The Correlation between the Imaging Characteristics of Imported COVID-19 at First Diagnosis and Clinical Severity Grading
-
摘要:
目的 探讨输入性新型冠状病毒感染(COVID-19)首诊影像学特点与临床严重度分级的相关性。 方法 回顾性分析2020年1月21日至2020年2月25日云南省经核酸检测确诊116例输入性COVID-19病例(年龄范围为5~84岁,男59例,女57例)的临床及影像资料。比较不同临床分型(轻型、普通型、重型、危重型)患者的临床资料、实验室检查、影像学特征的差异。 结果 116例输入型患者中,不同年龄组间患病差异有统计学意义(χ2 = 19.589,P = 0.006),21~55岁患病率较高,占44.83%(55/116),51~70岁者患重症肺炎(6/42,14.29%)较21~50岁3/52(5.17%)高(P < 0.05);发热/畏寒(70.8%)及呼吸道症状(58.4%)是新冠肺炎最常见首诊症状。本组病例从症状出现至第1次CT扫描时间平均为(4.17±1.12)d,时间越长,临床分型越重( F = 2.688,P = 0.049);不同临床分型白细胞总数、淋巴细胞总数、淋巴细胞百分比、乳酸脱氢酶(LDH)、C反应蛋白差异有统计学意义(F = 3.486,3.640,5.154,15.361,8.195,P均 < 0.05);重型、危重型淋巴细胞总数及淋巴细胞百分比较轻型与普通型明显降低( P < 0.05)。116例共383个病灶,总累及范围平均评分为(4.17±2.12)分,普通型较危重型累及范围小( F = 62.137,P = 0.000);病灶多累及双侧肺,约占70/116(78.26%),下叶85/116(37.12%)较中叶70/116(30.13%)、上叶75/116(32.75%)多见(χ2 = 10.190,P = 0.021),胸膜下区87/229(57.24%)较肺门区29/229(19.08%)、肺中带36/229(23.68%)多见(χ2 = 5.187,P = 0.018);圆形、椭圆形病灶多见(χ2 = 43.922,P = 0.000),其中带状及盘状病变以重型、危重型患者多见(P < 0.05);不同类型患者病变特点不同( χ2 = 50.974,P = 0.000),其中GGO内血管增粗发生率最高,约占19.58%。单纯GGO、PS、混合密度影、支气管充气征及晕征普通型较重型多见(P < 0.05),GGO伴支气管壁增厚、纤维索条、支气管变形以重型、危重型多见( P < 0.05);伴随病变中以胸膜增厚为最多见( χ2 = 42.119,P = 0.000)。 结论 不同临床分型的输入性COVID-19,临床资料、实验室检查及影像表现具有一定的特征性,在核酸检测试剂盒不足的情况下,HRCT对COVID-19的早期筛查、诊断、临床分型提供立论依据。 -
关键词:
- 输入性新型冠状病毒感染 /
- 影像表现 /
- 临床分级
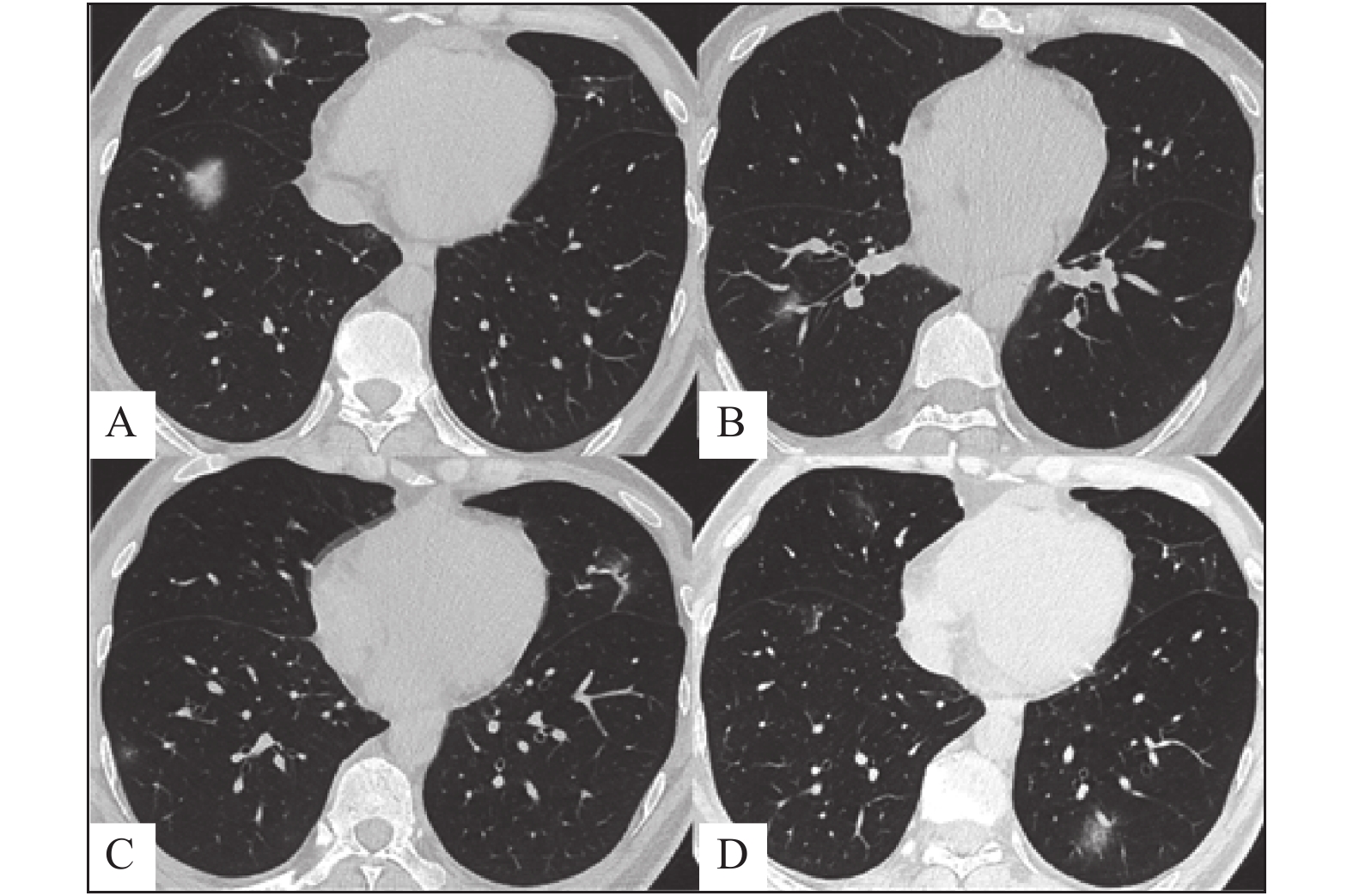
Abstract:Objective To investigate the correlation between the imaging characteristics of the first diagnosis of imported novel coronavirus pneumonia (COVID-19) and clinical severity grading. Methods A retrospective analysis was performed on the clinical and imaging data of 116 imported COVID - 19 cases (aged 5 ~ 84 years, 59 males and 57 females) confirmed by nucleic acid test on January 21, 2020 (solstice, February 25, 2020) in Yunnan province.Differences in clinical data, laboratory examination and imaging characteristics of patients with different clinical types (light, normal, heavy and critical) were compared. Fisher’ s exact probability method was used for comparison of measurement data, z-test was used for comparison of ppairs, analysis of variance was used for comparison of quantitative data, and mann-whitney test was used for comparison of ppairs. Results There was no statistically significant difference in prevalence between male and female patients with 116 cases input COVID-19 (χ2 = 1.288, P = 0.808); There were statistically significant differences among different age groups (χ2 = 19.589, P = 0.006), The prevalence of 21-55 years old is high, about 44.83% (55/116), the second is 51 to 70 years old, about 36.21% (42/116), Severe pneumonia (6/42, 14.29%) was higher in patients aged from 51 to 70 than in patients aged 21 to 50 (3/52(5.17%) (P < 0.05).; Fever/chills (70.8%) and respiratory symptoms (58.4%) were the most common initial symptoms of new crown pneumonia.The average time from symptom onset to the first CT scan was 4.17±1.12 days. The longer the time, the heavier the clinical classification ( F = 2.688, P = 0.049). The differences in total number of leukocytes, total number of lymphocytes, percentage of lymphocytes, lactate dehydrogenase (LDH) and c-reactive protein in different clinical classifications were statistically significant (F = 3.486, 3.640, 5.154, 15.361, 8.195, all P < 0.05). The total number and percentage of lymphocytes of the severe and critical types were significantly lower than that of the light and normal types ( P < 0.05). There were 383 lesions in 116 patients, with an average score of 4.17±2.12 points in total involvement range, and the involvement range of the normal type was smaller than that of the critical type ( F = 62.137, P = 0.000). The lesions mostly involve both lungs, accounting for approximately70/116 (78.26%), The lower lobe 85/116 (37.12%) is more common than the middle lobe 70/116 (30.13%) and the upper lobe 75/116 (32.75%) (χ2 = 10.190, P = 0.021) The subpleural area87/229 (57.24%) is more common than the hilum area 29/229 (19.08%) and the middle lung zone36/229 (23.68%) (χ2 = 5.187, P = 0.018); Round and oval lesions were more common (χ2 = 43.922, P = 0.000), and banded and discoid lesions were more common in severe and critical patients (P < 0.05). Different types of patients have different pathological characteristics ( χ2 = 50.974, P = 0.000), vascular enlargement sign is the highest incidence in GGO, approximately 19.58%, next is cable strip shadow, approximately 13.71% and paving pattern, about13.61%. pure GGO, paving pattern, mixed density, air bronchogram and halo sign are more common in ordinary type (P < 0.05), GGO accompanied by thickening of bronchial wall, fiber cord, and deformation of bronchi were mostly seen in heavy and critical cases ( P < 0.05); Pleural thickening was the most common extrapulmonary lesion ( χ2 = 42.119, P = 0.000), about 73.12%, Heavy pleural effusion is more common than normal type and critical type (P < 0.05). Conclusion The clinical data, laboratory examination and imaging findings of input COVID-19 with different clinical typing have certain characteristics. HRCT can provide theoretical basis for early screening, diagnosis and clinical typing of COVID-19 with insufficient nucleic acid detection kits. -
表 1 云南省输入性COVID-19首诊病例不同临床分型临床特征比较(n = 116例)( $\bar x \pm s $)
Table 1. Comparison of clinical characteristics of imported COVID-19 cases with different clinical types in Yunnan Province (n = 116 cases)( $\bar x \pm s $)
临床特征 [n(%)] COVID-19临床分型(n) χ2 P 轻型 普通型 重型 危重型 性别 24 80 10 2 1.288 0.808 男 59(50.86) 14 40 4 1 女 57(49.14) 10 40 6 1 年龄(岁) 19.589 0.006* 小于20 16(13.79) 7 9 0 0 21~50 52(44.83) 14 35 3 0 51~70 42(36.21) 3 32 6 1 大于70 6(5.17) 0 4 1 1 首诊临床症状 17.425 0.488 干咳/咽痛 52(58.4) 9 37 5 1 发热/畏寒 63(70.8) 10 43 8 2 全身酸痛/无力 26(29.2) 3 19 4 0 消化道症状 1(1.1) 0 0 0 1 头痛 5(5.6) 1 3 1 0 头晕/恶心 9(10.1) 2 6 1 0 呼吸困难/胸闷 11(12.4) 2 5 3 1 基础疾病 29.32 0.001* 无 89(72.36) − 糖尿病 9(7.14) 0 1 8 0 高血压 6(4.76) 0 1 4 1 心脏病 5(3.97) 0 3 0 2 脑血管疾病 4(3.17) 1 1 1 1 肺部疾病 4(3.17) 0 4 0 0 其他 9(7.14) 0 7 2 0 症状出现至首次
CT时间(d)4.17 ± 1.12 2.1 ± 1.7 3.05 ± 1.2 5.1 ± 3.5 9 ± 1.4 F = 2.688 0.049* *P < 0.05。 表 2 云南省输入性COVID-19首诊病例不同临床分型实验室指标比较(n = 116例)( $\bar x \pm s$)
Table 2. Comparison of laboratory indicators for different clinical types of imported COVID-19 cases in Yunnan Province (n = 116 cases) ( $\bar x \pm s$)
实验室指标 COVID-19临床分型 F P 轻型(n = 24) 普通型(n = 80) 重型(n = 10) 危重型(n = 2) 白细胞总数(109/L) 5.86 ± 1.76 5.16 ± 1.52 7.43 ± 5.61△ 4.8 ± 1.68 3.486 0.018* 淋巴细胞总数(109/L) 1.38 ± 0.66 1.35 ± 0.57 0.85 ± 0.47 0.47 ± 0.07 3.640 0.015* 淋巴细胞百分比(%) 28 ± 14 28 ± 1.9 16 ± 0.9 9 ± 3.01 5.154 0.002* AST(U/L) 22.66 ± 3.16 28.51 ± 4.28 36.46 ± 6.91 47.5 ± 6.92 2.537 0.060 ALT(U/L) 30.91 ± 3.56 26.91 ± 5.44 36.08 ± 8.05 31.05 ± 4.31 0.449 0.719 肌酶(U/L) 62.83 ± 2.66 64.02 ± 81.82 123.52 ± 74.16 422.05 ± 21.14 17.576 0.100 肌红蛋白(ng/mL) 31.13 ± 27.77 19.12 ± 19.89 35.95 ± 14.87 134.36 ± 137.69 15.361 0.060 乳酸脱氢酶(U/L) 213.91 ± 28.72 137.48 ± 2.53 257.52 ± 5.65 315.00 ± 10.21 8.195 < 0.001* 肌钙蛋白(ng/mL) 0.02 ± 0.001 0.35 ± 0.01 2.00 ± 0.007 0.02 ± 0.01 1.307 0.276 反应蛋白(mg/L) 12.10 ± 6.58 11.66 ± 7.26 52.16 ± 4.38 71.95 ± 5.75 12.326 < 0.001* 血沉(mm/h) 20.70 ± 5.13 28.3 ± 2.81 43.9 ± 6.95 83 ± 16.97 6.834 0.068 D2聚体(ug/ml) 0.47 ± 0.29 0.44 ± 0.27 0.60 ± 0.37 2.81 ± 2.32 30.256 0.073 *P < 0.05。 表 3 云南省输入性COVID-19首诊病例不同临床分型影像表现比较(n = 116例)( $\bar x \pm s $)
Table 3. Comparison of imaging manifestations of imported COVID-19 cases with different clinical types in Yunnan Province (n = 116 cases)( $\bar x \pm s $)
项目 [n(%)] COVID-19临床分型 χ2/F P 普通型(n = 80) 重型(n = 10) 危重型(n = 2) 累及侧别 6.210 0.128 左肺 8(7.61) 5 2 0 右肺 14(14.13) 10 3 0 双肺 70(78.26) 65 5 2 累及部位 10.190 0.021* 上叶 75(32.61) 57 16 2 中叶
(包括左肺上叶舌段)70(30.43) 65 4 1 下叶 85(36.96) 65 18 2 累及位置 8.904 0.045* 胸膜下 100(60.61) 80 18 2 肺中带 40(24.24) 26 11 3 肺门区 25(15.15) 14 9 2 病变形状 43.922 0.000* 楔形 109(28.45) 78 29 2 圆形、椭圆 178(46.47) 156 22 0 带状 42(10.96) 29 11 2 盘状 54(14.09) 26 22 6 病变特点 50.974 0.000* GGO 139(7.22) 101 34 4 铺路石征(PP) 262(13.61) 179 75 8 GGO + 实变 242(12.57) 170 68 4 GGO + 增粗血管(VES) 377(19.58) 278 91 8 GGO + 支气管壁增厚 114(5.92) 76 30 8 GGO + 充气支气管征 211(10.96) 144 59 8 GGO伴纤维索条 264(13.71) 159 97 8 GGO支气管变形 199(10.34) 128 63 8 晕征(HS) 68(3.53) 63 5 0 反晕征(RHS) 18(0.94) 16 2 0 实变 31(1.61) 26 4 1 伴随肺外改变 42.119 0.000* 胸膜增厚 291(73.12) 189 75 8 胸膜下透亮影 77(20.43) 35 33 8 胸腔积液 16(4.30) 6 8 2 淋巴结增大 4(2.15) 0 4 4 累及范围评分
(共18分)4.74 ± 2.12 4.01 ± 1.43 5.91 ± 3.23 9.33 ± 3.50 62.137 0.000* *P < 0.05。 -
[1] Mahase E. Coronavirus:covid-19 has killed more people than SARS and MERS combined,despite lower case fatality rate[J]. BMJ,2020,368:m641. [2] 邓芷晴,张笑春,李一荣,等. 胸部CT筛查在新型冠状病毒感染暴发早期的价值[J]. 中华放射学杂志,2020,54(5):430-434. [3] Franquet,Tomás. Imaging of pulmonary viral pneumonia.[J]. International Journal of Medical Radiology,2011,260(1):18-39. [4] 国家卫生健康委员会办公厅, 国家中医药管理局办公室. 新型冠状病毒感染的肺炎诊疗方案(试行第七版)[EB/OL]. (2020-03-03)[2020-04-03]. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml. [5] 中华医学会放射学分会. 新型冠状病毒感染的放射学诊断: 中华医学会放射学分会专家推荐意见(第一版)[J/OL]. (2020-02-08)[2020-04-03]中华放射学杂志, 2020, 54. http://rs.yiigle.com/yufabiao/1180115.htm. [6] 范丽,萧毅,王晨光,等. 影像科面对新型冠状病毒感染科室工作模式的转变[J]. 中华放射学杂志,2020,54(5):495-497. doi: 10.3760/cma.j.cn112149-20200207-00106 [7] Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China[J]. Lancet,2020,395(10223):497-506. [8] 黄璐,韩瑞,于朋鑫,等. 新型冠状病毒感染不同临床分型间CT和临床表现的相关性研究[J]. 中华放射学杂志,2020,54(4):300-304. doi: 10.3760/cma.j.cn112149-20200205-00087 [9] Shi H,Han X,Jiang N,et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan,China:a descriptive study[J]. The Lancet Infectious Diseases,2020,20(4):425-434. doi: 10.1016/S1473-3099(20)30086-4 [10] Xu Z,Shi L,Y Wang,et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome[J]. The Lancet Respiratory Medicine,2020,8(4):420-422. doi: 10.1016/S2213-2600(20)30076-X [11] Tian A S,Wh B,Niu A L,et al. Pulmonary pathology of early-phase 2019 novel coronavirus(COVID-19)pneumonia in two patients with lung cancer[J]. Journal of Thoracic Oncology,2020,15(5):700-704. doi: 10.1016/j.jtho.2020.02.010 [12] 胡瑞,黄楠,陈文,等. 新型冠状病毒感染确诊与疑似患者的临床和胸部CT影像比较[J]. 中华放射学杂志,2020,54(5):440-444. doi: 10.3760/cma.j.cn112149-20200220-00205 [13] Snydman D R. The diagnostic value of halo and reversed halo signs for invasive mold infections in compromised hosts.[J]. Clinical Infectious Diseases,2011,52(9):1144-1155. doi: 10.1093/cid/cir122 -






 下载:
下载: