Effect of Regional Citric acid Anticoagulation on NLRP-3 and Downstream Inflammatory Factors Expression in Patients with AKI after Cardiopulmonary Bypass
-
摘要:
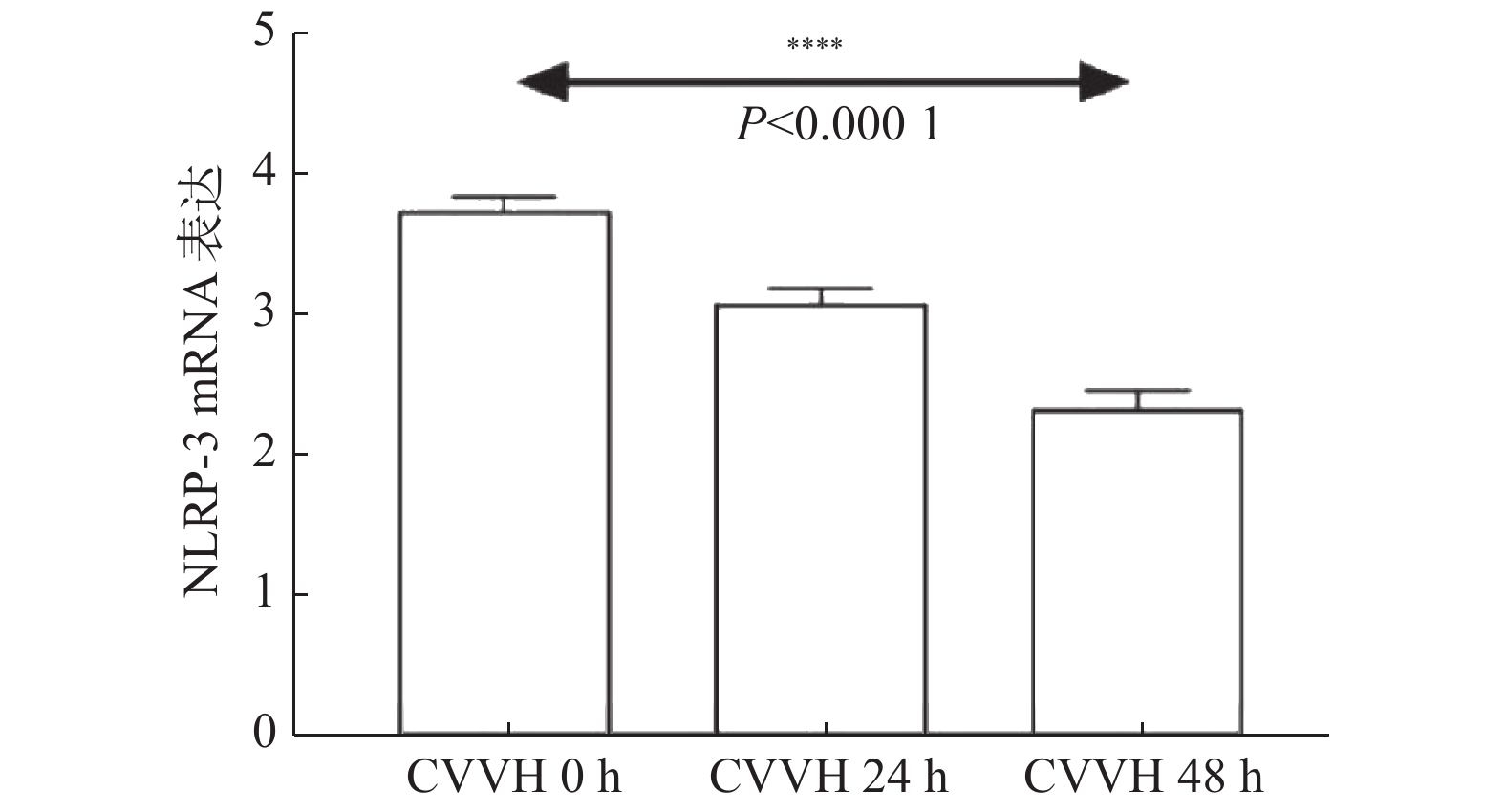
目的 探讨体外循环辅助(cardiopulmonary bypass,CPB)心脏术后发生急性肾损伤(acute kidney injury,AKI)患者使用局部枸橼酸抗凝对NLRP3及下游炎性通路表达的影响。 方法 选取2019年4月至2021年4月在昆明医科大学附属延安医院心脏大血管外科收治并接受体外循环辅助的开放性心脏手术的急性肾损伤患者共37例,其中心脏术后需行CRRT的AKI组患者31例;并随机选取心脏术后无AKI对照组32例。分别测定各组心脏超声、体外循环辅助时间、肝肾功能、心肌酶学等基线资料,采用qRT-PCR法测定NLRP-3及凋亡通路Caspase-1 mRNA相对表达量,采用ELISA法测定下游细胞因子(IL-1β、IL-6、IL-18)的表达水平,并将NLRP-3与上述各项指标进行相关性分析。 结果 与对照组相比,AKI组的体外循环辅助时间(转流时间、阻断时间、停跳时间、并行循环时间)显著延长(P < 0.05)。qRT-PCR结果显示:在AKI组中,CVVH治疗24 h、48 h后较治疗前NLRP-3和Caspase-1的mRNA表达下降(P < 0.05),且随治疗时间延长其表达进一步下降(P < 0.05)。在对照组中,术后各时间点NLRP-3和Caspase-1的mRNA表达均较术前升高(P < 0.05),在术后48 h表达开始下降(P < 0.05)。ELISA结果显示:在AKI组中,CVVH治疗24 h、48 h后较治疗前下游细胞因子IL-1β、IL-6与IL-18表达下降(P < 0.05)。在对照组中,术后各时间点下游细胞因子IL-1β、IL-6与IL-18表达均较术前升高(P < 0.05),在术后48 h表达开始下降(P < 0.05)。根据Spearman相关性分析结果提示:经局部枸橼酸抗凝CVVH治疗后的NLRP-3表达与阻断时间、停跳时间呈正相关(r = 0.514,P = 0.003;r = 0.401,P = 0.025)。 结论 体外循环心脏术后AKI患者NLRP-3及下游炎性因子表达升高;局部枸橼酸抗凝方式可有效降低NLRP-3及下游炎性因子的表达;CVVH治疗后的NLRP-3表达与阻断时间、停跳时间呈正相关。 -
关键词:
- 核苷酸结合寡聚化结构域样受体蛋白3炎性小体NLRP-3 /
- 局部枸橼酸抗凝 /
- 体外循环 /
- 急性肾损伤 /
- 炎性因子
Abstract:Objectives To explore the effects of regional citric acid anticoagulation on the expression of NLRP3 and its downstream inflammatory pathway in patients with acute kidney injury (AKI) after cardiopulmonary bypass (CPB). Methods A total of 37 patients with acute kidney injury who received open-heart surgery assisted by cardiopulmonary bypass from April 2019 to April 2021 in The Department of Cardiovascular Surgery, Yan’an Hospital Affiliated to Kunming Medical University were selected, including 31 patients in the AKI group requiring CRRT after cardiac surgery. 32 patients without AKI after cardiac surgery were randomly selected as the control group. Cardiac ultrasound, cardiopulmonary bypass auxiliary time, liver and kidney function, myocardial enzymology and other baseline data were measured in each group. The mRNA relative expression levels of NLRP-3 and apoptotic pathway caspase-1 were determined by qRT-PCR, and the expression levels of downstream cytokines (IL-1β, IL-6, IL-18) were determined by ELISA. The correlation between NLRP-3 and the above indicators was analyzed. Results Compared with the control group, the auxiliary time of cardiopulmonary bypass (cardiopulmonary bypass time, blocking time, stop time and parallel circulation time) in AKI group was significantly longer (P < 0.05). qRT-PCR results showed that in AKI group, the mRNA expressions of NLRP-3 and Caspase-1 decreased after 24 h and 48 h CVVH treatment compared with before treatment (P < 0.05), and further decreased with the prolonged treatment time (P < 0.05). In the control group, the mRNA expressions of NLRP-3 and Caspase-1 increased at all postoperative time points compared with those before surgery (P < 0.05), and began to decrease at 48h after surgery (P < 0.05). ELISA results showed that in AKI group, the expression of downstream cytokines IL-1β, IL-6 and IL-18 decreased after 24h and 48h CVVH treatment compared with before treatment (P < 0.05). In the control group, the expressions of downstream cytokines Il-1 β, Il-6 and Il-18 at all postoperative time points were increased compared with those before surgery (P < 0.05), and began to decrease 48h after surgery (P < 0.05). Spearman correlation analysis indicated that nlRP-3 expression was positively correlated with blocking time and stopping time after regional citric acid anticoagulant CVVH treatment (R = 0.514, P = 0.003; R = 0.401, P = 0.025). Conclusions The expression of NLRP-3 and downstream inflammatory factors increased in patients with AKI after cardiopulmonary bypass. Regional citric acid anticoagulation can effectively reduce the expression of NLRP-3 and downstream inflammatory factors. NLRP-3 expression after CVVH treatment was positively correlated with blocking time and stopping time. -
表 1 各引物序列
Table 1. Primer sequences
引物名称 序列5′→3′ NLRP-3 上游:CGTGAGTCCCATTAAGATGGAGT 下游:CCCGACAGTGGATATAGAACAGA Caspase-1 上游:CCGAGCTTTGATTGACTCCG 下游:TTCTGAGCCTGAGGATGTGG GAPDH 上游:GCACCGTCAAGGCTGAGAAC 下游:TGGTGAAGAACGCCAGTGGA 表 2 临床基线资料(
$\bar x$ ±$ s $ )Table 2. Clinical baseline data (
$\bar x \pm s$ )项目 对照组 AKI组 χ2/t/Z P 年龄(岁) 54.81 ± 9.08 52.74 ± 14.20 0.687 0.495 性别 男 14 19 15.302 0.000* 女 18 12 体重(kg) 59.27 ± 10.54 63.69 ± 14.03 1.420 0.161 身高(cm) 159.53 ± 9.73 162.10 ± 8.58 1.109 0.272 BMI(kg/m2) 23.26 ± 3.00 24.08 ± 4.07 0.972 0.335 WBC(×109/L) 6.71 ± 2.30 10.07 ± 17.33 1.086 0.282 Hb(g/L) 139.34(103,166) 139.10(77,242) −0.461 0.645 PLT(×109/L) 193.22 ± 39.21 160.13 ± 59.89 2.602 0.012* HCT(L/L) 0.42 ± 0.04 0.42 ± 0.08 0.085 0.933 Cr(μmol/L) 77.94(53,108) 160.03(59,1391) −2.496 0.013* BUN(mmol/L) 6.63(3.57,12.63) 9.07(2.46,44.61) −1.155 0.248 UA(μmol/L) 347.19 ± 89.75 414.48 ± 113.53 2.614 0.011* ALT(U/L) 26.66 ± 24.96 24.81 ± 16.15 0.348 0.729 AST(U/L) 32.94 ± 44.43 28.03 ± 19.87 0.563 0.576 ALP(U/L) 64.22(32,107) 76.13(37,202) −1.478 0.139 ALB(g/L) 38.09 ± 3.44 37.67 ± 4.63 0.413 0.681 CK(U/L) 167.25(29,1638) 73.35(13,304) −0.715 0.475 CK-MB(μg/L) 4.33 ± 17.65 2.43 ± 2.72 0.593 0.555 LDH(U/L) 226.34 ± 198.94 240.81 ± 108.26 0.357 0.722 LDH-MB(U/L) 36.56(23,126) 53.68(19,305) −1.900 0.057 EF(%) 56.88 ± 8.68 56.74 ± 11.78 0.051 0.959 LVDd(mm) 51.53 ± 10.11 52.61 ± 13.30 0.364 0.717 LA(mm) 41.78 ± 10.06 46.61 ± 15.52 1.471 0.146 RVd(mm) 21.34 ± 5.75 22.58 ± 7.01 0.767 0.446 RA(mm) 50.66 ± 10.66 55.68 ± 14.97 1.537 0.129 CO(L/min) 5.28 ± 2.06 5.80 ± 4.11 0.648 0.519 CI(L/min/m) 3.64 ± 1.24 3.81 ± 2.56 0.348 0.729 转流时间(min) 133.69(68,262) 245.61(81,600) −4.118 < 0.001* 阻断时间(min) 84.22(45,190) 131.42(47,313) −2.998 0.003* 停跳时间(min) 86.13(45,191) 137.58(48,314) −3.197 0.001* 并行循环时间(min) 36.19(15,82) 73.23(17,206) −3.879 < 0.001* *P < 0.05。 表 3 NLRP-3与临床多指标的相关性分析
Table 3. Correlation of NLRP-3 and clinical indexes
NLRP-3 r P 年龄 −0.168 0.365 体重 0.005 0.978 身高 0.030 0.871 BMI −0.034 0.855 WBC 0.032 0.864 Hb 0.331 0.069 PLT −0.066 0.723 HCT 0.240 0.193 Cr 0.066 0.723 BUN −0.084 0.654 UA 0.015 0.936 ALT 0.206 0.267 ALP −0.042 0.823 AST 0.128 0.493 ALB −0.097 0.604 CK 0.271 0.140 CK-MB −0.217 0.242 LDH −0.038 0.838 LDH-MB −0.070 0.707 EF 0.267 0.147 LVDd 0.016 0.934 LA −0.086 0.646 RVd −0.143 0.442 RA −0.075 0.688 CO 0.303 0.098 CI 0.289 0.114 转流时间 0.235 0.203 阻断时间 0.514 0.003* 停跳时间 0.401 0.025* 并行循环时间 −0.104 0.579 *P < 0.05。 -
[1] Englberger L,Suri R M,Li Z,et al. Clinical accuracy of RIFLE and acute kidney injury network(AKIN) criteria for acute kidney injury in patients undergoing cardiac surgery[J]. Crit Care,2011,15(1):16. [2] Pickering J W,James M T,Palmer S C. Acute kidney injury and prognosis after cardiopulmonary bypass:A meta - analysis of cohort studies[J]. Am J Kidney Dis,2015,65(2):283-293. doi: 10.1053/j.ajkd.2014.09.008 [3] Matthew H,Tezcan O B,Paul T,et al. Cardiovascular-specific mortality and kidney disease in patients undergoing vascular surgery[J]. JAMA Surg,2016,151(5):441-450. doi: 10.1001/jamasurg.2015.4526 [4] Schmitz M,Joannidis M,Czock D,et al. Regional citrate anticoagulation in renal replacement therapy in the intensive care station:Recommendations from the renal section of the DGIIN,OGIAIN and DIVI[J]. Med Klin Intensivmed Notfmed,2018,113(5):377-383. doi: 10.1007/s00063-018-0445-7 [5] Kidney disease:Improving global outcomes (KIDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury[J]. Nephron Clin Pract,2012,120(4):179-184. [6] Karkar A,Ronco C. Prescription of CRRT:A pathway to optimize therapy[J]. Ann Intensive Care,2020,10(1):32. doi: 10.1186/s13613-020-0648-y [7] Vinicius A O,Orestes F N,Ingrid K W,et al. Inflammation in renal diseases:New and old players[J]. Front Pharmacol,2019,10(10):1192. [8] Stutz A,Kolbe C,Stahl R,et al. NLRP3 inflammasome assembly is regulated by phosphorylation of the pyrin domain[J]. J Exp Med,2017,214(6):1725-1736. doi: 10.1084/jem.20160933 [9] Vives M,Hernandez A,Parramon F,et al. Acute kidney injury after cardiac surgery:Prevalence,impact and management challenges[J]. Int J Nephrol Renovasc Dis,2019,12(7):153-166. [10] Gao D,Jing S,Zhang Q,et al. Pterostilbene protects against acute renal ischemia reperfusion injury and inhibits oxidative stress,inducible nitric oxide synthase expression and inflammation in rats via the Toll-like receptor 4/nuclear factor-κB signaling pathway[J]. Exp Ther Med,2018,15(1):1029-1035. [11] Hoste E A,Vandenberghe W. Epidemiology of cardiac surgery-associated acute kidney injury[J]. Best Pract Res Clin Anaesthesiol,2017,31(3):299-303. doi: 10.1016/j.bpa.2017.11.001 [12] Wijeysundera D N,Karkouti K,Dupuis J Y,et al. Derivation and validation of a simplified predictive index for renal replacement therapy after cardiac surgery[J]. JAMA,2007,297(16):1801-1809. doi: 10.1001/jama.297.16.1801 [13] Lassnigg A,Schmidlin D,Mouhieddine M,et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery:A prospective cohort study[J]. J Am Soc Nephrol,2004,15(6):1597-1605. doi: 10.1097/01.ASN.0000130340.93930.DD [14] Clementi A,Virzì G M,Brocca A,et al. The Role of Cell-Free Plasma DNA in Critically Ill Patients with Sepsis[J]. Blood Purif,2016,41(1-3):34-40. doi: 10.1159/000440975 [15] Strobl K,Harm S,Weber V,et al. The role of ionized calcium and magnesium in regional citrate anticoagulation and its impact on inflammatory parameters[J]. Int J Artif Organs,2017,40(1):15-21. doi: 10.5301/ijao.5000558 [16] Yin L,Zhao H X,Zhang H Y,et al. Remdesivir alleviates acute kidney injury by inhibiting the activation of NLRP3 inflammasome[J]. Front Immunol,2021,12(5):652446. [17] Pang Y,Zhang P C,Lu R R,et al. Andrade-oliveira salvianolic acid B modulates Caspase-1-mediated pyroptosis in renal ischemia-reperfusion injury via Nrf2 pathway[J]. Front Pharmacol,2020,11(9):541426. [18] Lee D W,Kim J S,Kim Y,et al. Catheter-based renal sympathetic denervation induces acute renal inflammation through activation of caspase-1 and NLRP3 inflammasome[J]. Anatol J Cardiol,2019,21(3):134-141. -






 下载:
下载: