Condyle Position and Symmetry in Transverse Discrepancy Patients with Temporomandibular Joint Disorders
-
摘要:
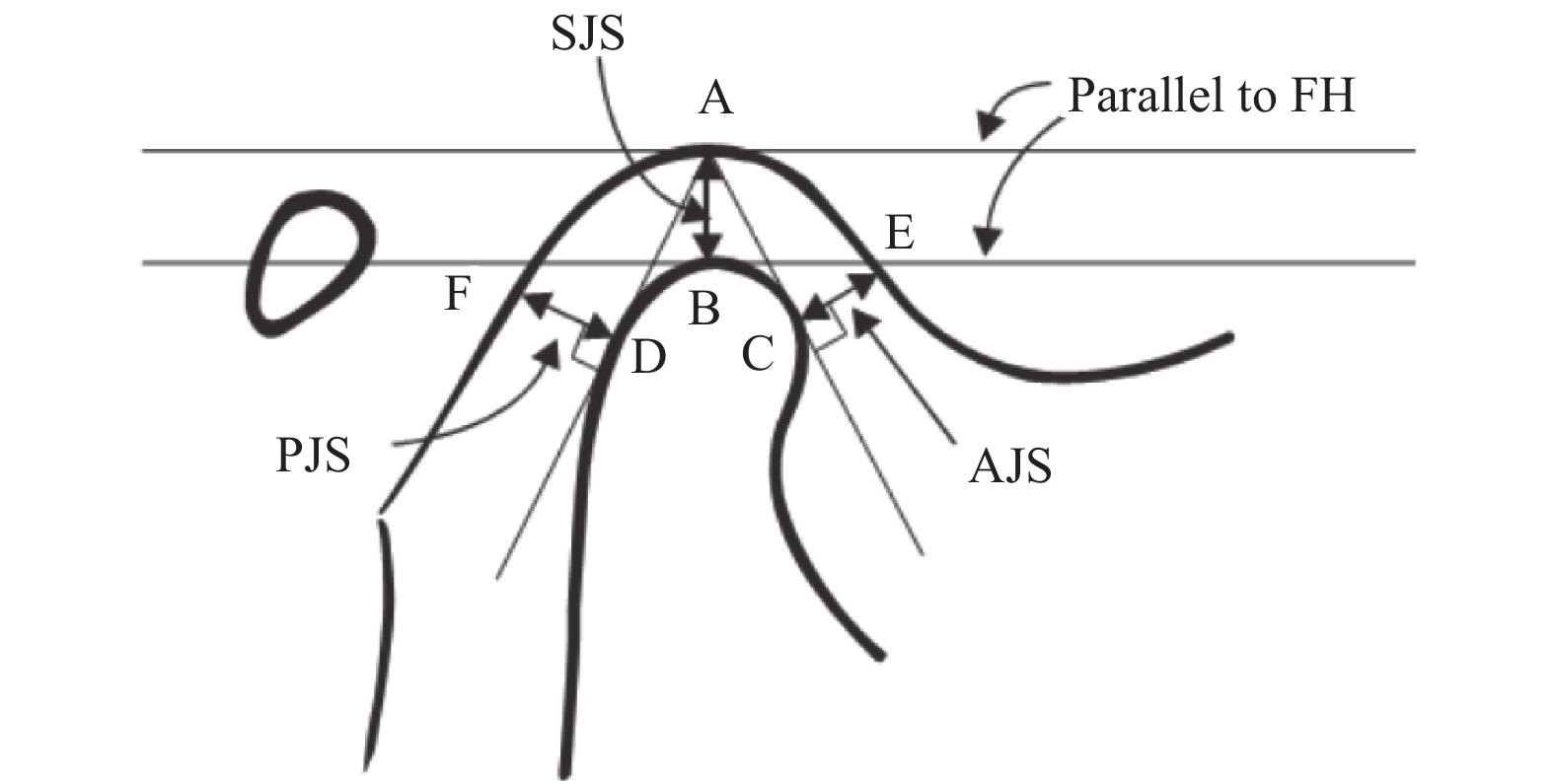
目的 研究横向不调伴TMD(Temporomandibular Disorders,颞下颌关节紊乱病)患者髁突形态、位置及下颌骨对称性与正常者的区别。 方法 纳入18名不调伴颞下颌关节病患者及18名正常者,治疗前拍摄CBCT(Cone Beam CT,锥形束CT),对比分析2组髁突形态、位置与下颌对称性的特点。 结果 (1)双侧升支高度,试验组与对照组,差异无统计学意义(P > 0.05);试验组与对照组下颌骨对称性指数,差异有统计学意义(P < 0.05);下颌骨对称性对照组优于试验组。(2)试验组与对照组相比,关节前间隙、上间隙、后间隙,差异无统计学意义(P > 0.05);对照组双侧髁突位置有相关性(P < 0.05),试验组双侧髁突位置无相关性(P > 0.05)。(3)试验组双侧髁突轴向角左侧(25.56±8.69)°,右侧(25.88±10.19)°显著大于对照组,左侧(19.77±8.18)°,右侧(19.69±7.53)°,差异有统计学意义(P < 0.05);试验组与对照组双侧髁突轴向角均有相关性(P < 0.05)。(4)髁突前后径试验组,左侧(16.47±2.03) mm,右侧(16.62±2.16) mm 与对照组的左侧(17.76±1.93) mm,右侧(17.84±2.09) mm,差异无统计学意义(P > 0.05);髁突中侧径试验组的左侧(7.12±1.3) mm,右侧(6.78±1.47) mm,与对照组的左侧(8±0.88) mm,右侧(7.76±0.92) mm,差异有统计学意义(P < 0.05)。(5)试验组双侧髁突中心与正中矢状面距,差异无统计学意义(P > 0.05);对照组双侧髁突中心与正中矢状面距,差异无统计学意义(P > 0.05);双侧髁突中心前后向,试验组与对照组相比差异无统计学意义(P > 0.05),试验组两侧髁突与正中矢状面距无相关性(P > 0.05),对照组两侧髁突与正中矢状面距有相关性(P < 0.05)。 结论 横向不调伴TMD患者下颌骨对称性、盘突关系、双侧髁突位置相关性较差,髁突小于正常者。对于横向不调患者,临床应积极评估颞下颌关节,以降低正畸治疗风险。 Abstract:Objective To investigate condylar morphology, position and mandibular symmetry in transverse discrepancy patients with temporomandibular joint disorders compared to those with normal occlusion. Methods 18 transverse discrepancy patients with temporomandibular joint disorders and 18 normal occlusion participants were selected .CBCT (Cone Beam CT) was taken before treatment, and the condylar morphology, position and mandibular symmetry of the two groups were compared and analyzed. Results (1) There was no significant difference in the height of bilateral ascending ramus between the experimental group and the control group (P > 0.05). The difference of mandibular symmetry index between experimental group and control group was statistically significant (P < 0.05). Mandibular symmetry in control group was better than that in the experimental group (P < 0.05); (2) There was no significant difference in anterior, superior and posterior joint space between the experimental group and the control group (P > 0.05). The condylar position on both sides of the control group was correlated (P < 0.05), while the condylar position on both sides of the test group was not(P > 0.05).(3)The axial condylar angles on the left side and right side of the experimental group were (25.56 ± 8.69)° and (25.88 ± 10.19)°, respectively, which are significantly higher than those in the control group, and the differences were statistically significant( P < 0.05). There was a correlation between the axial condylar angles in the two groups(P < 0.05). (4) Anteroposterior diameter of condyle in the experimental group was (16.47 ± 2.03) mm on the left side and (16.62 ± 2.16) mm on the right side.The left side of the control group was (17.76 ± 1.93) mm, and the right side was (17.84 ± 2.09) mm, and there was no significant difference between the two groups (P > 0.05). The medio-lateral diameter of condyle in the experimental group was (7.12 ± 1.3) mm on the left, (6.78 ± 1.47) mm on the right, and that in the control group was (8 ± 0.88) mm on the left, and(7.76 ± 0.92)mm on the right, the difference between the two groups was statistically significant (P < 0.05). (5) There was no significant difference in the distance between the condylar center and the median sagittal plane between the two sides in both group (P > 0.05). There was no significant difference between the experimental group and the control group in the anteroposterior orientation of the condylar center on both sides (P > 0.05). There was no correlation between the condylar and the median sagittal plane distance on both sides in the experimental group (P > 0.05), but there was correlation between the condylar and the median sagittal plane distance on both sides in the control group (P < 0.05). Conclusion In the patients with transverse discrepancy and TMD, the mandibular symmetry, disc-process relationship and bilateral condylar position had poor correlation, and the condylar was smaller than the normal occlusal patients. For patients with transverse discrepancy, TMJ should be actively evaluated to reduce the risk of orthodontic treatment. -
Key words:
- Transverse discrepancy /
- Temporomandibular joint disorders /
- Condylar process /
- Symmetry
-
表 1 试验组与对照组升支高度与对称性指数的比较[(
$\bar x \pm s$ ),mm]Table 1. Comparison of ramal height and mandibular symmetry between experimental group and control group [(
$\bar x \pm s$ ),mm]下颌对称
性测量左侧升支
高度右侧升支
高度非对称性
指数(%)试验组 47.51 ± 5.87 48.51 ± 7.08 3.94 ± 3.24 对照组 49.51 ± 3.94 48.79 ± 3.87 1.61 ± 1.13 t −1.2 −0.152 2.888 P 0.239 0.88 0.009 表 2 试验组与对照组关节间隙比较[(
$\bar x \pm s$ ),mm]Table 2. Comparison of joint space between experimental group and control group [(
$\bar x \pm s$ ),mm]关节间隙 左侧关节 右侧关节 前间隙 上间隙 后间隙 前间隙 上间隙 后间隙 试验组 1.78 ± 0.47 2.07 ± 0.73 2.02 ± 0.90 1.93 ± 0.91 2.31 ± 1.02 2.18 ± 1.46 对照组 1.83 ± 0.68 2.27 ± 0.72 1.9 ± 0.39 2 ± 0.58 2.28 ± 0.67 1.95 ± 0.43 t −0.257 −0.828 0.504 −0.262 0.097 0.651 P 0.799 0.413 0.619 0.795 0.924 0.523 表 3 试验组与对照组髁突位置比较(
$\bar x \pm s$ )Table 3. Comparison of condylar position between experimental group and control group (
$\bar x \pm s$ )分组 左侧A/P 右侧A/P r P 试验组 1.05 ± 0.52 1.06 ± 0.48 0.269 0.281 对照组 1.01 ± 0.30 1.09 ± 0.44 0.632 0.005 表 4 试验组与对照组髁突轴向角比较及相关性(
$\bar x \pm s$ )Table 4. Comparison of axial condylar angles between experimental group and control group and its Pearson’s correlation matrix (
$\bar x \pm s$ )轴向角比较及相关性 左侧髁突轴向角(°) 右侧髁突轴向角(°) r P 试验组 25.56 ± 8.69 25.88 ± 10.19 0.751 0.000 对照组 19.77 ± 8.18 19.69 ± 7.53 0.601 0.000 t 2.057 2.072 P 0.047 0.046 表 5 试验组与对照组髁突前后径与中侧径对比[(
$\bar x \pm s$ ),mm]Table 5. Comparison of greatest medio-lateral and antero-posterior diameter of the condylar between experimental group and control group [(
$\bar x \pm s$ ),mm]髁突径 试验组 对照组 t P 髁突前后径 左侧 16.47 ± 2.03 17.76 ± 1.93 −1.951 0.061 右侧 16.62 ± 2.16 17.84 ± 2.09 −1.735 0.092 髁突中侧径 左侧 7.12 ± 1.3 8 ± 0.88 −2.376 0.023 右侧 6.78 ± 1.47 7.76 ± 0.92 −2.405 0.022 表 6 试验组与对照组双侧髁突中心与矢状面距比较及两组双侧间相关性[(
$\bar x \pm s$ ),mm]Table 6. Comparison of distance from the geometric centers of the condylar processes to the mid sagittal plane between two groups, Pearson’s correlation matrix of distance from the geometric centers of the condylar processes to the mid sagittal plane between two groups [(
$\bar x \pm s$ ),mm]髁突中心与矢状面距 试验组 对照组 左侧髁突中心与矢状面距 52.69 ± 3.93 52.31 ± 3.37 右侧髁突中心与矢状面距 54.04 ± 2.82 53.36 ± 3.52 t 1.528 2.02 P 0.145 0.059 r 0.421 0.796 P 0.082 0.000 表 7 试验组与对照组髁突几何中心前后向差异比较[(
$\bar x \pm s$ ),mm]Table 7. Comparison of antero-posterior difference between the geometric center of the right and left condylar processes between two groups[(
$\bar x \pm s$ ),mm]双侧髁突中心前后向差异 髁突几何中心前后向差异 试验组 3.23 ± 2.50 对照组 2.83 ± 1.34 t 0.615 P 0.543 -
[1] Yusuf E,Buket A,Itir S,et al. Evaluation of occlusion types,pain severity,and onset of complaints in 127 patients with temporomandibular disorders:A retrospective study[J]. Cranio,2020,38(3):168-173. doi: 10.1080/08869634.2018.1509824 [2] Zynul A,Sunita S. Three-dimensional comparative evaluation of articular disc position and other temporomandibular joint,morphology in Class II horizontal and vertical cases with Class I malocclusion.[J]. Angle Orthod,2020,90(5):707-714. doi: 10.2319/121519-801.1 [3] Gye H,Jae H. Protocols for orthodontic treatment of patients with temporomandibular joint disorders[J]. Am J Orthod Dentofacial Orthop,2021,159(3):373-388. doi: 10.1016/j.ajodo.2020.09.023 [4] Chun X Z,Xiao M,Wei W,et al. Reliability of 2 methods in maxillary transverse deficiency diagnosis[J]. Am J Orthod Dentofacial Orthop,2021,159(6):758-765. doi: 10.1016/j.ajodo.2020.02.019 [5] Valentina G. Correlation between unilateral posterior crossbite, mandibular shift and jaw muscles: A review[J/OL]. Webmedcentral Orthod, 2014, 5(1): 1-6. [6] Nehal M, Amira A, Mona M, Transverse malocclusion and temporomandibular disorders: Verification of the controversy[J]. J Oral Facial Pain Headache, 2019, 33(4): 355–361. [7] Kook Y A,Kim Y. Evaluation of facial asymmetry with three-dimensional cone-beam computed tomography[J]. J Clin Orthod,2011,45(2):112-115. [8] Park J U,Kook Y A,Kim Y. Assessment of asymmetry in a normal occlusion sample and asymmetric patients with three-dimensional cone beam computed tomography:A study for a transverse reference plane[J]. Angle Orthod,2012,82(5):860-867. doi: 10.2319/102911-668.1 [9] Marcelo Reis Fraga,Andréia Fialho Rodrigues. Anteroposterior condylar position:A comparative study between subjects with normal occlusion and patients with class I,class II Division 1,and class III malocclusions[J]. Medical Science Monitor,2013,19(2):903-907. [10] Habets L L,Bezuur J N,Naeiji M,Hansson T L. The orthopantomogram,an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry[J]. J Oral Rehabil,1988,15(5):465-471. doi: 10.1111/j.1365-2842.1988.tb00182.x [11] J A McNamara. Transverse deficiency[J]. Am J Orthod Dentofacial Orthop,2000,117(5):567-570. doi: 10.1016/S0889-5406(00)70202-2 [12] Ferro F, Spinella P, Lama N. Transverse maxillary arch form and mandibular asymmetry in patients with posterior unilateral crossbite.[J] Am J Orthod Dentofacial Orthop. 2011, 140(6): 828-838. [13] Lippold C,Hoppe G,Moiseenko T,et al. Analysis of condylar differences in functional unilateral crossbite during early treatment- a randomized clinical study[J]. Orofac Orthop,2008,69(4):283-296. doi: 10.1007/s00056-008-0803-9 [14] Leonardi R,Caltabiano M,Cavallini C,et al. Condyle fossa relationship associated with functional posterior crossbite,before and after rapid maxillary expansion[J]. Angle Orthod,2012,82(6):1040-1046. doi: 10.2319/112211-725.1 [15] Karine E,Carolina F,Leandro A,et al. Three-dimensional assessment of craniofacial asymmetry in children with transverse maxillary deficiency after rapid maxillary expansion:A prospective study[J]. Orthod Craniofac Res,2020,23(3):300-312. doi: 10.1111/ocr.12370 [16] Burke G,Major P,Glover K,Prasad N. Correlation between condylar characteristics and facial morphology in class II preadolescent patients[J]. Am J Orthod dentofacial Orthop,1998,114(3):328-336. doi: 10.1016/S0889-5406(98)70216-1 [17] Katsavrias E G,Halazonetis D J. Condyle and fossa shape in class II and class III skeletal patterns:A morphometric tomographic study[J]. Am J Orthod Dentofacial Orthop,2005,128(3):337-346. doi: 10.1016/j.ajodo.2004.05.024 [18] Incesu L,Takaya Yilmaz N,Oütcen Toller M,Uzun E. Relationship of condylar position to dics position and morphology[J]. Eur J Radiol,2004,51(3):269-273. doi: 10.1016/S0720-048X(03)00218-3 [19] Wiese M,Wenzel A,Hintze H,et al. Osseous changes and condylar position in TMJ tomograms:Impact of RDC/TMD clinical diagnosis on agreement between expected and actual finding[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod,2008,106(2):52-63. doi: 10.1016/j.tripleo.2008.03.021 [20] Vivek R,Swaroopa R,Kranthi P,et al. Computed tomographic evaluation of condylar symmetry and condyle-fossa relationship of the temporomandibular joint in subjects with normal occlusion and malocclusion:A comparative study[J]. J Clin Diagn Res,2017,11(2):29-33. [21] Masi M,Lederman H M,Yamashita H K,et al. Temporomandibular joint evaluation with magnetic resonance imaging in children with functional unilateral posterior crossbite,treated with rapid maxillary expansion[J]. Am J Orthod Dentofacial Orthop,2009,136(2):207-217. doi: 10.1016/j.ajodo.2007.10.048 [22] Lee Y H,Hong I K,An J S. Anterior joint space narrowing in patients with temporomandibular disorder[J]. J Orofac Orthop,2019,80(3):116-127. doi: 10.1007/s00056-019-00172-y [23] Westesson P L,Bifano J A,Tallents R H. Increased horizontal angle of the mandibular condyle in abnormal temporomandibular joints a magnetic resonance imaging study[J]. Oral Surg Oral Med Oral Pathol,1991,72(3):359-363. doi: 10.1016/0030-4220(91)90233-3 [24] Ueki K,Nakagawa K,Takatsuka S,et al. Temporo mandibular joint morphology and disc position in skeletal class III patients[J]. J Craniomaxillofac Surg,2000,28(6):362-368. doi: 10.1054/jcms.2000.0181 [25] Yifan H,Han L,Qiuping L. Morphologic changes in idiopathic condylar resorption with different degrees of bone loss[J]. Oral Surg Oral Med Oral Pathol Oral Radio,2019,128(3):332-340. doi: 10.1016/j.oooo.2019.05.013 [26] Saccucci M,Polimeni A,Festa F,et al. Do skeletal cephalometric characteristics correlate with condylar volume,surface and shape A 3D analysis[J]. Head Face Med,2012,8(2):15-17. -






 下载:
下载: