Clinical Characteristics of Newly Diagnosed Type 2 Diabetes Mellitus and Influencing Factors of Glycosylated Hemoglobin Among Tibetans in Deqin
-
摘要:
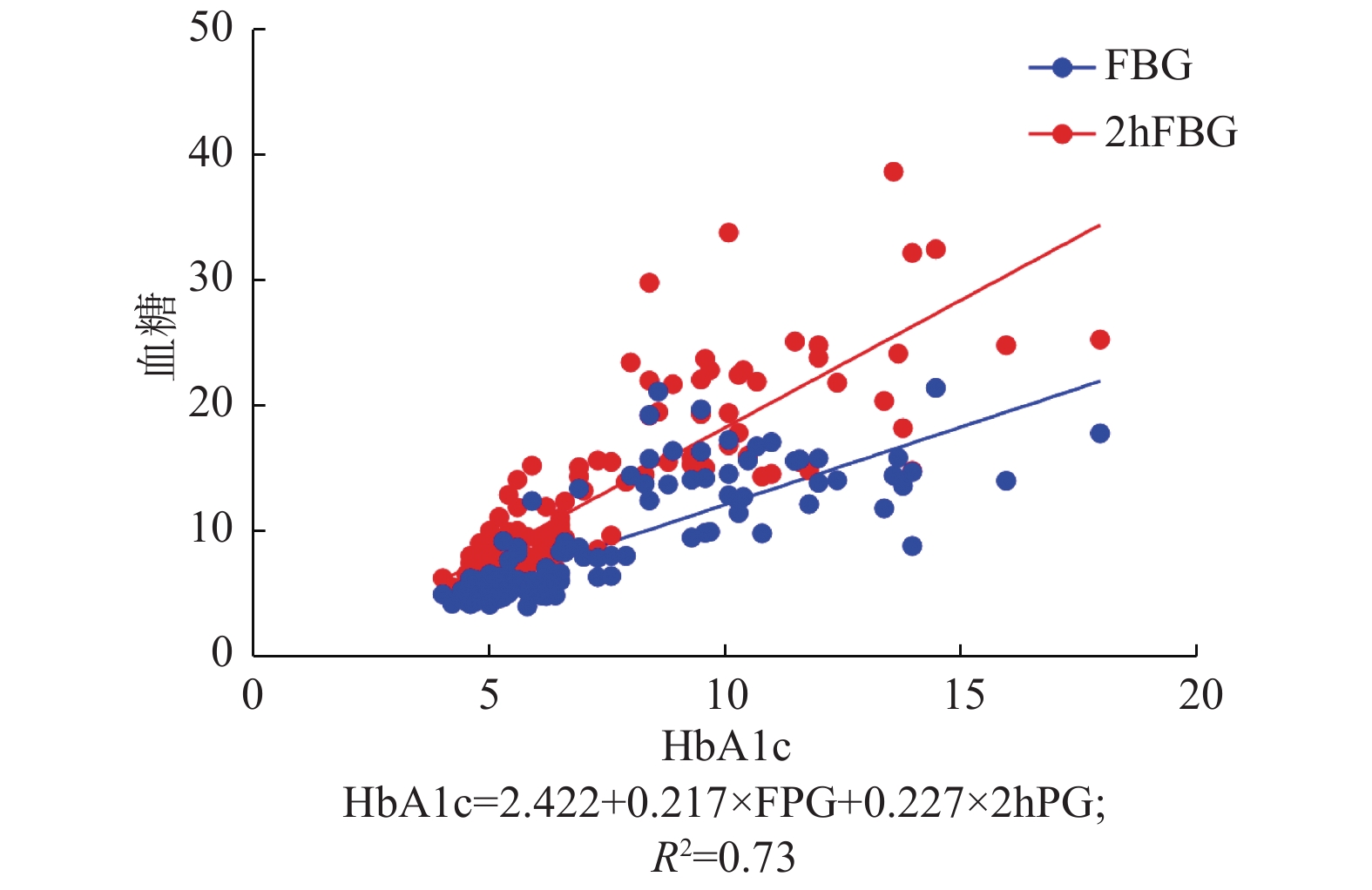
目的 探讨德钦藏族初诊断2型糖尿病患者的临床特点,分析糖化血红蛋白(HbA1c)的影响因素,了解高原藏族人群HbA1c与血红蛋白(Hb)的相关性。 方法 收集2018年5月到2020年6月德钦县医院体检和诊治的藏族患者120例的临床资料,依据血糖水平分为初诊断2型糖尿病组、糖尿病前期组和糖耐量正常组,比较3组之间一般资料及实验室指标间的差异。按血红蛋白水平,将研究对象分为高血红蛋白组及血红蛋白正常组,比较2组间空腹血糖、餐后2 h血糖及糖化血红蛋白的水平。对HbA1c与空腹血糖(FPG)、餐后2 h血糖(2 hPG)、血红蛋白进行多元线性回归分析。 结果 与糖耐量正常组相比,糖尿病组有更高的体重指数(BMI)、甘油三酯(TG)、胆固醇(TC)、低密度脂蛋白(LDL)和脂肪肝占比(P < 0.05)。3组间性别、年龄、高血压占比、高密度脂蛋白(HDL)、尿酸(UA)、红细胞(RBC)及Hb,差异无统计学意义(P > 0.05)。高血红蛋白组与正常血红蛋白组间空腹血糖、餐后2 h血糖及HbA1c,差异无统计学意义(P > 0.05)。多元线性回归分析提示空腹血糖及餐后血糖均影响HbA1c,而Hb不是HbA1c的影响因素。回归方程为HbA1c = 2.46 + 0.215×FPG + 0.228×2 hPG(R2 = 0.73,P < 0.05)。 结论 德钦藏族初诊断2型糖尿病患者有更高的BMI、TG、TC和脂肪肝占比,是早期识别糖尿病的线索。HbA1c的主要影响因素是空腹血糖和餐后2 h血糖,Hb不是HbA1c的影响因素。 Abstract:Objective To investigate the clinical characteristics of newly diagnosed type 2 diabetes mellitus (T2DM) patients among Tibetans in Deqin, analyze the influencing factors of HbA1c, and explore the correlation between HbA1c and hemoglobin (Hb) in Tibetan population at high altitude. Methods Clinical data of 120 tibetan patients with medical examination or receiving diagnosis and treatment in People’ s Hospital of Deqinfrom May 2018 to June 2020 were collected, and they were divided into three groups according to blood glucose level: newly diagnosed type 2 diabetes group, pre-diabetes group and normal glucose tolerance group. General data and laboratory indexes among the three groups were compared. According to hemoglobin level, the subjects were divided into high hemoglobin group and normal hemoglobin group. Fasting plasma glucose (FPG), two-hour postprandial plasma glucose (2 hPG) and glycosylated hemoglobin (HbA1c) levels between the two groups were compared. The relationship between HbA1c and FPG, 2 hPG and Hb was analyzed by multiple linear regression. Results Comparedwith the normal glucose tolerance group, the diabetes group had higher body mass index (BMI), triglyceride (TG), cholesterol (TC), low density lipoprotein (LDL) and fatty liver ratio (P < 0.05). There were no significant differences in gender, age, hypertension, high density lipoprotein (HDL), uric acid (UA), red blood cell (RBC) and Hb among the three groups. There was no significant difference in FPG, 2 hPG and HbA1c between the high hemoglobin group and the normal hemoglobin group (P > 0.05). Multiple linear regression analysis showed that both FPG and 2 hPG affected HbA1c, but Hb did not. The regression equation was y = 2.422 + 0.217 × FPG + 0.227 × 2 hPG (R2 = 0.73, P < 0.05). Conclusion BMI, TG, TC and fatty liver in patients with newly diagnosed type 2 diabetes mellitus in Deqin Tibetan nationality is higher, which is a clue for early recognition of diabetes. The main influencing factors of HbA1c were FPG and 2 hPG. Hb was not the influencing factor of HbA1c. -
Key words:
- Type 2 Diabetes /
- Plateau /
- Tibetan /
- Glycosylated hemoglobin
-
表 1 糖尿病组、糖尿病前期组、糖耐量正常组的资料比较[(
${x}\pm s$ ),n]Table 1. Data comparison between diabetes group,prediabetes group and glucose tolerance normal group [(
${x}\pm s$ ),n]组别 糖耐量正常组 糖尿病前期组 2型糖尿病组 χ2/t P n 31 32 57 性别(男/女) 18/15 16/16 38/19 3.119 0.21 年龄 55.5 ± 10.0 54.0 ± 9.7 53.7 ± 12.1 0.274 0.761 BMI(kg/m2) 22.0 ± 2.5 24.1 ± 2.9 26.3 ± 4.0*▲ 16.648 0.00 高血压 13 18 25 1.64 0.44 脂肪肝 7 12 30* 7.706 0.021 与糖耐量正常组比较,*P < 0.05; 糖尿病前期组比较,▲P < 0.05。 表 2 糖尿病组、糖尿病前期组、糖耐量正常组实验室资料比较(
$\bar x \pm s$ )Table 2. Comparison of laboratory data between diabetic group,prediabetes group and normal glucose tolerance group (
$\bar x \pm s$ )组别 糖耐量正常组(n = 31) 糖尿病前期组(n = 32) 2型糖尿病组(n = 57) t P FPG(mmol/L) 5.02 ± 0.43 5.96 ± 0.57 12.9 ± 3.85*▲ 114.4 0.00 2hPG(mmol/L) 6.80 ± 0.75 8.74 ± 1.16 18.9 ± 6.60*▲ 89.69 0.00 HbA1c(%) 5.05 ± 0.56 5.68 ± 0.72 9.62 ± 2.95*▲ 62.22 0.00 TG(mmol/L) 1.36 ± 0.45 1.78 ± 0.92 2.20 ± 1.66* 4.545 0.013 TC(mmol/L) 4.66 ± 0.43 5.16 ± 1.32 5.46 ± 1.38* 4.262 0.016 LDL(mmol/L) 2.45 ± 0.79 2.74 ± 0.77 2.53 ± 0.79* 1.218 0.3 HDL(mmol/L) 1.10 ± 0.30 1.11 ± 0.35 1.02 ± 0.3 1.079 0.343 UA(µmol/L) 333.5 ± 78.8 338.9 ± 79.1 319.5 ± 112.6 0.477 0.622 RBC(×109) 5.1 ± 0.6 5.0 ± 0.6 5.2 ± 0.6 1.807 0.169 Hb(g/L) 153.4 ± 15.5 151.6 ± 17.0 156.9 ± 18.8 1.408 0.249 与正常糖耐量组比较,*P < 0.05;与糖尿病前期组比较,▲P < 0.05。 表 3 高血红蛋白组与正常血红蛋白组指标的比较(
$\bar x \pm s$ )Table 3. Comparison between high hemoglobin group and normal hemoglobin group (
$\bar x \pm s$ )组别 高血红蛋白组(n = 45) 血红蛋白正常组(n = 75) t P FPG(mmol/L) 8.78 ± 4.34 9.41 ± 5.00 0.726 0.47 2hPG(mmol/L) 14.17 ± 8.18 12.45 ± 6.58 1.266 0.208 HbA1c(%) 7.79 ± 3.39 7.14 ± 2.71 1.152 0.252 表 4 HbA1c多元线性回归分析
Table 4. Multiple linear regression analysis of HbA1c
变量 偏回归系数 标准误 标准回归系数 t P VIF 常量 2.422 1.292 1.874 0.063 FPG 0.217 0.061 0.333 3.561 0.001 3.709 2hPG 0.227 0.039 0.551 5.865 0.000 3.733 Hb 0.000 0.008 0.001 0.017 0.986 1.029 -
[1] 张泽鑫,罗樱樱,刘林,等. 拉萨地区藏族成年人群糖尿病前期及糖尿病患病率初步调查分析[J]. 中国糖尿病杂志,2019,27(8):567-571. doi: 10.3969/j.issn.1006-6187.2019.08.002 [2] 姚勇利,白秀玲. 高原地区红细胞增多人群血红蛋白与HbA1c关系的初步研究[J]. 高原医学杂志,2006,16(2):31-32. [3] 蒋云海,徐文荣. 论完善健康诊疗机制于少数民族地区精准脱贫的意义—以迪庆藏族自治州德钦县为例[J]. 云南民族大学学报(哲学社会科学版),2019,36(3):95-100. [4] 中国2型糖尿病防治指南(2020年版)[J]. 中国2型糖尿病防治指南(2020年版)[J]. 中华糖尿病杂志,2021,13(4):315-409. [5] 中国高血压防治指南修订委员会等. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志,2019,24(1):24-56. doi: 10.3969/j.issn.1007-5410.2019.01.002 [6] 赵一多,张瑶,康龙丽. 短期和长期暴露于高海拔地区人群的葡萄糖稳态维持[J]. 国外医学(医学地理分册),2016,37(2):186-194. doi: 10.3969/j.issn.1001-8883.2016.02.026 [7] Wang L,Gao P,Zhang,M,et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013[J]. JAMA,2017,317(24):2515-2523. doi: 10.1001/jama.2017.7596 [8] 李彦红,刘学慧. 糖化血红蛋白与糖尿病相关性研究进展[J]. 中国城乡企业卫生,2021,36(06):70-72. [9] 孙曾梅,邬云红,李秀钧,等. 高原人群糖化血红蛋白的研究进展[J]. 华西医学,2017,32(12):1935-1938. [10] 李娅,贾德梅,赵滢,等. 高原地区不同人群糖化血红蛋白切点探讨[J]. 中华检验医学杂志,2013,36(2):142-145. doi: 10.3760/cma.j.issn.1009-9158.2013.02.011 [11] 吕雪梅,高赟,邬云红,等. 糖化血红蛋白检测对中国西藏藏族糖尿病及糖尿病前期诊断价值的研究[J]. 中国糖尿病杂志,2013,21(8):686-688. doi: 10.3969/j.issn.1006-6187.2013.08.004 [12] Ju H B,Yang L P,Fan Jian,et al. Comparison of blood sugar and glycosylated hemoglobin in type 2 diabetic patients of Chinese provinces at different altitudes[J]. Biomed Res,2014,25(3):311-316. [13] 孙曾梅,王溯源,何华,等. HbA1c对高原不同血红蛋白人群糖代谢异常诊断价值的研究[J]. 国际内分泌代谢杂志,2019,39(2):73-76. [14] 白玛康卓,巴桑次仁,次仁央宗,等. 不同海拔地区世居藏族人群高原红细胞增多症患病率的流行病学调查[J]. 第三军医大学学报,2016,38(3):220-225. [15] 唐大东. 高原地区糖尿病患者糖化血红蛋白水平测定及影响因素研究[J]. 山西医药杂志,2017,46(16):1936-1938. doi: 10.3969/j.issn.0253-9926.2017.16.007 [16] 马杜娟,罗玮,蒋艳萍,等. 高原地区肥胖与2型糖尿病及其微血管并发症的研究进展[J]. 青海医药杂志,2021,51(3):61-64. -






 下载:
下载: