0.66## 苯溴马隆 12.5 3.38 ± 0.51* 3.71 ± 0.47 2.59 ± 0.76 2.96 ± 0.36## 与模型组比较,*P < 0.05;与正常组比较,#P < 0.05,##P < 0.01。 表 5 芒果苷元对尿酸性肾病大鼠血尿酸和血肌酐水平的影响[(
$\bar x \pm s$ ),n = 10]Table 5. Effect of norathyriol on serum uric acid (SUA) and serum creatinine (Scr) in hyperuricemic nephropathy rats [(
$ \bar x \pm s$ ),n = 10]组别 剂量(mg/kg) 血尿酸(μmol/L) 血肌酐(μmol/L) 正常 0.5%CMC-Na 93.30 ± 25.50 66.13 ± 11.01 模型 0.5%CMC-Na 312.77 ± 60.85## 104.38 ± 27.92## 芒果苷元 1.0 249.37 ± 65.50##* 94.90 ± 17.01## 2.0 196.81 ± 112.08#* 86.74 ± 23.73# 4.0 257.32 ± 25.99##* 92.21 ± 24.74## 苯溴马隆 12.5 255.41 ± 59.37## 103.52 ± 12.84## 与模型组比较,*P < 0.05;与正常组比较,#P < 0.05,##P < 0.01。 表 6 芒果苷元对尿酸性肾病大鼠FEUA、CUr、CCr、FLur、EurGF、UUA/UCr的影响[(
$\bar x \pm s$ ),n = 10]Table 6. Effect of norathyriol on FEUA、CUr、CCr、FLur、EurGF、UUA/UCr in hyperuricemic nephropathy rats [(
$ \bar x \pm s$ ),n = 10]组别 剂量
(mg/kg)尿酸分级排泄
指数FEUA(%)尿酸清除率
CUr(ml/min)肌酐清除率
CCr (ml/min)肾小球尿酸负荷率
FLur(μmol/min)单位肾小球滤过尿酸
排泄EurGF(μmol/L)尿尿酸/尿肌酐
UUA/UCr正常 0.5%CMC-Na 16.11 ± 6.83 0.10 ± 0.06 0.68 ± 0.27 0.059 ± 0.026 13.83 ± 4.86 0.20 ± 0.05 模型 0.5%CMC-Na 16.38 ± 5.34 0.13 ± 0.10 0.79 ± 0.33 0.23 ± 0.12## 50.17 ± 14.67## 0.53 ± 0.20## 芒果苷元 1.0 19.41 ± 6.88 0.11 ± 0.04 0.61 ± 0.23 0.16 ± 0.08## 46.66 ± 16.56## 0.49 ± 0.16## 2.0 49.57 ± 31.51#* 0.41 ± 0.25#* 0.79 ± 0.18 0.16 ± 0.12# 52.46 ± 18.17## 0.62 ± 0.30## 4.0 17.71 ± 6.71 0.12 ± 0.06 0.72 ± 0.33 0.18 ± 0.08## 46.01 ± 18.42## 0.50 ± 0.16## 苯溴马隆 12.5 21.98 ± 10.30 0.14 ± 0.06 0.68 ± 0.21 0.08 ± 0.15## 45.89 ± 13.01## 0.44 ± 0.11## 与模型组比较,*P < 0.05;与正常组比较,#P < 0.05,##P < 0.01。 表 7 芒果苷元对尿酸性肾病大鼠脏器指数的影响[(
$\bar x \pm s$ ),n = 10]Table 7. Effect of norathyriol on organ index in hyperuricemic nephropathy rats [(
$ \bar x \pm s$ ),n = 10]组别 剂量
(mg/kg)脏器指数(mg/g) 肾脏指数 肝脏指数 心脏指数 脾脏指数 正常 0.5%CMC-Na 6.87 ± 0.35 37.07 ± 5.21 3.34 ± 0.34 2.53 ± 0.42 模型 0.5%CMC-Na 10.96 ± 1.93## 37.58 ± 3.57 3.33 ± 0.18 2.52 ± 0.60 芒果苷元 1.0 11.66 ± 2.26## 37.55 ± 3.30 3.20 ± 0.57 2.75 ± 0.49 2.0 11.02 ± 2.03## 36.17 ± 4.85 3.38 ± 0.40 2.75 ± 0.88 4.0 10.97 ± 1.84## 35.26 ± 4.13 3.18 ± 0.26 3.01 ± 0.44# 苯溴马隆 12.5 11.13 ± 1.61## 37.78 ± 2.72 3.29 ± 0.40 2.96 ± 0.41# 与模型组比较,*P < 0.05;与正常组比较,#P < 0.05,##P < 0.01。 -
[1] Conen D,Wietlisbach V,Bovet P,et al. Prevalence of hyperuricemia and relation of serum uric acid with cardiovascular risk factors in a developing country[J]. Bmc Public Health,2004,4(9):1-9. [2] Qiu L,Cheng X Q,Wu J,et al. Prevalence of hyperuricemia and its related risk factors in healthy adults from Northern and Northeastern Chinese provinces[J]. Bmc Public Health,2013,13(1):664. doi: 10.1186/1471-2458-13-664 [3] Pascart T,Lioté F. Gout:state of the art after a decade of developments[J]. Rheumatology,2019,58(1):27-44. [4] Filiopoulos V,Hadjiyannakos D,Vlassopouls D. New insights into uric acid effects on the progression and prognosis of chronic kidney disease[J]. Ren Fail,2012,34(4):510-520. doi: 10.3109/0886022X.2011.653753 [5] Badve S V,Brown F,Hawley C M,et al. Challenges of conducting a trial of uric-acid-lowering therapy in CKD[J]. Nat Rev Nephrol,2011,7(5):295-300. doi: 10.1038/nrneph.2010.186 [6] Gustafsson D,Unwin R. The pathophysiology of hyperuricaemia and its possiblerelationship to cardiovascular disease,morbidity and mortality[J]. BMC Nephrol,2013,14(164):1-9. [7] Kang D H,Chen W. Uric acid and chronic kidney disease:new understanding of an old problem[J]. Semin Nephrol,2011,31(5):447-452. doi: 10.1016/j.semnephrol.2011.08.009 [8] 胡文姬,李学坚,刘布鸣,等. 芒果苷苷元研究进展[J]. 时珍国医国药,2013,24(11):2759-2763. [9] Niu Y F,Liu J,Liu H Y,et al. Hypouricaemic action of mangiferin results from metabolite norathyriol via inhibiting xanthine oxidase activity[J]. Pharm Biol,2016,54(9):1680-1686. doi: 10.3109/13880209.2015.1120322 [10] Lin H,Tu C,Niu Y F,et al. Dual actions of norathyriol as a new candidate hypouricaemic agent:uricosuric effects and xanthine oxidase inhibition[J]. Eur J of Pharmacol,2019,853:371-380. doi: 10.1016/j.ejphar.2019.04.034 [11] Perez-Ruiz F,Calabozo M. García Erauskin G,et al. García Erauskin G,et al. Renal underexcretion of uric acid is present in patients with apparent high urinary uric acid output[J]. Arthritis Rhum,2002,47(6):610-613. doi: 10.1002/art.10792 [12] Ali B H,Al Z M,Adham S A,et al. Therapeutic effect of chrysin on adenine-induced chronic kidney disease in rats[J]. Cell Physiol Biochem,2016,38(1):248-257. doi: 10.1159/000438626 [13] Liu N,Wang L,Yang T,et al. EGF receptor inhibition alleviates hyperuricemic nephropathy[J]. J Am Soc Nephrol,2015,26(11):2716-2729. doi: 10.1681/ASN.2014080793 [14] 张云静,邹作君,于龙丽,等. 早期肾功能损害患者肾脏排泄尿酸各指标的比较与分析[J]. 中国中西医结合肾病杂志,2012,13(1):54-56. doi: 10.3969/j.issn.1009-587X.2012.01.017 [15] Wang C P,Wang X,Zhang X,et al. Morin improves urate excretion and kidney function through regulation of renal organic ion transporters in hyperuricemic mice[J]. J Pharm Pharm Sci,2010,13(3):411-427. doi: 10.18433/J3Q30H [16] Wortmann R L,Fox I H. Limited value of uric acid to creatinine ratios in estimating uric acid excretion[J]. Ann Intern Med,1980,93(6):822-825. doi: 10.7326/0003-4819-93-6-822 -






 下载:
下载: