Correlation between Gestational Age, Biparietal Diameter and Fetal Thyroid Estimated by the 2-Dimensional Sonography
-
摘要:
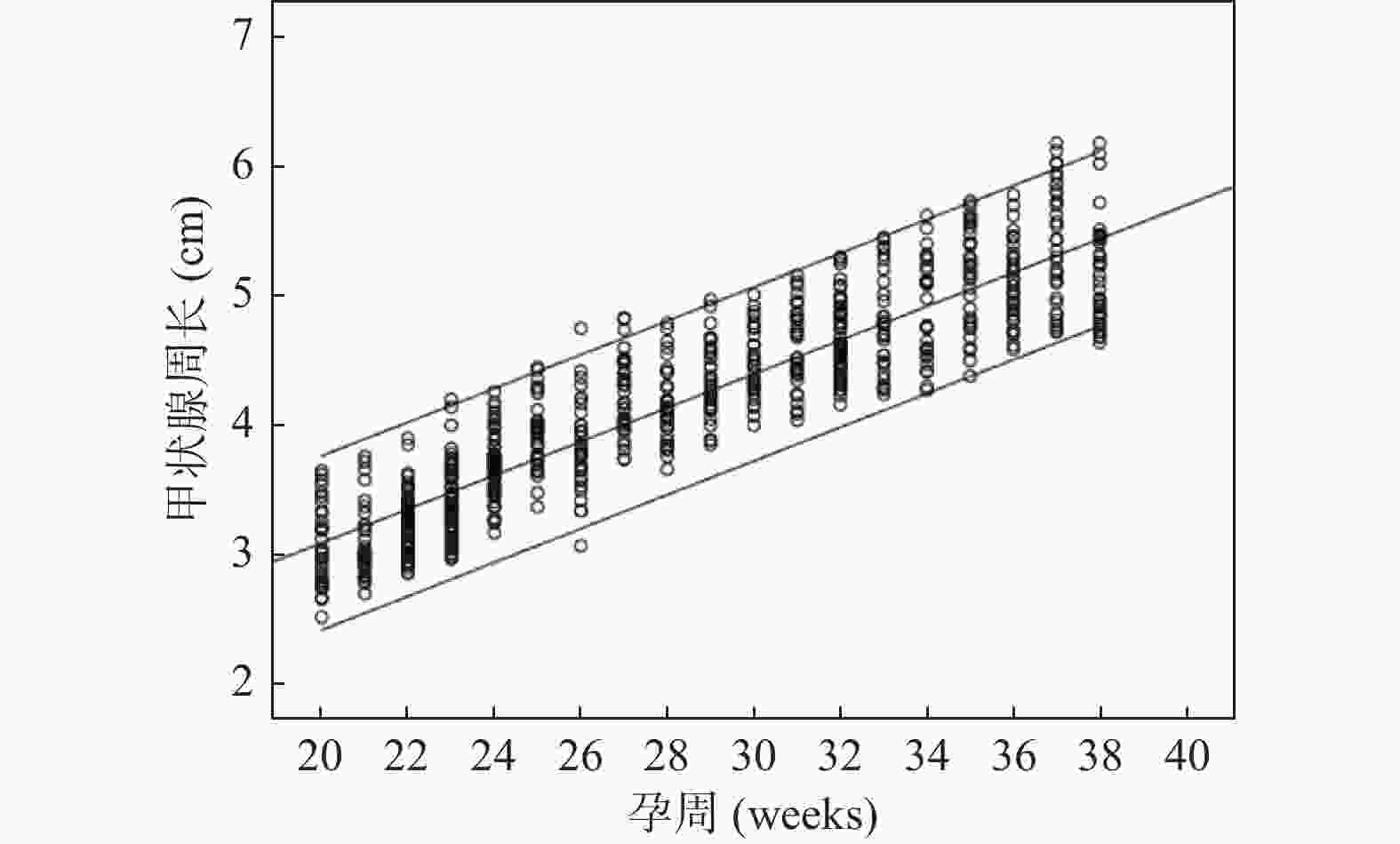
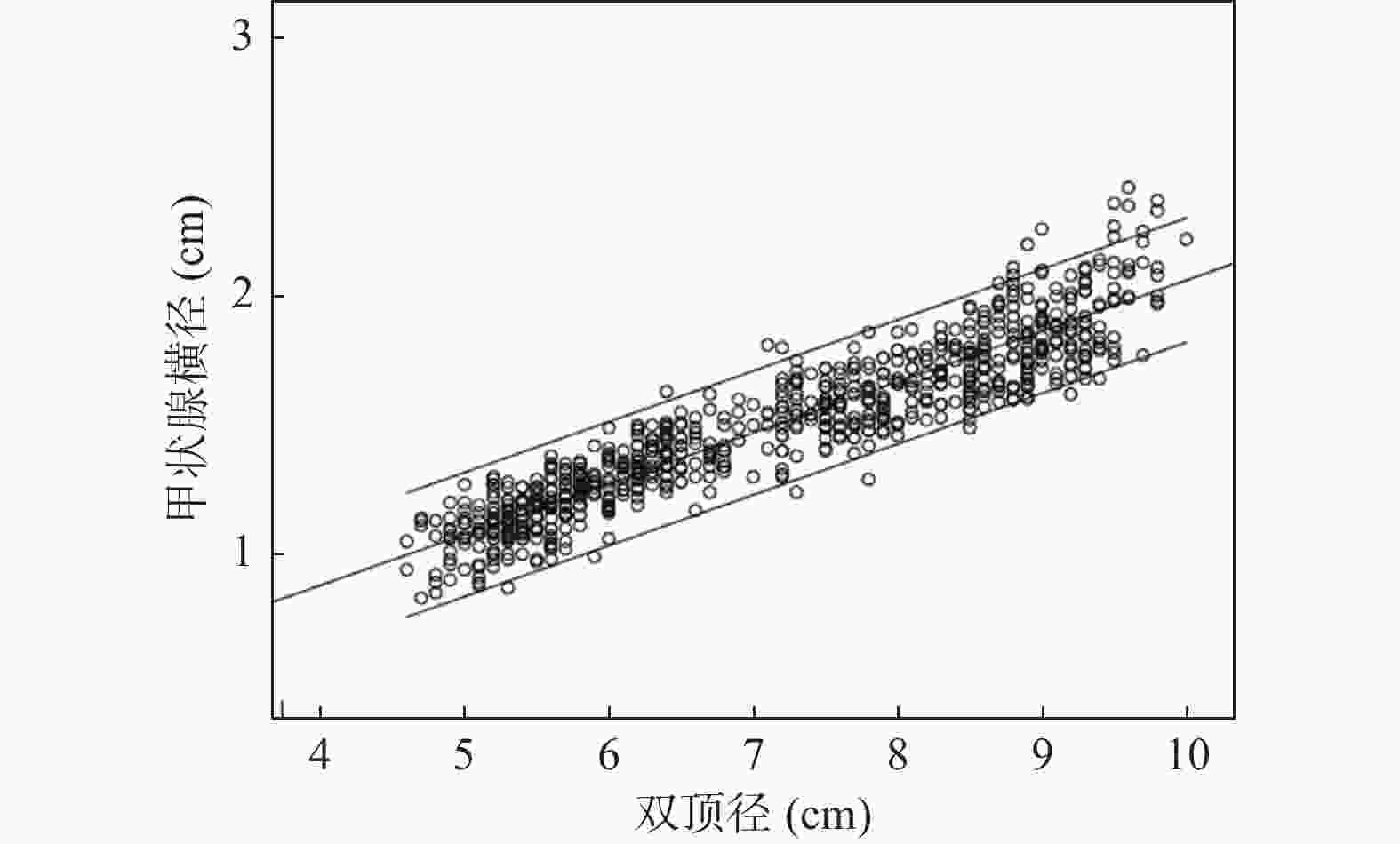
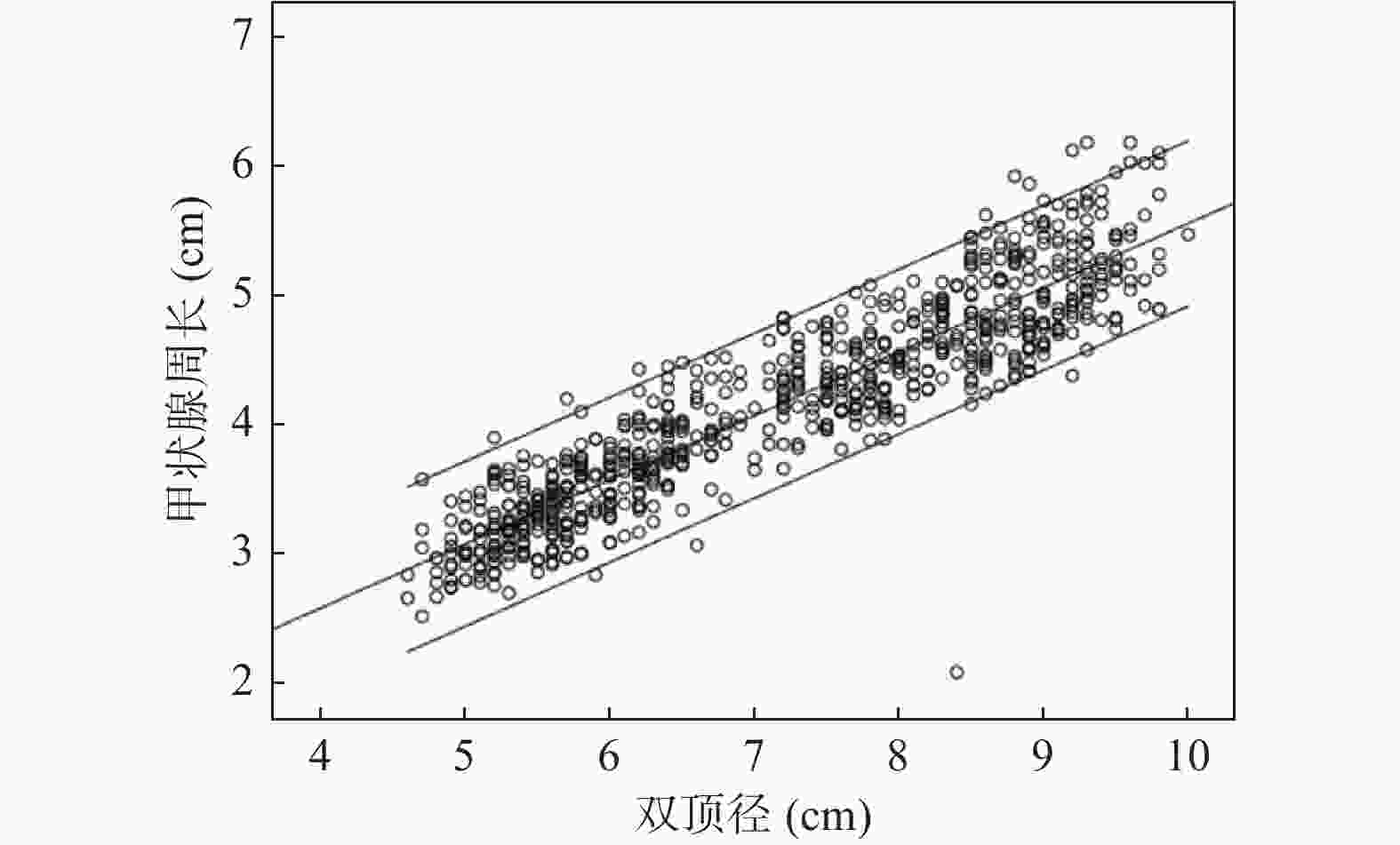
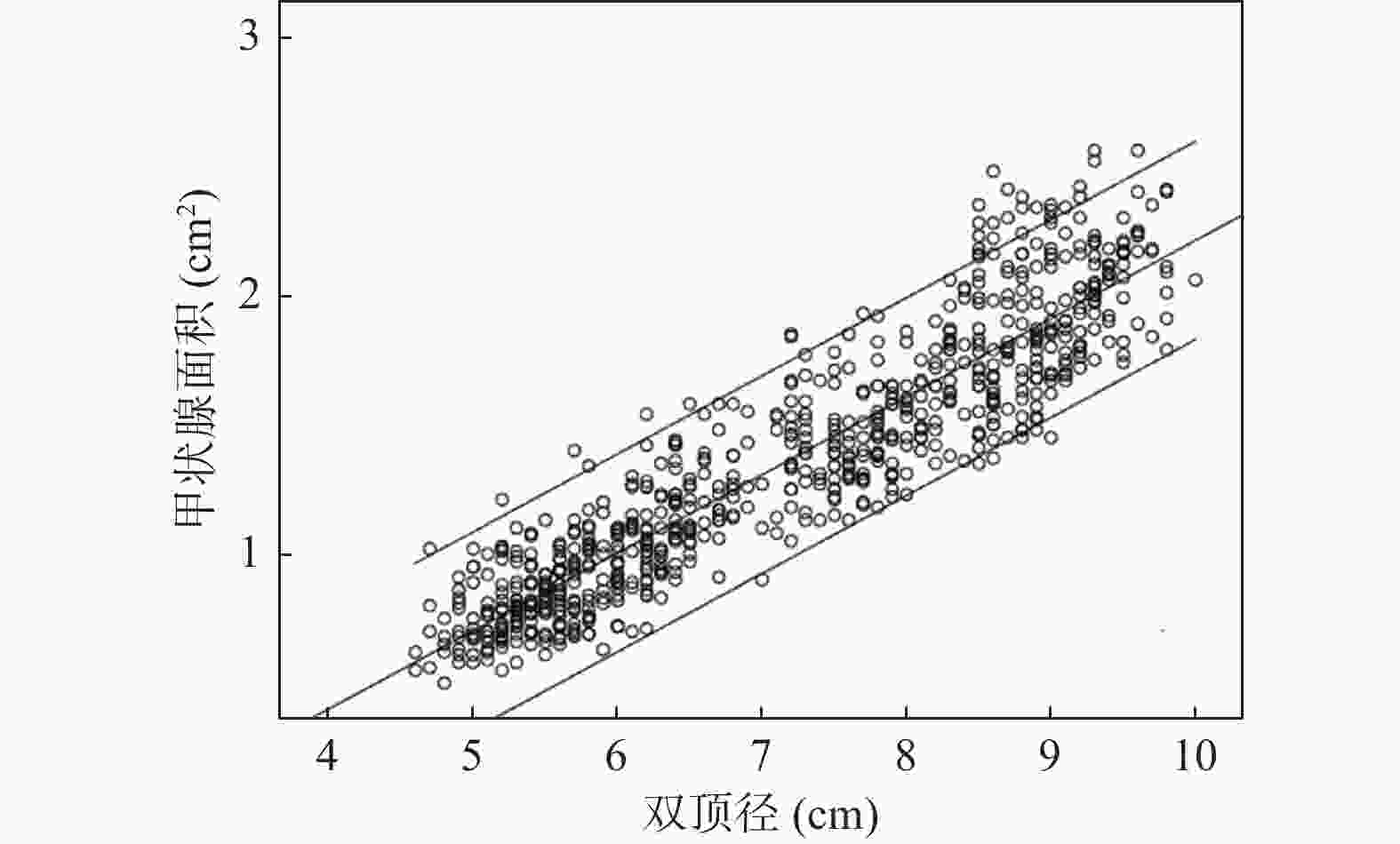
目的 利用经腹部二维超声探讨胎儿不同孕周、双顶径与甲状腺大小相关性的研究,建立胎儿甲状腺正常参考范围,用于临床评估胎儿甲状腺功能。 方法 对740名妊娠20~38周的健康孕妇进行测量胎儿甲状腺直径、周长及面积,计算5th、50th、95th百分位数,分析其分别与孕周、双顶径的相关性。 结果 获得20~38周胎儿甲状腺的直径、周长及面积的正常参考范围,发现其第5th、50th、95th百分位数分别随孕龄增加而增大,与孕龄呈高度相关性,相关系数r分别为0.909、0.904、0.913,差异有统计学意义 (P < 0.01);同时随双顶径增加而增大,与双顶径呈高度相关性,相关系数r分别为0.922、0.914、0.916,差异有统计学意义 (P < 0.01)。 结论 建立不同孕龄和双顶径胎儿甲状腺正常参考范围,不仅有助于监测高风险胎儿甲状腺的大小,及早发现甲状腺功能异常;还可通过监测甲状腺大小来评估甲状腺肿大胎儿宫内治疗的效果。 Abstract:Objective To explore the correlation between different gestational age, biparietal diameter and fetal thyroid size by transabdominal two-dimensional ultrasound, and to provide the normal reference range of fetal thyroid for clinical evaluation of fetal thyroid function. Methods The diameter, circumference and area of the fetal thyroid were measured for 740 healthy pregnant women at 20~38 weeks, the 5th, 50th and 95th percentile was calculated. The correlation between the fetal thyroid with gestational age and biparietal diameter was analyzed respectively. Results The reference range of the diameter, circumference and area of fetal thyroid at 20-38 weeks were obtained. We found the 5th, 50th and 95th percentiles increased with the gestational age, and showed a high correlation with gestational age (r = 0.909, 0.904 and 0.913, respectively), which was statistically significant (P < 0.01); And also increased with biparietal diameter, highly correlated with the biparietal diameter (r = 0.922, 0.914 and 0.916, respectively), which was statistically significant (P < 0.01). Conclusion In this study, we established the reference range of fetal thyroid according to different gestational ages and biparietal diameter, which is not only helpful to monitor the size of fetal thyroid at high risk for early detection of fetal goiter dysfunction, but also can assess the effect of intrauterine therapy on goiter fetuses by monitoring fetal thyroid size. -
Key words:
- Fetus thyroid /
- Goiter /
- 2-dimensional sonography /
- Prenatal diagnosis
-
表 1 20~38周胎儿甲状腺横径、周长和面积的百分位数
Table 1. Percentiles of fetal thyroid diameter,circumference and area during 20-38 weeks’ gestation
孕周(周) n(740) 横径(cm)百分位数 周长(cm)百分位数 面积(cm2)百分位数 5th 50th 95th 5th 50th 95th 5th 50th 95th 20 32 0.87 1.02 1.24 2.65 3.01 3.58 0.55 0.68 1.02 21 32 0.94 1.12 1.27 2.74 3.12 3.76 0.58 0.74 1.11 22 76 1.01 1.15 1.33 2.92 3.23 3.92 0.64 0.80 1.20 23 71 1.06 1.22 1.38 3.01 3.43 4.05 0.68 0.89 1.29 24 58 1.12 1.32 1.49 3.28 3.58 4.16 0.72 1.04 1.39 25 30 1.18 1.38 1.57 3.39 3.78 4.27 0.88 1.12 1.43 26 31 1.22 1.43 1.60 3.48 3.96 4.46 0.92 1.18 1.52 27 36 1.27 1.47 1.67 3.60 4.13 4.65 0.98 1.24 1.60 28 30 1.30 1.52 1.72 3.71 4.25 4.79 1.04 1.31 1.67 29 34 1.33 1.57 1.76 3.82 4.36 4.92 1.09 1.39 1.74 30 30 1.37 1.60 1.81 3.95 4.47 5.01 1.12 1.47 1.82 31 31 1.42 1.65 1.88 4.18 4.59 5.16 1.20 1.55 1.90 32 54 1.48 1.69 1.92 4.27 4.76 5.29 1.27 1.62 1.97 33 31 1.51 1.72 1.96 4.36 4.87 5.45 1.35 1.70 2.04 34 30 1.55 1.79 2.02 4.42 5.04 5.62 1.41 1.77 2.13 35 32 1.58 1.87 2.12 4.50 5.13 5.73 1.48 1.86 2.24 36 34 1.67 1.94 2.19 4.57 5.22 5.88 1.54 1.97 2.40 37 32 1.70 2.01 2.33 4.63 5.30 6.02 1.62 2.07 2.52 38 36 1.74 2.06 2.42 4.72 5.45 6.18 1.68 2.12 2.56 表 2 不同双顶径胎儿甲状腺横径、周长和面积的百分位数
Table 2. Percentiles of fetal thyroid diameter, circumference and area according to biparietal diameter
双顶径(cm) 横径(cm)百分位数 周长(cm)百分位数 面积(cm2)百分位数 5th 50th 95th 5th 50th 95th 5th 50th 95th 5.0 0.92 1.10 1.30 2.70 3.03 3.43 0.53 0.69 1.02 5.5 0.98 1.16 1.36 2.82 3.17 3.61 0.59 0.77 1.07 6.0 1.04 1.24 1.45 2.95 3.39 3.79 0.65 0.88 1.14 6.5 1.15 1.34 1.52 3.21 3.60 4.04 0.76 1.03 1.31 7.0 1.24 1.40 1.60 3.34 3.85 4.32 0.87 1.18 1.46 7.5 1.30 1.48 1.69 3.59 4.09 4.60 1.01 1.32 1.64 8.0 1.38 1.57 1.74 3.88 4.31 4.86 1.10 1.47 1.79 8.5 1.47 1.65 1.85 4.08 4.58 5.08 1.19 1.55 1.92 9.0 1.52 1.72 1.94 4.28 4.77 5.28 1.28 1.64 2.07 9.5 1.59 1.80 2.01 4.44 4.98 5.47 1.37 1.86 2.30 10.0 1.64 1.89 2.18 4.58 5.24 5.76 1.46 1.95 2.47 -
[1] Derakhshan A,Peeters R P,Taylor P N,et al. Association of maternal thyroid function with birthweight:a systematic review and individual-participant data meta-analysis[J]. The Lancet Diabetes & Endocrinology,2020,8(6):501-510. [2] Gietka-Czernel M,DeBska M,Kretowicz P,et al. Fetal thyroid in two-dimensional ultrasonography:nomograms according to gestational age and biparietal diameter[J]. Eur J Obstet Gynecol Reprod Biol,2012,162(2):131-138. doi: 10.1016/j.ejogrb.2012.02.013 [3] Glendenning P. Management of thyroid dysfunction during pregnancy and postpartum:an endocrine society clinical practice guideline[J]. J Clin Endocrinol Metab,2012,8(4):2543-2565. [4] Iijima S. Current knowledge about the in utero and peripartum management of fetal goiter associated with maternal Graves' disease[J]. Eur J Obstet Gynecol Reprod Biol X,2019,5(3):1-7. [5] Abdi H,Amouzegar A,F Azizi. Antithyroid drugs[J]. Iran J Pharm Res,2019,18(Suppl1):1-12. [6] Sarkar S,Bischoff L. Management of hyperthyroidism during the preconception phase,pregnancy,and the postpartum period[J]. Semi Reprod Med,2016,34(6):317-322. doi: 10.1055/s-0036-1593489 [7] Pearce EN. Management of thyrotoxicosis:preconception,pregnancy,and the postpartum period[J]. Endocr Pract,2019,25(1):62-68. doi: 10.4158/EP-2018-0356 [8] 董源芬,杨冬梅. 妊娠合并甲状腺功能减的研究进展[J]. 中国优生与遗传杂志,2014,22(2):134-135. [9] Min-Jung K,Yong-Hwa C,So-Young P,et al. Intra-amniotic thyroxine to treat fetal goiter[J]. Obstet Gynecol Sci,2016,59(1):66-70. doi: 10.5468/ogs.2016.59.1.66 [10] Stagnaro-Green A,Abalovich M,Alexander E,et al. Guidelines of the American thyroid association for the diagnosis and management of thyroid disease during pregnancy and postpartum[J]. Thyroid,2011,21(10):1081-1125. doi: 10.1089/thy.2011.0087 [11] 任金河,邵明鹤,梁淑霞,等. 胎儿甲状腺肿大的产前超声研究[J]. 中国全科医学,2004,7(20):1475-1476. doi: 10.3969/j.issn.1007-9572.2004.20.009 [12] 刘彦英,钱隽,李谊,等. 胎儿甲状腺的超声检测及其临床意义[J]. 中国超声医学杂志,2014,4(30):350-352. [13] 李丽雅,吕国荣,李敏,等. 二维和三维超声联合羊水相关激素测定评价胎儿甲状腺功能[J]. 中国超声医学杂志,2014,30(7):639-641. [14] Ceccaldi P F,Cohen S,Vuillard E,et al. Correlation between colored doppler echography of fetal thyroid goiters and histologic study[J]. Fetal Diagn Ther,2010,27(4):233-235. doi: 10.1159/000304269 [15] Luton D,Gac I L,Vuillard E,et al. Management of Graves’ disease during pregnancy:the key role of fetal thyroid gland monitoring[J]. J Clin Endocrinol Metab,2005,90(11):6093-6098. doi: 10.1210/jc.2004-2555 [16] Bromley B,Frigoletto F D,Cramer D,et al. The fetal thyroid:normal and abnormal sonographic measurements[J]. J Ultrasound Med,1992,11(1):25-28. doi: 10.7863/jum.1992.11.1.25 [17] Ranzini A C,Ananth C V,Smulian J C,et al. Ultrasonography of the fetal thyroid. Nomograms based on biparietal diameter and gestational age[J]. J Ultrasound Med,2001,20(6):613-617. doi: 10.7863/jum.2001.20.6.613 [18] Bernardes L S,Ruano R,Sapienza A D,et al. Nomograms of fetal thyroid measurements estimated by 2-dimensional sonography[J]. J Clin Ultrasound,2008,36(4):193-199. doi: 10.1002/jcu.20434 [19] Barbosa R M,Andrade K C,Silveira C,et al. Ultrasound measurements of fetal thyroid:reference ranges from a cohort of low-risk pregnant women[J]. Bio Med Research International,2019,17(12):1-8. [20] Marin R C,Bello-Munoz J C,Martinez G V,et al. Use of 3-dimensional sonography for prenatal evaluation and follow-up of fetal goitrous hypothyroidism[J]. J Ultrasound Med,2010,29(9):1339-1343. doi: 10.7863/jum.2010.29.9.1339 [21] Nath CA,Oyelese Y,Yeo L,et al. Three-dimensional sonography in the evaluation and management of fetal goiter[J]. Ultrasound Obstet Gynecol,2005,25(3):312-314. doi: 10.1002/uog.1863 [22] 李敏,李丽雅,吕国荣,等. 三维超声检测胎儿甲状腺体积[J]. 中国医学影像技术,2013,29(1):158-160. -






 下载:
下载: