The Relationship between Vitamin D Receptor Gene Polymorphism and Type 2 Diabetes Mellitus with Osteoporosis in Kunming Area
-
摘要:
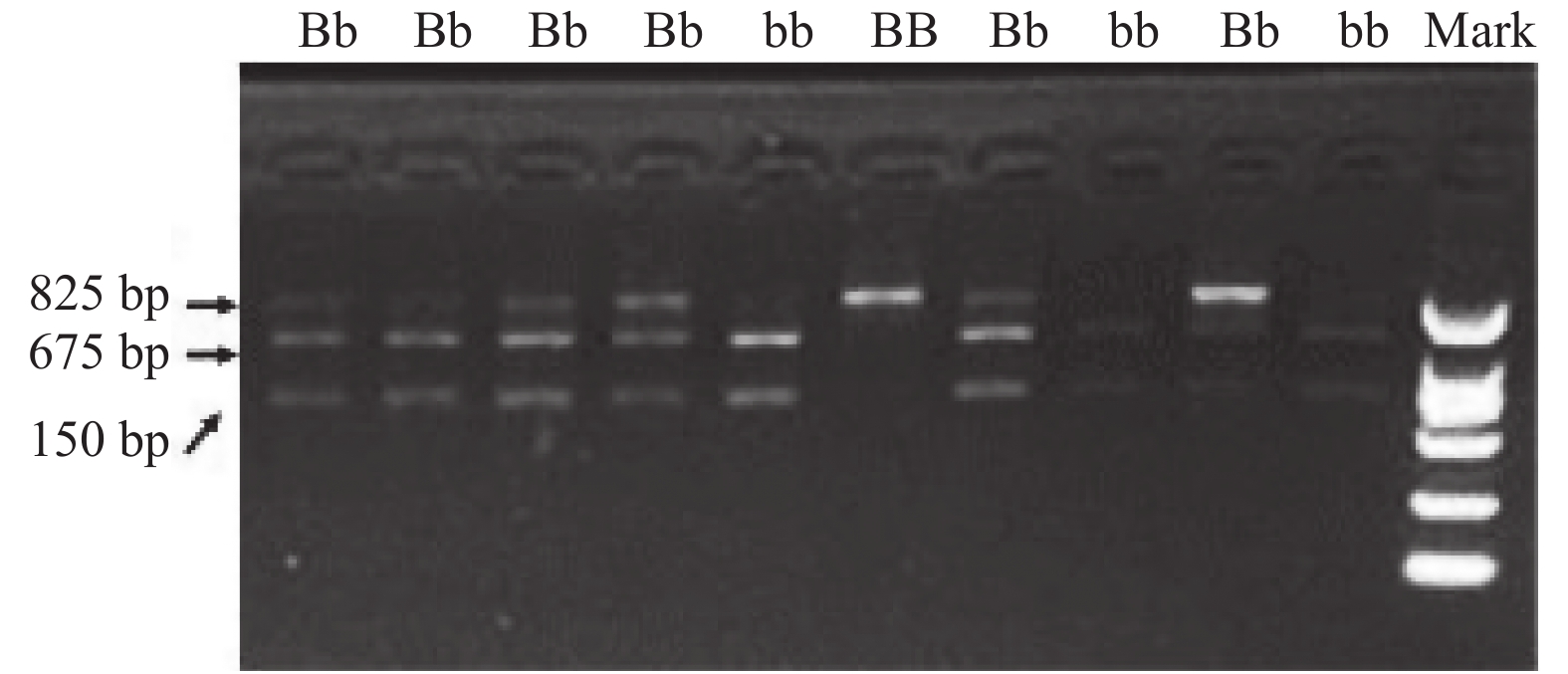
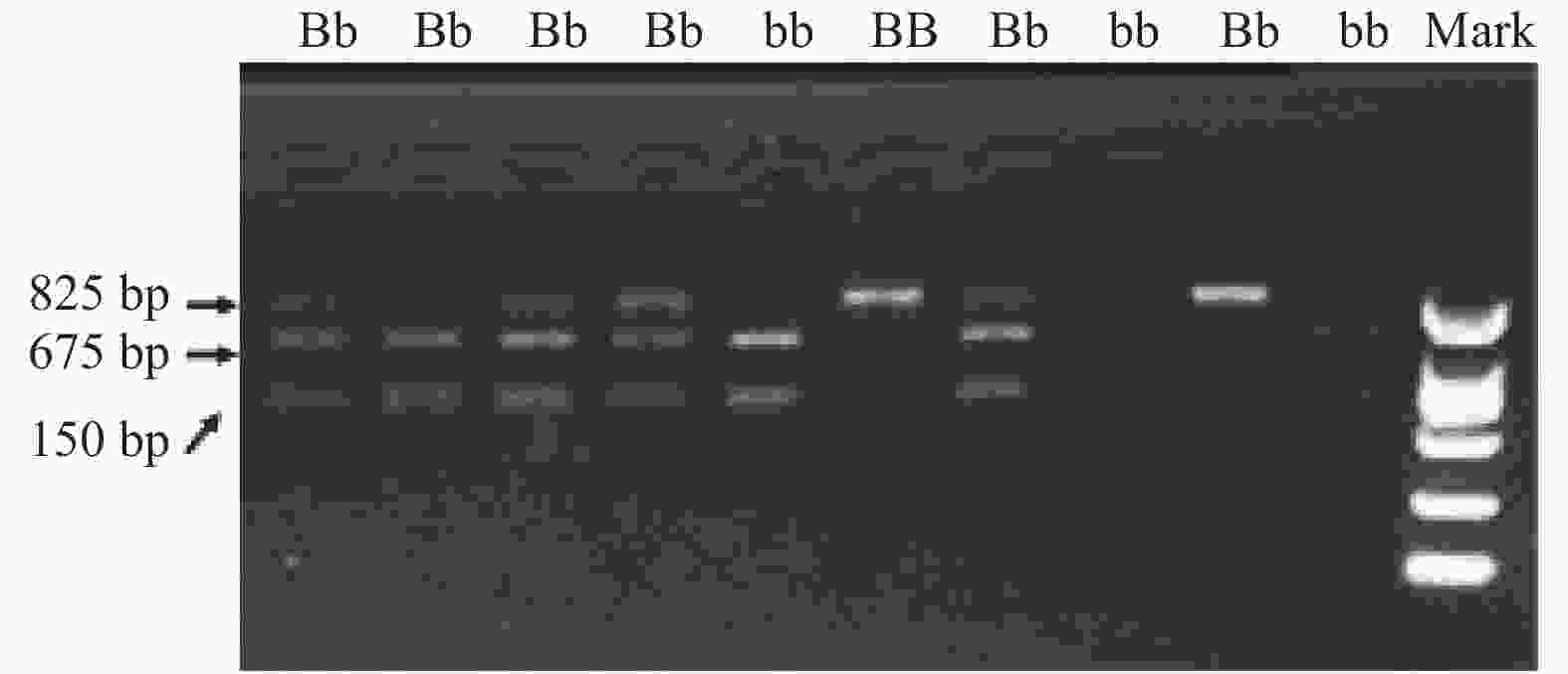
目的 研究维生素D受体(VDR)基因多态性与昆明地区2型糖尿病(T2DM)伴骨质疏松症的关系,探讨T2DM伴骨质疏松症发病的遗传易感因素。 方法 收集2017年6月至2019年1月在昆明市第一人民医院内分泌科住院的T2DM患者237例,(1)按骨密度结果分组为T2DM无骨质疏松组(61例),T2DM合并骨量减少组(111例),T2DM伴骨质疏松组(65例),采用PCR-RFLP技术,检测VDR基因型,比较3组患者以下指标间的差异:VDR基因型及等位基因频率,性别、年龄、糖尿病病程、血压、身高、体重、体重指数(BMI)、空腹血糖(FPG)、糖化血红蛋白(HbA1c)、血钙、血脂、血尿酸(UA)、维生素D浓度、雌激素、睾酮水平,超敏C-反应蛋白(Hs-CRP)、纤维蛋白原(FIB),口服葡萄糖耐量(OGTT)-0 h、2 h血糖,0 h、2 h胰岛素(INS)水平,胰岛素抵抗指数(HOMA-IR);(2)比较VDR不同基因型间骨密度的差异;(3)将VDR基因型及组间差异有统计学意义的指标进行多因素Logistic回归分析。 结果 (1)昆明地区T2DM患者,VDR基因型以Bb型为主,占77.6%;(2)3组患者比较,VDR基因型频率及等位基因频率,差异无统计学意义(P > 0.05);(3)VDR 3种基因型比较,各部位的骨密度,差异无统计学意义(P > 0.05);(4)多因素Logistic回归分析显示:年龄,吸烟可进入回归方程,而VDR基因型未进入回归方程。 结论 (1)昆明地区T2DM患者,VDR基因型以Bb型为主;(2)年龄,吸烟是昆明地区 T2DM伴骨质疏松患者的独立危险因素,VDR(Bsm I)基因型与昆明地区 T2DM伴骨质疏松症的遗传易感性无关。 -
关键词:
- 维生素D受体基因多态性 /
- 2型糖尿病 /
- 骨质疏松症
Abstract:Objective To study the relationship between vitamin D receptor (VDR) gene polymorphism and type 2 diabetes mellitus (T2DM) with osteoporosis in Kunming area, and to explore the genetic susceptibility factors of T2DM with osteoporosis. Methods We selected 237 diabetic patients in the department of endocrinology of First People’ s hospital of Kunming from June 2017 to January 2019. (1) The patients were divided into T2DM without osteoporosis group (61 cases), T2DM with osteopenia group (111 cases), and T2DM with osteoporosis group (65 cases) by bone mineral density results. PCR - RFLP technique was used to detect VDR genotypes, we compared the differences between the three groups of patients in following indicators: VDR genotype and allele frequency, sex, age, duration of diabetes, blood pressure, height, weight, body mass index (BMI), fasting plasma glucose (FPG), glycosylated hemoglobin (HbA1c), blood calcium, blood lipids, blood uric acid (UA), the concentration of vitamin D, estrogen and testosterone levels, allergic C - reactive protein (Hs - CRP), fibrinogen (FIB), oral glucose tolerance (OGTT) -0 h, 2 h; 0 h, 2 h-insulin (INS) level and insulin resistance index (HOMA-IR). (2) The differences in the bone mineral density was compared between different genotypes. (3) The VDR genotypes and the indicators with statistical differences between groups were analyzed by multivariate logistic regression. Results (1) VDR genotype was given priority to with a Bb, accounting for 77.6% in patients with T2DM in kunming area. (2) VDR genotype frequency and allele frequency differences between the three groups had no statistical significance (P > 0.05). (3) There was no significant difference in BMD between the three genotypes of VDR (P > 0.05) (P > 0.05). (4) Multivariate logistic regression analysis showed that age and smoking could enter the regression equation, but VDR genotype did not. Conclusions (1) The main VDR genotype of T2DM patients in Kunming was Bb (2) Age and smoking were independent risk factors of T2DM patients with osteoporosis in Kunming. VDR (BSMI) genotype was not associated with the genetic susceptibility of T2DM patients with osteoporosis in Kunming. -
表 1 研究对象的一般资料比较[
$\bar x \pm s$ ,M(P25,P75)]Table 1. Comparison of general data of study subjects [
$\bar x \pm s$ ,M(P25,P75)]指标/分组 T2DM无骨质疏松组
(61例)T2DM合并骨量减少组
(111例)T2DM伴骨质疏松组
(65例)χ2/F/Z P 性别(男/女)) 46/15 61/50 # 15/50* # & 18.286 0.000 年龄(岁) 61.65 ± 8.16 64.79 ± 10.15# 66.33 ± 6.77* # & 4.573 0.011 吸烟(是/否) 24/37 32/79 11/54* # 7.833 0.020 饮酒(是/否) 17/44 29/82 6/59* # & 8.518 0.014 绝经年龄(女,岁) 50(48,54) 50(48,52) 50(48,51) −0.744 0.457 糖尿病病程(a) 9.18 ± 7.34 10.11 ± 7.46 8.69 ± 7.36 0.805 0.449 收缩压(mmHg) 126.77 ± 22.50 129.07 ± 19.73 125.77 ± 22.54 0.543 0.582 舒张压(mmHg) 80.77 ± 11.51 78.64 ± 10.27 74.97 ± 12.30*# 4.364 0.014 身高(m) 167.64 ± 7.32 164.12 ± 8.04 # 158.13 ± 7.21* #& 24.880 0.000 体重(kg) 71.02 ± 11.16 65.85 ± 9.94 # 59.07 ± 10.45* #& 20.955 0.000 体重指数(kg/m2) 25.26 ± 2.77 24.29 ± 2.75 # 23.40 ± 3.21* # 6.369 0.002 TC(mmol/L) 4.94 ± 1.59 4.57 ± 1.22 4.90 ± 1.02 2.122 0.122 TG(mmol/L) 2.13(1.32,3.25) 1.65(1.19,2.26) 1.79(1.30,2.41) −2.163 0.051 HDLC(mmol/L) 1.09 ± 0.34 1.15 ± 0.28 1.23 ± 0.31* # 3.410 0.035 LDLC(mmol/L) 2.79 ± 1.14 2.82 ± 0.99 3.15 ± 1.01 2.389 0.094 FPG(mmol/L) 8.63(7.31,12.29) 8.55(6.85,11.19) 8.13(6.58,10.97) −1.297 0.195 HBA1c(%) 8.60 ± 1.91 8.32 ± 2.04 8.06 ± 1.76 1.199 0.303 OGTT-0 h(mmol/L) 8.09 ± 2.29 8.25 ± 2.06 8.13 ± 2.71 0.093 0.911 OGTT-2 h(mmol/L) 17.86 ± 3.19 18.29 ± 4.60 17.81 ± 4.73 0.223 0.800 INS-0 h(mIU/L) 15.36(9.50,21.35) 15.64(7.83,32.75) 15.23(8.23,25.83) −0.426 0.670 INS-2 h(mIU/L) 34.79(23.12,58.31) 41.12(25.93,67.58) 52.49(35.09,81.46) −1.300 0.194 HOMR-IR 4.77(2.69,9.08) 5.23(2.65,11.2) 4.98(2.37,8.86) −0.492 0.623 UA(μmol/L) 354.05 ± 86.92 342.32 ± 99.48 314.82 ± 92.09 2.909 0.057 血钙(mmol/L) 2.33 ± 0.11 2.31 ± 0.12 2.32 ± 0.12 0.722 0.487 雌激素
(pmol/L)116.90(80.73,152.44,) 90.42(60.97,140.19) 81.12(58.63,98.22)* # −1.949 0.041 睾酮(nmol/L) 9.13(1.94,14.85) 5.17(1.32,12.09) 1.57(1.17,2.38)* #& −2.281 0.023 维生素D(ng/mL) 18.15 ± 9.72 16.78 ± 6.16 16.00 ± 5.71 1.403 0.248 Hs-CRP(mg/L) 1.72(0.61,3.02) 1.70(0.50,2.69) 1.06(0.50,3.16) −0.368 0.713 FIB(g/L) 2.89 ± 0.70 2.77 ± 0.64 2.80 ± 0.72 0.599 0.550 总体比较:*P < 0.05,两两比较:与无骨质疏松组比较,#P < 0.005,;与合并骨量减少组比较,&P < 0.05。 表 2 VDR基因型分布频率比较[n(%)]
Table 2. Comparison of VDR genotypes distribution frequency [n(%)]
组别/基因型 BB Bb bb 合计(n) T2DM无骨质疏松组 6(9.8) 46(75.4) 9(14.8) 61 T2DM合并骨量减少组 17(15.3) 89(80.2) 5(4.5) 111 T2DM伴骨质疏松组 8(12.3) 49(75.4) 8(12.3) 65 合计(n) 31 184 22 237 注:χ2 = 6.456,P = 0.168。 表 3 VDR等位基因分布频率比较
Table 3. VDR allele frequency distribution
组别/基因型 频数 B b T2DM无骨质疏松组 122 58 64 T2DM合并骨量减少组 222 123 99 T2DM伴骨质疏松组 130 65 65 注:χ2 = 1.953,P = 0.162。 表 4 VDR基因多态性与2型糖尿病患者BMD的关系[(g/cm2),(
$\bar x \pm s $ )]Table 4. The relationship between the VDR gene polymorphism and BMD of T2DM patients [(g/cm2),(
$\bar x \pm s $ )]指标/分组 BB组(31例) Bb组(184例) bb组(22例) F/Z P 腰1 0.944 ± 0.163 0.933 ± 0.162 0.964 ± 0.179 0.260 0.771 腰2 1.004 ± 0.1960 1.009 ± 0.195 1.040 ± 0.202 0.182 0.834 腰3 1.073 ± 0.184 1.048 ± 0.199 1.097 ± 0.217 0.493 0.612 腰4 1.112 ± 0.236 1.069 ± 0.197 1.138 ± 0.168 1.069 0.346 左股骨颈 0.870 ± 0.142 0.863 ± 0.198 0.874 ± 0.192 0.027 0.974 左大粗隆 0.723 ± 0.165 0.750 ± 0.159 0.773 ± 0.183 0.145 0.866 左全髋 0.961(0.817,1.033) 0.921(0.824,1.056) 0.979(0.727,1.081) 0.087 0.957 右股骨颈 0.842(0.734,0.965) 0.836(0.739,0.970) 0.877(0.589,1.052) 0.015 0.993 右大粗隆 0.747(0.586,0.824) 0.750(0.628,0.869) 0.795(0.528,0.911) 0.481 0.786 右全髋 0.893 ± 0.265 0.924 ± 0.15 0.915 ± 0.233 0.244 0.784 表 5 Logistic回归分析结果
Table 5. Logistic analysis results
因素 B P OR 95%CI VDR −0.648 0.253 0.523 0.172~1.587 性别 0.476 0.622 1.609 0.243~10.665 年龄 0.109 0.004 1.115 1.035~1.202 吸烟 2.334 0.013 10.318 1.637~65.046 饮酒 −1.034 0.226 0.356 0.067~1.895 DBP 0.006 0.795 1.006 0.962~1.051 身高 −0.106 0.181 0.900 0.770~1.051 体重 0.002 0.985 1.002 0.859~1.168 BMI −0.134 0.551 0.875 0.564~1.358 HDL-C 0.253 0.782 1.288 0.215~7.713 雌激素 0.000 0.915 1.000 0.994~1.007 睾酮 −0.131 0.061 0.877 0.765~1.006 -
[1] Gordon Gong,Gleb Haynatzki,Vera Haynatzka,et al. Bone miberal density-affecting denes in africans[J]. J The National Medical Association,2006,98(7):1102-1108. [2] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南[J]. 中国糖尿病杂志,2014,22(8):2-42. [3] 中华医学会骨质疏松和骨矿盐分会. 原发性骨质疏松症诊治指南[J]. 中华骨质疏松和骨矿盐疾病杂志,2011,4(1):2-17. doi: 10.3969/j.issn.1674-2591.2011.01.002 [4] Vestergard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes -a meta-analysis[J]. Osteoporosis Int,2007,18(2):427-444. [5] 董松,崔立芹,雷蕾,等. 2型糖尿病并发骨质疏松的相关危险因素[J]. 武警医学,2015,6(2):824-827. [6] Rakel A,Sheehy O,Rahme E,LeLorier J. Osteoporosis among patients with type 1 and type 2 daibetes[J]. Diabetes Metabolism,2008,34(6):193-205. [7] Franke S,Siggelkow H,Wolf G,et al. Advanced glycation endproducts influence the Mrna expression of RAGE,RANKL and various osteoblastic genes in humanosteoblasts[J]. Arch Physiol Biochen,2007,113(7):154-161. [8] Botolin S,McCabe L R. Chronic hyperglycemia modulates osteoblast gene expression through osmotic and non-osmotic pathways[J]. J Cell Biochem,2006,99(10):411-417. [9] 曹国磊,王思瑶,李思源,等. 老年男性2型糖尿病患者骨密度情况及相关影响因素[J]. 中国老年学杂志,2017,2(37):612-613. [10] Zhu G Y,Wang H F,Shi Y X,et al. Environmengt eadmium exposure and forearm bone density[J]. Biometals,2007,17(5):499-503. [11] Akesson A,Bjiellerup P,Lundh T,et al. Cadmium-induced effects on bone in a population-based study of women[J]. Environ Health Per-spect,2006,114(6):830-834. doi: 10.1289/ehp.8763 [12] 赵金秀,周学瀛,刘国仰,等. 北京地区汉族人维生素D受体基因多态性分布[J]. 中国医学科学院学报,1997,19(1):18. doi: 10.3321/j.issn:1000-503X.1997.01.007 [13] 梁伟,修玲玲,梁奕铨,等. 维生素D受体基因多态性与骨质疏松症[J]. 中山医科大学学报,2002,23(1):47-49. [14] 张红红,陶国枢,吴青. 维生素D受体基因多态性与骨质疏松的初步研究[J]. 军医进修学院学报,1998,19(1):29-30. [15] Lim S K,Park Y S,Park J M,et al. Lack of association between vitamin D receptor genotypes and osteoporosis in Koreans[J]. J Clin Endocrinol Metab,1995,80(12):3667-3681. [16] Hansen T S, Abrahamsen B, Henriksen F L, et al. Vitamin D receptor alleles do not predict bone mineral density or hone loss in Danish perimenopausal women[J]. Bone,1998,22(5):571-575. -





 下载:
下载: