Study on the Morphology and Function of a Single Parathyroid Gland in situ by Endoscopy and Parathyroid Hormone Determination in Drainage Fluid
-
摘要:
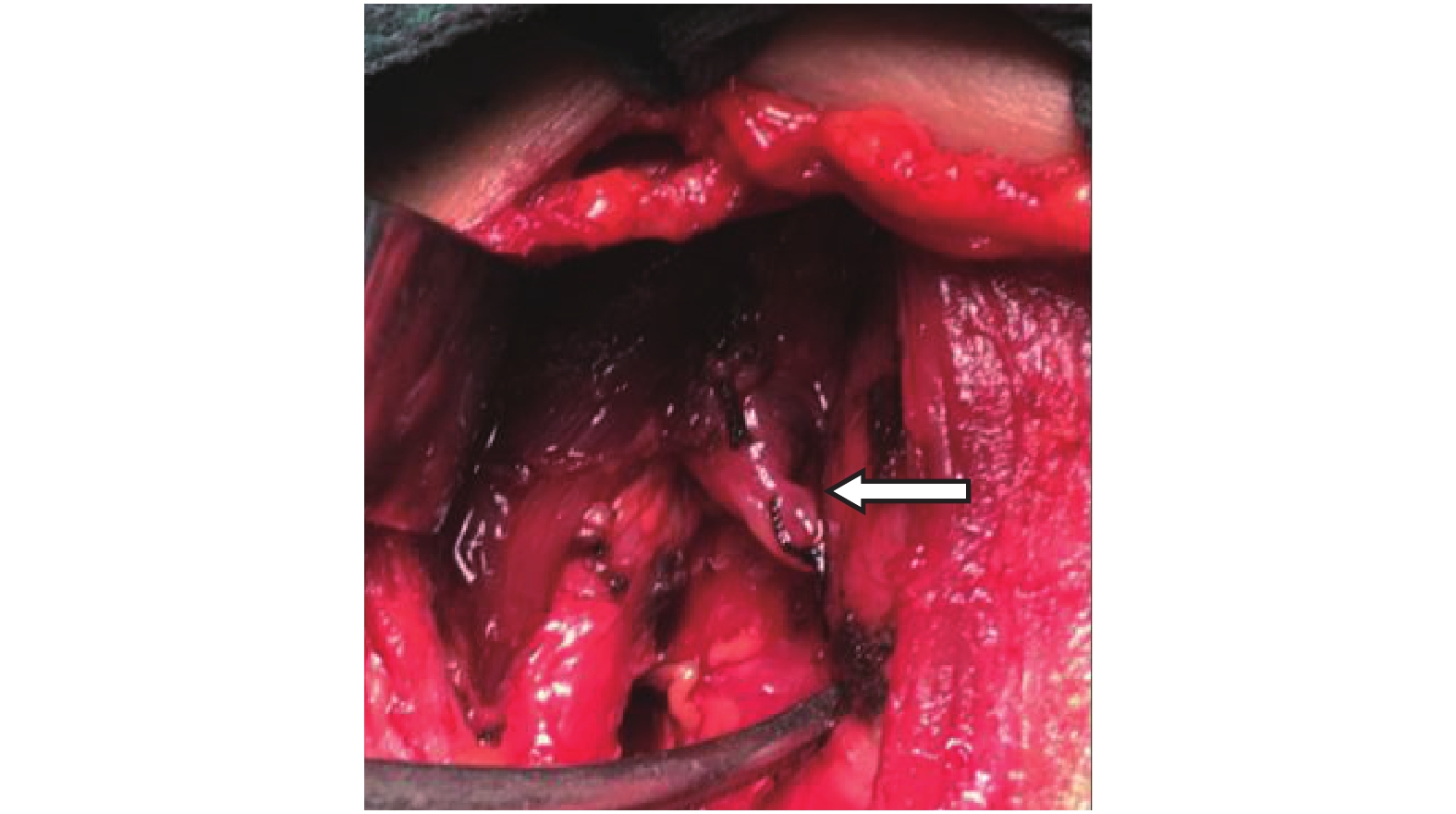
目的 探讨单枚甲状旁腺原位保留后的大体形态和功能转归变化规律,为临床上不同血供类型的甲状旁腺原位保留后的存活,功能及预后的判断提供理论依据。 方法 将行单侧甲状腺切除,术中因甲状旁腺的类型和血供原因行一枚甲状旁腺移植,原位保留另一枚甲状旁腺的42例患者作为研究对象。术后不同时段通过事先留置的引流管用0.5 cm的鼻内窥镜对目标甲状旁腺进行动态观察。术后第1、2、3天,每天上午7点至8点抽取引流液测dPTH。根据甲状旁腺原位保留的具体情况分为3个两两比较组,1组:腺体裸化面积≤50%和 > 50% 。2组:原位保留的甲状旁腺肉眼可辨认血管蒂的有无。3组:上甲状旁腺和下甲状旁腺。统计分析用SPSS17.0软件包。 结果 术后不同时间段通过内窥镜共观察目标甲状旁腺26枚,其中上甲状旁腺19枚,下甲状旁腺7枚。手术24 h后内窥镜找到并记录18枚,3枚上甲状旁腺未找到。48 h后找到并记录19枚。4枚上旁腺未找到。术中15枚上旁腺中14枚基本完整保留其血供,有肉眼可辨的血管蒂相连。1枚无明显血管蒂,该上甲状旁腺术后24 h、48 h观察腺体均为黑色,认为坏死可能,其余上旁腺无坏死征象。7枚下旁腺原位保留后裸化面积在50.0%~95.0%,只有2枚有明显的血管蒂,其余5枚无血管蒂,4枚腺体只有纤维组织膜与周围相连。术中原位保留后只有2枚有淤血表现,5枚术中变色不明显。24 h后观察到2枚有轻度淤血呈显淡褐色,1枚缺血呈黄白色;其余2枚色泽正常。48 h后2枚有轻度淤血呈显淡红褐色,5枚色泽正常,1枚缺血呈黄白色。实验数据统计学分析结果:(1)不同裸化面积,不同时间段dPTH两两比较,差异有统计学意义(P < 0.05)。术中甲状旁腺原位保留后腺体裸化面积越大,则血供破坏越大,对腺体功能影响越明显。(2)血管蒂的有无,不同时间段dPTH两两比较,差异无统计学意义(P > 0.05)。单从术后不同时间段dPTH实验数据来看,两组间存在差异(P < 0.05),有血管蒂组术后dPTH的值大于无血管蒂组,但统计学分析两者无统计学差异(P > 0.05),考虑是否和样本数量有关。 (3)上、下甲状旁腺,不同时间段dPTH两两比较,差异有统计学意义(P < 0.05)。进一步证实上甲状旁腺较下甲状旁腺更易原位保留,相对来说腺体裸化少,对血供破坏小,周围小血管和结缔组织较完整。上甲状旁腺原位保留后对血供的影响明显小于下甲状旁腺,术后功能好于下位甲状旁腺。 结论 通过内窥镜观察和监测甲状腺术后dPTH水平和变化规律完成了对单枚原位保留的甲状旁腺术后近期形态和功能的研究。术后dPTH维持在一个高水平是原位保留的甲状旁腺存活的直接证据。甲状腺术后高dPTH说明了大多数情况下手术只是影响了PTH分泌入血的途径,原位保留的甲状旁腺仍能持续分泌大量的PTH。术后dPTH 在24 h后就降至低水平,提示原位保留的甲状旁腺损伤较重,血供破坏明显,甲状旁腺的分泌功能明显低下。 Abstract:Objective To explore the changing rule of morphology and function single parathyroid gland in situ, so as to provide a theoretical basis for the survival, function and prognosis of parathyroid glands with different blood supply types. Methods Forty-two patients who underwent unilateral thyroidectomy, single parathyroid gland transplantation and retained the other parathyroid gland in situ due to the type of blood supply, were selected as objects. Target parathyroid glands were dynamically observded by nasal endoscope with inner diameter of 0.5 cm connected to previously retained drainage tube at different intervals of postoperation. The drainage liquid was collected to detect the level of dPTH in following 1st, 2nd, 3rd day between 7 and 8 am. Above patients were divided into three groups for pairwise comparison. The first group: glands shown ≤50% and>50% in naked area, the second group: vascular pedicle could be observed in parathyroid glands in situ by naked eye, the third group: the superior parathyroid gland and the inferior parathyroid gland. SPSS17.0 was used for statistical analysis. Results Twenty-six target parathyroid glands were observed by endoscope at different intervals of postoperation, 19 of which were superior parathyroid glands and the rest were inferior parathyroid glands. 18 parathyroid glands were found and recorded while 3 superior parathyroid glands were found by endoscope at 24 h of postoperation. 19 parathyroid glands were found , recorded while 4 superior parathyroid glands were not found at 48 h of postoperation. During operation, 14 of 15 superior parathyroid glands almost completely retained blood supply and contected with visible vascular pedicle, the rest 1 had no obvious vascular pedicle and exhibited black at both 24 h and 48 h of postoperation, being considered as necrosis while other superior parathyroid glands had no symptom of necrosis. The naked area of 7 inferior parathyroid glands in situ ranged from 50.0% to 95.0%, 2 of which exhibited visiable vascular pedicle while the rest 5 did not and fibrous membranes contected to periphery were observed in 4 of 5 inferior parathyroid glands. Extravasated blood was obvious in 2 inferior parathyroid glands in situ and the rest 5 was normal in clolor during operation. As for the rest 5 normal inferior parathyroid glands, 2 exhibited ecru for slight extravasated blood, 1 displayed yellowish-white for ischemia, and the rest 2 were normal at 24 h postoperation. 2 inferior parathyroid glands with slight bleeding shown reddish brown, 5 were normal in color and 1 with ischemia exhibited yellowish-white. Experimental data results of statistical analysis: (1) The difference of dPTH of different intervals on the basis of different naked area pairwise comparison was statistically significant (P < 0.05). The larger naked area of parathyroid glands remained in situ during operation induced more serious destruction on blood supply, yielding to more profound influence on function of glands. (2) The difference of dPTH of different intervals on the basis of pairwise comparison between the presence and absence of vascular pedicles was not statistically significant (P > 0.05). However, significance existed between two groups only in term of experimental data of dPTH at different intervals of postoperation. The count of dPTH from the presence of vascular pedicles was more high that of dPTH without vascular pedicles but no statistical difference was found, perhaps sample size could account for divergence. (3) The difference of dPTH of different intervals on the basis of pairwise comparison between superior and inferior parathyroid gland was statistically significant (P < 0.05). It is further confirmed that compared with inferior parathyroid gland, superior parathyroid gland was more trend in situ because of less in naked area, blood supply and more integrity of peripheral vessels and connective tissue. Conclusions The recent morphology and function of single parathyroid gland preserved in situ can be studied through endoscopic observation and monitoring of the level and changing rule of dPTH after thyroid surgery . The maintenance of dPTH at a high level after operation is a direct evidence of the survival of parathyroid glands preserved in situ.The high postoperative dPTH shows that in most cases, the operation only affects the way of PTH secretion into the blood and the parathyroid gland retained in situ can still secrete a large amount of PTH. The decrease of dPTH to a low level 24 hours after operation shows that the parathyroid gland retained in situ has serious damage, obvious blood supply destroy and depressed secretion. -
Key words:
- Thyroid surgery /
- Endoscope /
- Drainage fluid parathyroid /
- Parathyroid glands
-
表 1 不同裸化面积dPTH比较[M(P25,P75)]
Table 1. Comparison of dPTH on the basis of different naked area [M(P25,P75)]
指标 n 第1天 第2天 第3天 裸化面积≤50% 27 1920.0(1267.0,2500.0) 1723.1(315.3,2500.0) 439.0(121.8,1198.0) 裸化面积 > 50% 15 1351.1(267.6,2083.0) 492.9(79.6,1749.0) 194.0(44.7,1327.0) Z −2.055 −2.115 −1.234 P 0.040* 0.034* 0.217 不同裸化面积比较,不同时间段dPTH两两比较,差异有统计学意义,*P < 0.05。 表 2 血管蒂有无dPTH比较[M(P25,P75)]
Table 2. Comparison of dPTH between the presence and absence of vascular pedicles [M(P25,P75)]
指标 n 第1天 第2天 第3天 无血管蒂 14 1099.8(259.3,2187.3) 814.3(109.0,2321.0) 218.5(42.1,1329.3) 有血管蒂 28 1731.0(1286.9,2500.0) 1025.5(316.2,2318.8) 540.5(125.1,1204.3) Z −1.647 −0.828 −1.134 P 0.100 0.408 0.257 血管蒂的有与无比较,不同时间段dPTH两两比较,差异无统计学意义,P > 0.05。 表 3 上、下甲状旁腺dPTH比较[M(P25,P75)]
Table 3. Comparison of dPTH between superior and inferior parathyroid gland [M(P25,P75)]
指标 n 第1天 第2天 第3天 下甲状旁腺 7 418.2(77.0,2083.0) 150.0(65.9,1749.0) 45.0(34.2,194.0) 上甲状旁腺 35 1739.0(1267.6,2500.0) 1312.6(316.0,2432.0) 642.0(134.8,1231.0) Z −2.235 −2.212 −2.329 P 0.025* 0.027* 0.020* 上甲状旁腺与下甲状旁腺比较,不同时间段dPTH两两比较,差异有统计学意义,*P < 0.05。 表 4 术后甲状旁腺内窥镜观察结果(%)
Table 4. The results were observed by endoscope(%)
位置 裸化面积 血管蒂 术中变色 术后24 h 术后48 h 右侧上旁腺 20 有 黄褐色 未观察 红褐色 左侧上旁腺 80 无 褐色 黑褐色 黑褐色 左侧上旁腺 90 有 淡红黄色 红褐色 未找到 左侧上旁腺 30 有 褐色 色泽正常 色泽正常 左侧上旁腺 50 有 变色不明显 淡红褐色 淡红褐色 右侧上旁腺 70 有 红褐色 红褐色 红褐色 左侧下旁腺 95 无 变色不明显 色泽正常 色泽正常 左侧下旁腺 90 不明显 变色不明显 淡红褐色 色泽正常 右侧上旁腺 40 有 变色不明显 未找到 未观察 左侧上旁腺 40 有 变色不明显 色泽正常 未观察 右侧上旁腺 30 有 红褐色 淡黄褐色 未找到 右侧上旁腺 40 有 淡红褐色 未找到 未找到 左侧上旁腺 40 有 红褐色 未观察 淡黄红色 右侧上旁腺 30 有 变色不明显 色泽正常 色泽正常 右侧上旁腺 50 有 变色不明显 淡黄褐色 淡黄褐色 左侧下旁腺 80~90 无 变色不明显 色泽正常 色泽正常 右侧上旁腺 40 有 变色不明显 红褐色 红褐色 左侧上旁腺 40 有 稍变色 淡红褐色 淡黄褐色 右侧下旁腺 60 有 红褐色 未观察 色泽正常 左侧上旁腺 30 有 变色不明显 色泽正常 色泽正常 右侧上旁腺 40 有 无 黄白色 黄白色 左侧下旁腺 40~50 无 无 未观察 红褐色 右侧上旁腺 30 有 无 未找到 未找到 右侧下旁腺 50 无 淡红褐色 淡红褐色 淡红褐色 右侧下旁腺 90 无 变色不明显 黄白色 黄白色 左侧下旁腺 10 有 变色不明显 未观察 色泽正常 -
[1] 马云海,钱军,程若川,等. 监测甲状腺术后引流液和血清中甲状旁腺素及血钙的临床意义[J]. 中华内分泌外科杂志,2014,8(4):301-305. doi: 10.3760/cma.j.issn.1674-6090.2014.04.013 [2] 黄韬. 甲状旁腺术中损伤的预防和处理[J]. 中国实用外科杂志,2008,28(3):179-180. doi: 10.3321/j.issn:1005-2208.2008.03.009 [3] 程若川,艾杨卿,刁畅,等. 甲状腺手术中甲状旁腺显露及功能保护的临床研究[J]. 中国普外基础与临床杂志,2009,16(5):351-355. [4] Lee D Y,Cha W,Jeong W J,et al. Preservation of the inferior thyroidal vein reduces post-thyroidectomy hypocalcemia[J]. Laryngoscope,2014,124(5):1272-1277. doi: 10.1002/lary.24519 [5] Bliss R D,Gauger P G,Delbridge L W. Surgon's approach to the thyroid gland:surgical anatomy and the importance of technique[J]. World J Surg,2000,24(8):891-897. doi: 10.1007/s002680010173 [6] 陈杨,李文杰,林乐岷. 被膜解剖技术用于甲状腺全切除术[J]. 中国临床医学,2011,18(5):708-710. doi: 10.3969/j.issn.1008-6358.2011.05.049 [7] 朱精强,汪洵理,魏涛,等. 纳米碳甲状旁腺负显影辨认保护技术在甲状腺癌手术中的应用[J]. 中国普外基础与临床杂志,2013,20(9):992-994. [8] Thomusch O,Machens A,Sekulla C,et al. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery:a multivariate analysis of 5846 consecutive patients[J]. Surgery,2003,133(2):180-185. doi: 10.1067/msy.2003.61 [9] Cavicchi O,Piccin O,Caliceti U,et al. Accuracy of PTH assay and corrected calcium in early prediction of hypoparathyroidism after thyroid surgery[J]. Otolaryngol Head Neck Surg,2008,138(5):594-600. doi: 10.1016/j.otohns.2008.01.016 [10] Khairy G A,Al-Saif A. Incidental parathyroidectomy during thyroid resection:incidence,risk factors,and outcome[J]. Ann Saudi Med,2011,31(3):274-278. doi: 10.4103/0256-4947.81545 [11] Shaha A R. Revision thyroid surgery-technical considerations[J]. Otolaryngol Clin North Am,2008,41(6):1169-1183. [12] Sywak M S,palazzo F F,Yeh M,et al. parathyroid hormone assay predicts hypocalcaemia after total thyroidectomy[J]. ANZ J surg,2007,77(8):667-670. doi: 10.1111/j.1445-2197.2007.04183.x [13] Warren F M,Andersen P E,Wax M K,et al. Intraoperative parathyroid hormone levels in thyroid and parathyroid surgery[J]. Laryngosecope,2002,112(10):1866-1870. doi: 10.1097/00005537-200210000-00031 [14] 闫利英,赵瑞敏,施秉银. 甲状腺术中快速甲状旁腺素测定对预测术后低钙学症发生危险性的研究进展[J]. 中华耳鼻喉头颈外科杂志,2006,46(6):474-476. [15] 周广起,刘新梅,熊斌,等. 分化型甲状腺癌术后PTH变化及发生低钙血症的临床分析[J]. 中国普通外科杂志,2014,23(5):700-702. [16] Graciano A J,Chone C T,Fischer C A. Applicability of immediate,late or serial intact parathyroid hormone measurement following total thyroidectomy[J]. Braz J Otorhinolaryngol,2012,78(5):78-82. doi: 10.5935/1808-8694.20120012 [17] Pisanu A,Saba A,Coghe F,et al. Early prediction of hypocal-cemia following total thyroidectomy using combined intact parathyroid hormone and serum calcium measurement[J]. Langenbecks Arch Surg,2013,398(3):423-430. doi: 10.1007/s00423-012-1017-6 [18] Costanzo M,Marziani A,Condorelli F,et al. Post-thyroidectomy hypocalcemic syndrome:predictive value of early PTH. Preliminary results[J]. Ann Ital Chir,2010,81(4):301-305. -






 下载:
下载: