Changes and Clinical Significance of Plasma sTREM-1,sFLT-1 and SOD Levels in Patients with Severe Pneumonia
-
摘要:
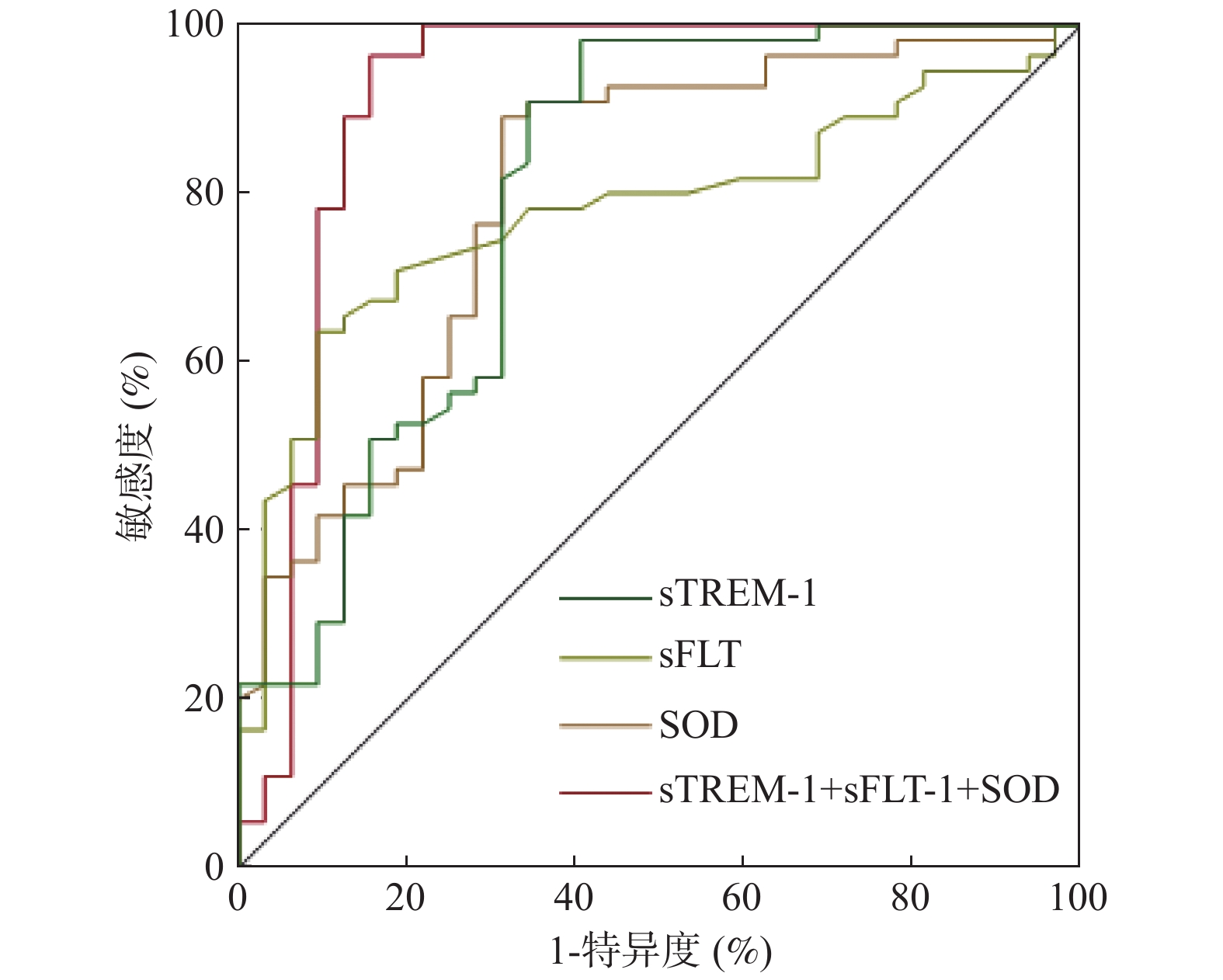
目的 探讨重症肺炎(SP)患者血浆可溶性髓系细胞触发受体-1(sTREM-1)、可溶性fms样酪氨酸激酶受体-1(sFLT-1)及超氧化物歧化酶(SOD)水平变化及临床意义。 方法 选取海口市第三人民医院(2018年1月至2019年1月)收治的150例肺炎患者,根据病情程度分为普通肺炎组(n = 63)和SP组(n = 87),治疗后随访28 d,根据是否死亡将SP组分为死亡组(n = 32)和存活组(n = 55),另选取同期60名体检健康者为对照组。对比各组血浆sTREM-1、sFLT-1、SOD水平,多因素Logistics回归分析SP患者不良预后影响因素,ROC曲线分析血浆sTREM-1、sFLT-1、SOD水平对SP患者不良预后的预测价值。 结果 对照组、普通肺炎组、SP组血浆sTREM-1、sFLT-1水平逐渐提升,SOD水平逐渐降低(P < 0.05)。多因素Logistics回归分析显示,重症监护室(ICU)时间(OR = 1.784,95%CI 1.077~2.955)、急性生理和慢性健康评估Ⅱ(APACHE Ⅱ)评分(OR = 1.834,95%CI 1.130~2.976)、sTREM-1(OR = 1.236,95%CI 1.034~1.477)、sFLT-1(OR = 1.095,95%CI 1.026~1.169)为SP患者不良预后独立危险因素,动脉血氧分压(PaO2)(OR = 0.894,95%CI 0.809~0.988)、SOD(OR = 0.933,95%CI 0.879~0.990)为保护因素(P < 0.05)。ROC曲线显示,sTREM-1+sFLT-1+SOD(AUC = 0.913,95%CI 0.833~0.963)预测SP患者不良预后的敏感度和特异度高于sTREM-1(AUC = 0.799,95%CI 0.699~0.877)、sFLT-1(AUC = 0.780,95%CI 0.678~0.861)、SOD(AUC = 0.801,95%CI 0.701~0.879)预测。 结论 SP患者血浆sTREM-1、sFLT-1水平明显提升,SOD水平明显降低,为不良预后独立影响因素,联合检测可提升不良预后预测价值。 -
关键词:
- 重症肺炎 /
- 血浆 /
- 可溶性髓系细胞触发受体-1 /
- 可溶性fms样酪氨酸激酶受体-1 /
- 超氧化物歧化酶
Abstract:Objective To investigate the changes and clinical significance of plasma levels of soluble myeloid cell trigger receptor-1 (sTREM-1), soluble Fms-like tyrosine kinase receptor-1 (sFLT-1) and superoxide dismutase (SOD) in patients with severe pneumonia (SP). Methods A total of 150 patients with pneumonia admitted to our hospital (January 2018 to January 2019) were selected and divided into normal pneumonia group (n = 63) and SP group (n = 87) according to their condition, follow-up for 28 days after treatment, SP was divided into death group (n = 32) and survival group (n = 55) according to whether or not they died, and 60 healthy people who had physical examination during the same period were selected as control group.The plasma levels of sTREM-1, sFLT-1, and SOD in each group were compared, multivariate Logistics regression was used to analyze the factors affecting the adverse prognosis of SP patients, the ROC curve analyzed the predictive value of plasma sTREM-1, sFLT-1, and SOD levels on the adverse prognosis of SP patients. Results The plasma levels of sTREM-1 and sFLT-1 in the control group, common pneumonia group and SP group gradually increased, while the SOD level gradually decreased (P < 0.05).Multivariate logistic regression analysis showed that intensive care unit (ICU) time (OR = 1.784, 95%CI: 1.077~2.955), Acute Physiology and Chronic Health Assessment Ⅱ (APACHE Ⅱ) score (OR = 1.834, 95%CI: 1.130~2.976), sTREM-1 (OR = 1.236, 95%CI: 1.034~1.477), sFLT-1 (OR = 1.095, 95%CI: 1.026~1.169) was an independent risk factor for poor prognosis in SP patients, arterial blood oxygen pressure (PaO2) (OR = 0.894, 95%CI: 0.809~0.988), SOD (OR = 0.933, 95%CI: 0.879~0.990) was a protective factor (P < 0.05).The ROC curve showed that the sensitivity and specificity of sTREm-1+sFLT-1+SOD (AUC = 0.913, 95%CI: 0.833~0.963) in predicting the poor prognosis of SP patients were higher than those of sTREm-1 (AUC = 0.799, 95%CI: 0.699~0.877), sFLT-1 (AUC = 0.780, 95%CI: 0.678~0.861), and SOD (AUC = 0.801, 95%CI: 0.701~0.879). Conclusions Plasma sTREM-1 and sFLT-1 levels in SP patients are significantly increased, and SOD levels are significantly reduced. These are independent factors affecting poor prognosis. Combined detection can increase the predictive value of poor prognosis. -
表 1 3组血浆sTREM-1、sFLT-1、SOD水平对比(
$\bar x \pm s$ )Table 1. Comparison of plasma sTREM-1,sFlt-1 and SOD levels in three groups (
$\bar x \pm s$ )组别 n sTREM-1(ng/L) sFLT-1(ng/L) SOD(KU/L) SP组 87 62.75 ± 8.24Δ* 286.97 ± 35.68Δ* 95.49 ± 22.93Δ* 普通肺炎组 63 39.16 ± 4.76Δ 241.14 ± 31.35Δ 117.04 ± 23.29Δ 对照组 60 19.01 ± 2.49 202.90 ± 28.24 131.10 ± 26.73 F - 943.481 122.268 40.386 P - 0.000 0.000 0.000 SP:重症肺炎;sTREM-1:可溶性髓系细胞触发受体-1;sFLT-1:可溶性血管内皮生长因子受体-1;SOD:超氧化物歧化酶;与对照组比较,ΔP < 0.05;与普通肺炎组比较,*P < 0.05。 表 2 SP患者不良预后影响因素的单因素分析[M(QL,QU)]
Table 2. Univariate analysis of influencing factors of poor prognosis in patients with SP [M(QL,QU)]
项目 死亡组(n = 32) 存活组(n = 55) χ2/t/Z P 性别(男/女) 21/11 28/27 1.781 0.182 年龄(岁,$\bar x \pm s$) 61.47 ± 6.28 59.87 ± 6.37 1.133 0.260 BMI(kg/m2) 24(22,25) 23(21,26) −0.436 0.663 体温(℃) 38(37,39) 38(37,38) −2.687 0.007 脉搏(次/min,$\bar x \pm s$) 116.53 ± 20.20 104.27 ± 19.23 2.815 0.006 呼吸频率(次/min,$\bar x \pm s$) 34.06 ± 7.79 31.67 ± 8.09 1.347 0.182 感染类型(细菌/混合) 28/4 45/10 0.484 0.487 肺炎场所(CAP/HAP) 27/5 48/7 - 0.705 吸烟史[n(%)] 13(40.63) 17(30.91) 0.845 0.358 饮酒史[n(%)] 7(21.88) 9(16.36) 0.409 0.522 ICU时间(d) 12(8,15) 8(6,9) −6.022 0.000 氧合指数 121.69(97.98,160.08) 140.89(88.58,207.61) −1.602 0.109 FiO2(%) 0.51(0.44,0.62) 0.40(0.28,0.47) −3.751 0.000 PaO2(mmHg) 49.78(38.38,61.75) 62.74(52.68,76.18) −3.230 0.001 PaCO2(mmHg,$\bar x \pm s$) 40.16 ± 22.20 39.16 ± 9.85 −1.324 0.189 pH值 7.37(7.30,7.43) 7.43(7.29,7.50) −1.409 0.159 MAP(mmHg,$\bar x \pm s$) 86.22 ± 17.93 84.33 ± 19.18 0.454 0.651 WBC(×109/L) 12.27(6.16,17.91) 9.91(7.69,15.40) −0.779 0.436 RBC(×1012/L,$\bar x \pm s$) 3.57 ± 0.78 3.63 ± 0.88 −0.584 0.777 PLT(×109/L,$\bar x \pm s$) 310.68 ± 84.06 225.63 ± 91.87 −0.755 0.452 收缩压(mmHg,$\bar x \pm s$) 127.88 ± 16.83 133.42 ± 18.86 −1.374 0.173 舒张压(mmHg,$\bar x \pm s$) 80.13 ± 10.29 81.45 ± 13.70 −0.476 0.635 GLU(mmol/L) 6.90(6.14,7.63) 7.36(4.80,9.75) −0.779 0.436 Scr(μmol/L) 81.31(46.90,139.79) 82.35(56.78,111.49) −0.123 0.902 BUN(mmol/L) 12.31(5.49,15.35) 9.05(6.58,10.73) −1.932 0.053 APACHEⅡ评分(分) 21(17,26) 16(14,20) −4.736 0.000 sTREM-1(ng/L,$\bar x \pm s$) 68.16 ± 7.56 59.60 ± 6.92 5.382 0.000 sFLT-1(ng/L) 314.36(305.52,326.20) 269.27(251.71,290.36) −6.153 0.000 SOD(KU/L,$\bar x \pm s$) 80.43 ± 20.20 104.25 ± 19.77 −5.376 0.000 BMI:体质指数;CAP:社区获得性肺炎;HAP:医院获得性肺炎;ICU:重症监护室;FiO2:吸入气中氧浓度分数;PaO2:动脉血氧分压;PaCO2;动脉血二氧化碳分压;MAP:平均动脉压;WBC:白细胞计数;RBC:红细胞计数;PLT:血小板计数;GLU:葡萄糖;Scr:血肌酐;BUN:血尿素氮;APACHEⅡ:急性生理和慢性健康评估Ⅱ;sTREM-1:可溶性髓系细胞触发受体-1;sFLT-1:可溶性血管内皮生长因子受体-1;SOD:超氧化物歧化酶。 表 3 SP患者不良预后影响因素的多因素Logistics回归分析
Table 3. Multivariate logistic regression analysis of influencing factors of poor prognosis in patients
变量 β SE Waldχ2 P OR(95%CI) 体温 0.145 0.109 1.755 0.183 1.157(0.943~1.433) 脉搏 0.001 0.032 0.002 0.966 0.999(0.939~1.063) ICU时间 0.579 0.257 5.062 0.024 1.784(1.077~2.955) FiO2 0.571 0.367 1.479 0.191 0.948(0.902~0.997) PaO2 −0.112 0.051 4.830 0.028 0.894(0.809~0.988) APACHEⅡ评分 0.606 0.247 6.016 0.014 1.834(1.130~2.976) sTREM-1 0.212 0.090 5.396 0.020 1.236(1.034~1.477) sFLT-1 0.091 0.033 7.513 0.006 1.095(1.026~1.169) SOD −0.069 0.030 5.250 0.022 0.933(0.879~0.990) ICU:重症监护室;FiO2:吸入气中氧浓度分数;PaO2:动脉血氧分压;PaCO2;APACHEⅡ:急性生理和慢性健康评估Ⅱ;sTREM-1:可溶性髓系细胞触发受体-1;sFLT-1:可溶性血管内皮生长因子受体-1;SOD:超氧化物歧化酶。 表 4 血浆sTREM-1、sFLT-1、SOD水平对SP患者不良预后的预测价值
Table 4. Predictive value of plasma sTREM-1,sFlt-1 and SOD levels on poor prognosis of patients with SP
指标 AUC(95%CI) 约登指数 截断值 敏感度 特异度 sTREM-1 0.799(0.699~0.877) 0.493 68.87 ng/L 65.62 83.64 sFLT-1 0.780(0.678~0.861) 0.485 299.67 ng/L 81.25 67.27 SOD 0.801(0.701~0.879) 0.578 83.27 U/L 68.75 89.09 sTREM-1+sFLT-1+SOD 0.913(0.833~0.963) 0.787 0.55 84.37 94.36 -
[1] Metlay J P,Waterer G W,Long A C,et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American thoracic society and infectious diseases society of America[J]. Am J Respir Crit Care Med,2019,200(7):e45-e67. doi: 10.1164/rccm.201908-1581ST [2] 王超,苏强,张淑文,等. 多器官功能障碍综合征病情严重度评分系统[J]. 中国医学科学院学报,2007,29(4):497-500. [3] Richards G,Levy H,Laterre P F,et al. CURB-65,PSI,and APACHE Ⅱ to assess mortality risk in patients with severe sepsis and community acquired pneumonia in PROWESS[J]. J Intensive Care Med,2011,26(1):34-40. doi: 10.1177/0885066610383949 [4] Mizgerd J P. Pathogenesis of severe pneumonia:advances and knowledge gaps[J]. Curr Opin Pulm Med,2017,23(3):193-197. doi: 10.1097/MCP.0000000000000365 [5] Zhao X,Xu L,Yang Z,et al. Significance of sTREM-1 in early prediction of ventilator-associated pneumonia in neonates:a single-center,prospective,observational study[J]. BMC Infect Dis,2020,20(1):542. doi: 10.1186/s12879-020-05196-z [6] Failla C M,Carbo M,Morea V. Positive and Negative Regulation of Angiogenesis by Soluble Vascular Endothelial Growth Factor Receptor-1[J]. Int J Mol Sci,2018,19(5):1306. doi: 10.3390/ijms19051306 [7] Ikelle L,Naash M I,Al-Ubaidi M R. Oxidative Stress,Diabetic Retinopathy,and Superoxide Dismutase 3[J]. Adv Exp Med Biol,2019,1185:335-339. doi: 10.1007/978-3-030-27378-1_55 [8] 中国医师协会急诊医师分会. 中国急诊重症肺炎临床实践专家共识[J]. 中国急救医学,2016,36(2):97-107. doi: 10.3969/j.issn.1002-1949.2016.02.001 [9] Gibot S,Cravoisy A,Levy B,etal. Soluble triggering receptor expressed on myeloid cells and the diagnosis of pneumonia[J]. N Engl J Med,2004,350(5):451-458. doi: 10.1056/NEJMoa031544 [10] Tammaro A,Derive M,Gibot S,et al. TREM-1 and its potential ligands in non-infectious diseases:from biology to clinical perspectives[J]. Pharmacol Ther,2017,177:81-95. doi: 10.1016/j.pharmthera.2017.02.043 [11] 孙印,韦海燕,何士杰. 重症肺炎患者血清suPAR、sTREM-1水平变化及意义[J]. 山东医药,2017,57(22):59-60. doi: 10.3969/j.issn.1002-266X.2017.22.022 [12] Moriyama M,Hirano T,Kawano T,etal. Toll-like receptor 4 plays an important role to enhance bacterial clearance from the nose in synergy with triggering receptor expressed on myeloid cells (TREM)-1 expression on polymorphonuclear neutrophils[J]. Int J Pediatr Otorhinolaryngol,2018,112:27-33. doi: 10.1016/j.ijporl.2018.06.025 [13] Carrasco K,Boufenzer A,Jolly L,etal. TREM-1 multimerization is essential for its activation on monocytes and neutrophils[J]. Cell Mol Immunol,2019,16(5):460-472. doi: 10.1038/s41423-018-0003-5 [14] Saleh L,Samantar R,Garrelds IM,etal. Low Soluble Fms-Like Tyrosine Kinase-1,Endoglin,and Endothelin-1 Levels in Women With Confirmed or Suspected Preeclampsia Using Proton Pump Inhibitors[J]. Hypertension,2017,70(3):594-600. doi: 10.1161/HYPERTENSIONAHA.117.09741 [15] Hao D,Li Y,Zhao G,etal. Soluble fms-like tyrosine kinase-1-enriched exosomes suppress the growth of small cell lung cancer by inhibiting endothelial cell migration[J]. Thorac Cancer,2019,10(10):1962-1972. doi: 10.1111/1759-7714.13175 [16] Yang K Y,Liu K T,Chen Y C,et al. Plasma soluble vascular endothelial growth factor receptor-1 levels predict outcomes of pneumonia-related septic shock patients:a prospective observational study[J]. Crit Care,2011,15(1):R11. doi: 10.1186/cc9412 [17] 高延秋,张华,李双凤,等. 血浆可溶性血管内皮生长因子受体1在重症肺炎患者中的诊断与预测价值[J]. 郑州大学学报(医学版),2017,52(1):63-67. doi: 10.13705/j.issn.1671-6825.2017.01.017 [18] Chang X,Yao J,He Q,et al. Exosomes From Women With Preeclampsia Induced Vascular Dysfunction by Delivering sFlt (Soluble Fms-Like Tyrosine Kinase)-1 and sEng (Soluble Endoglin) to Endothelial Cells[J]. Hypertension,2018,72(6):1381-1390. doi: 10.1161/HYPERTENSIONAHA.118.11706 [19] Karapetsa M,Pitsika M,Goutzourelas N,et al. Oxidative status in ICU patients with septic shock[J]. Food Chem Toxicol,2013,61:106-111. doi: 10.1016/j.fct.2013.03.026 -






 下载:
下载: