Assessment of Nasal Resistance Measurement in the Diagnosis and Treatment of OSA in Children
-
摘要:
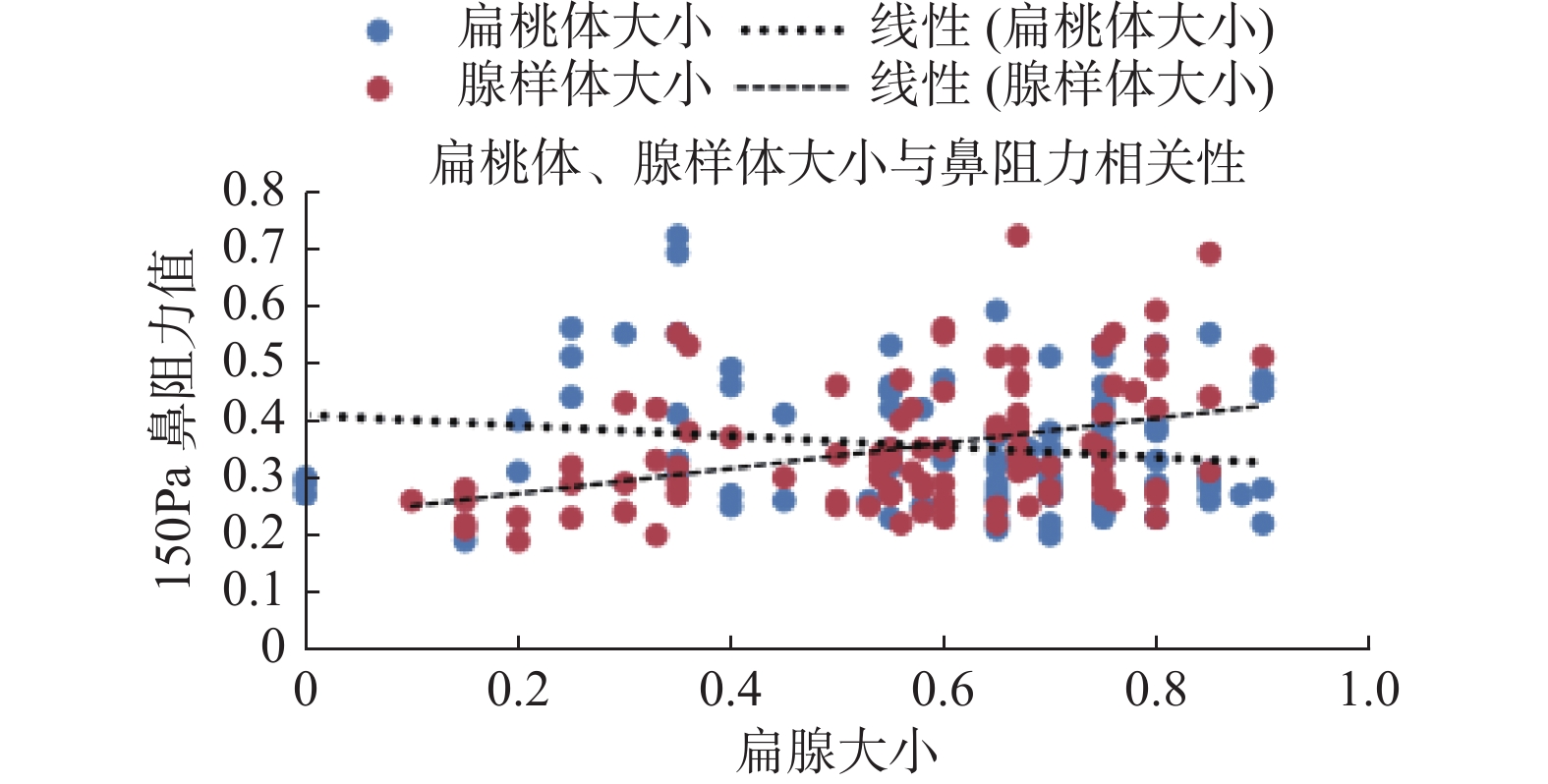
目的 通过测量儿童OSA患儿鼻阻力测定,分析鼻阻力测定在儿童OSA诊疗中的临床作用。 方法 纳入昆明医科大学附属儿童医院2019年7月至2020年7月收治的100名连续OSA患儿作为试验组,所有患儿均通过多导睡眠图(polysomnograph ,PSG)确诊,随机选取20名无睡眠障碍的健康儿童作为对照组。试验组及对照组儿童均行鼻阻力测定,根据PSG结果将试验组分为轻度OSA、中度OSA、重度OSA 3组。根据扁桃体、腺样体大小进一步将试验组为3个亚组:腺样体肥大组、扁桃体肥大组、腺扁肥大组。试验组患儿均使用低温等离子刀切除肥大的扁桃体和(或)腺样体,术后1月随访,再次行鼻阻力测定。 结果 试验组鼻阻力均值显著高于对照组(P < 0.05),而轻度OSA组、中度OSA组、重度OSA组鼻阻力均值,差异无统计学意义( P > 0.05)。 腺样体肥大组、扁腺肥大组显著高于扁桃体肥大组及对照组( P < 0.05),扁桃体肥大组鼻阻力均值与对照组比较,差异无统计学意义( P > 0.05),腺样体肥大组、扁腺肥大组2组间,差异无统计学意义( P > 0.05)。试验组鼻阻力值术后低于术前( P < 0.05)。鼻阻力值与腺样体肥大呈正相关( ρ = 0.38, P < 0.001),与OAHI值、扁桃体肥大无相关性( ρ = 0.09、ρ = -0.16, P > 0.05)。 结论 鼻阻力值在OSA儿童中明显增高,并可以反应儿童OSA腺样体肥大的程度,也可以在一定程度评估术后上气道阻力改善的效果。 Abstract:Objective To analyze the efficacy of nasal resistance measurement in the diagnosis and treatment of OSA in children by measuring the data of nasal resistance measurement in children with OSA. Methods A total of 100 OSA children admitted to our hospital from July 2019 to July 2020 were included as the experimental group. All the children were diagnosed by polysomnograph (PSG), and 20 healthy children without sleep disorders were randomly selected as the control group. The children in the experimental group and the control group were tested for nasal resistance. According to the results of PSG, the study group was divided into three groups: mild OSA, moderate OSA and severe OSA. According to the size of tonsils and adenoids, the experimental group was further divided into three subgroups: adenoid hypertrophy group, tonsil hypertrophy group, and adenotonsillar hypertrophy group. In the experimental group, hypertrophy tonsils and/or adenoids were removed by low-temperature plasma knife, and nasal resistance was measured again after 1 month follow-up. Results The mean nasal resistance value of experimental group was significantly higher than that of control group (P < 0.05), but there was no statistical difference in the mean nasal resistance of mild OSA group, moderate OSA group and severe OSA group ( P > 0.05). Adenoid hypertrophy group and adenotonsillar hypertrophy group were significantly higher than tonsil hypertrophy group and control group ( P < 0.05). There was no statistical difference in mean nasal resistance value between tonsil hypertrophy group and control group ( P > 0.05), and there was no statistical difference between adenoid hypertrophy group and adenotonsillar hypertrophy group ( P > 0.05). The nasal resistance value of the study group was lower after surgery than before ( P < 0.05). Nasal resistance value was positively correlated with adenoid hypertrophy ( ρ = 0.38, P < 0.001), but not with OAHI value and tonsil hypertrophy ( ρ = 0.09, ρ= -0.16, P > 0.05). Conclusion The nasal resistance value is significantly increased in OSA children, which reflects the degree of OSA adenoidal hypertrophy in children, and can be used to evaluate the effect of postoperative improvement of upper airway resistance to a certain extent. -
Key words:
- Nasal resistance /
- Sleep apnea /
- Obstructive /
- Children
-
表 1 试验组与对照组一般情况对比(
$ \bar x \pm s $ )Table 1. Comparison of general information between the experimental group and the control group (
$ \bar x \pm s $ )组别 n 性别(男/女) 年龄(岁) BMI(kg/m 2) 对照组 20 11/9 5.11 ± 0.81 17.12 ± 0.89 轻度OSA组 15 7/8 5.06 ± 0.79 16.98 ± 1.22 中度OSA组 33 16/17 4.96 ± 0.89 17.20 ± 0.56 重度OSA组 52 28/24 4.98 ± 0.82 17.12 ± 0.91 F 1.48 1.28 P 0.332 0.516 对照组 20 11/9 5.11 ± 0.81 17.12 ± 0.89 扁桃体肥大组 22 12/10 4.92 ± 0.89 16.97 ± 0.99 腺样体肥大组 25 13/12 4.94 ± 0.79 17.09 ± 1.02 扁腺肥大组 53 26/27 5.10 ± 0.72 16.97 ± 0.99 F 1.59 1.67 P 0.289 0.198 表 2 试验组鼻阻力均值比较结果(
$ \bar x \pm s $ )Table 2. Comparison of nasal resistance in experimental groups (
$ \bar x \pm s $ )
组别总鼻阻力值 75 Pa 150 Pa 300 Pa
对照组0.22 ± 0.05 0.27 ± 0.06 0.35 ± 0.07
轻度OSA组0.27 ± 0.05* 0.32 ± 0.09* 0.43 ± 0.09*
中度OSA组0.28 ± 0.85* 0.34 ± 0.11* 0.45 ± 0.15*
重度OSA组0.30 ± 0.10* 0.35 ± 0.12* 0.48 ± 0.16*
F3.14 3.31 4.10
P0.029 0.021 0.010
对照组0.22 ± 0.05 0.27 ± 0.06 0.35 ± 0.07
扁桃体肥大组0.22 ± 0.08 0.31 ± 0.01 0.38 ± 0.10
腺样体肥大组0.26 ± 0.07*△ 0.39 ± 0.01*△ 0.41 ± 0.11*△
扁腺肥大组0.30 ± 0.10*△ 0.46 ± 0.12*△ 0.49 ± 0.15*△
F3.75 3.84 3.92
P0.019 0.014 0.012 与对照组比较,*P < 0.05;腺样体肥大组、扁腺肥大组与扁桃体肥大组分别两两比较, △P < 0.05。 表 3 试验组术前与术后鼻阻力均值比较结果(
$ \bar x \pm s $ )Table 3. Comparison of mean nasal resistance between the experimental group before and after operation (
$ \bar x \pm s $ )项目
n总鼻阻力值 75 Pa 150 Pa 300 Pa 术前 100 0.28 ± 0.08 0.34 ± 0.10 0.46 ± 0.15 术后 100 0.26 ± 0.07* 0.30 ± 0.06* 0.40 ± 0.09* t 2.16 2.39 2.66 P 0.042 0.023 0.012 与术前比较,*P < 0.05。 -
[1] 张亚梅, 张天宇. 实用小儿耳鼻咽喉科学[M]. 北京: 人民卫生出版社, 2011: 361-352. [2] 中华耳鼻咽喉头颈外科杂志编委会,中华医学会耳鼻咽喉科学分会. 儿童阻塞性睡眠呼吸暂停低通气综合征诊疗指南草案(乌鲁木齐)[J]. 中华耳鼻咽喉头颈外科杂志,2007,42(2):83-84. doi: 10.3760/j.issn:1673-0860.2007.02.002 [3] Clement P A. Committee report on standardization of rhinomanometry[J]. Rhinology,1984,22(3):151-155. [4] 江恒谦,蔡志良,詹小燕. 腺样体术后鼻阻力测定的临床意义[J]. 包头医学院学报,2015,34(4):56-57. [5] 中国儿童OSA诊断与治疗指南制订工作组,中华医学会耳鼻咽喉头颈外科学分会小儿学组,中华医学会儿科学分会呼吸学组,中华医学会小儿外科学分会中华耳鼻咽喉头颈外科杂志编辑委员会. 中国儿童阻塞性睡眠呼吸暂停诊断与治疗指南(2020)[J]. 中华耳鼻咽喉头颈外科杂志,2020,55(8):729-747. doi: 10.3760/cma.j.cn115330-20200521-00431 [6] 沈翎,林宗通,林兴,等. 儿童阻塞性睡眠呼吸暂停低通气综合征危险因素的病例对照研究[J]. 山东大学耳鼻喉眼学报,2018,32(2):25-29. doi: 10.6040/j.issn.1673-3770.0.2018.086 [7] Brodsky L. Modern assessment of tonsils and adenoids[J]. Pediatr Clin North Am, 1989, 36(6): 1551-1569. [8] 娄凡,张铁松,马静,等. 慢性间歇性缺氧对阻塞性睡眠呼吸暂停低通气综合征儿童听功能的影响[J]. 昆明医科大学学报,2020,41(7):94-98. doi: 10.3969/j.issn.1003-4706.2020.07.019 [9] 严降雨,殷敏,李静,等. 临床评估鼻阻力的方法学研究[J]. 中国中西医结合耳鼻咽喉科杂志,2016,24(3):184-189. [10] 邓力山. 鼻阻力测定在鼻内窥镜治疗鼻阻塞疾病中的临床意义[J]. 实用临床医药杂志,2014,18(3):136-138. doi: 10.7619/jcmp.201403048 [11] Kwak P E,Gorman B K,Olson K L. Nasal gout presenting as nasal obstruction[J]. JAMA Otolaryngol Head Neck Surg,2013,139(4):411-413. doi: 10.1001/jamaoto.2013.220 [12] 黄辉,钟晓燕,廖艳萍,等. 鼻阻力指标检测在阻塞性睡眠呼吸暂停综合征患者中的应用价值[J]. 海南医学,2015,26(11):1583-1585. doi: 10.3969/j.issn.1003-6350.2015.11.0567 [13] Marcus C L,Brooks L J,Draper K A,et al. Diagnosis and management of childhood obstructive sleeop apnea syndrome[J]. Pediatrics,2012,130(3):e714-e755. doi: 10.1542/peds.2012-1672 [14] 韩勇. 鼻阻力指标检测在阻塞性睡眠呼吸暂停综合征患者中的应用价值[J]. 临床医药文献杂志,2018,5(61):79. -






 下载:
下载: