The Currative Effect of Biological Lengthened Handle Total Hip Arthroplasty in the Treatment of Subtrochanteric Fracture Combined with Femoral Head Necrosis
-
摘要:
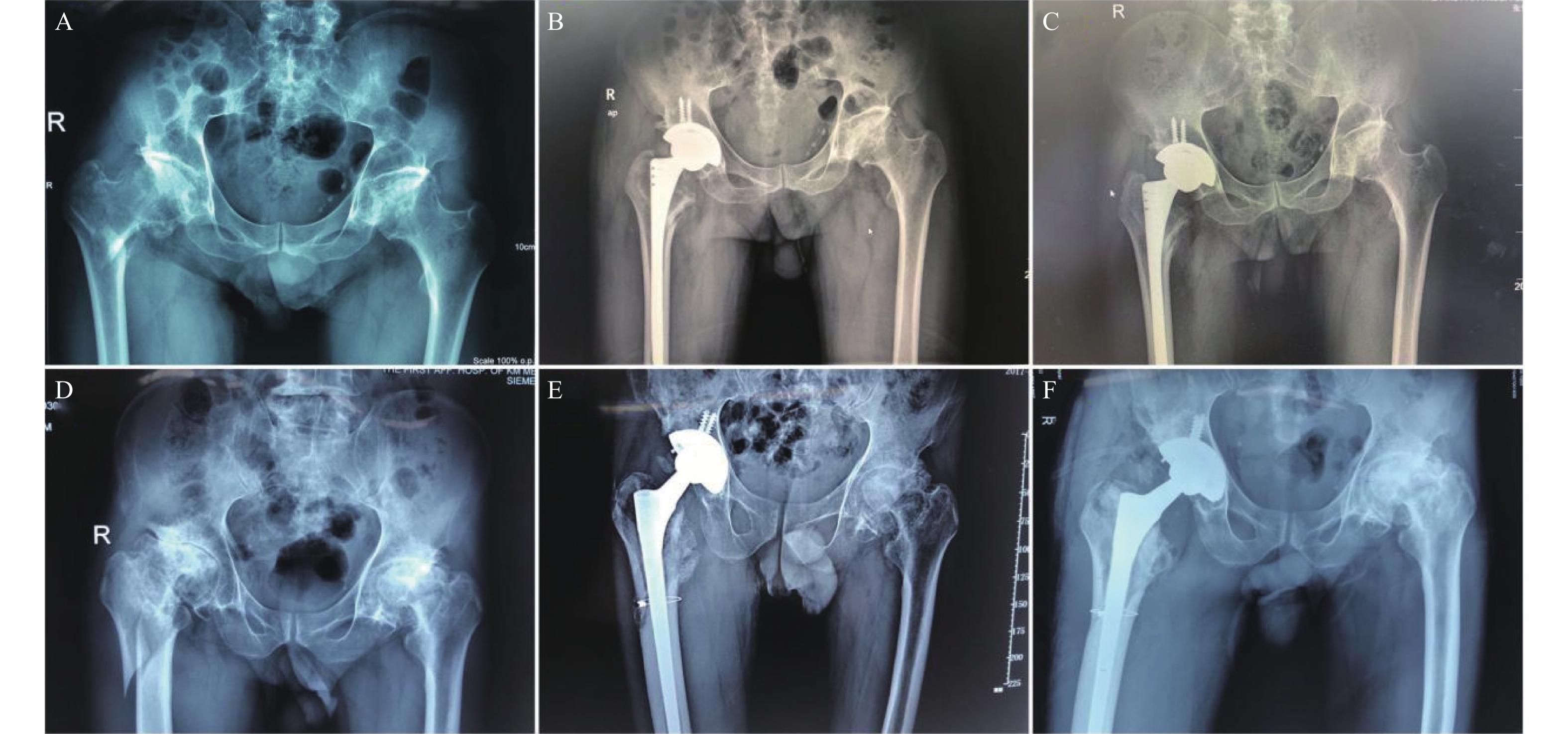
目的 探讨使用生物型加长柄行全髋关节置换治疗股骨转子下骨折合并股骨头缺血性坏死的可行性及临床疗效。 方法 回顾性分析2016年1月至2020年1月收治的88位患者,其中30例股骨转子下骨折合并股骨头缺血性坏死行Ⅰ期生物型加长柄关节置换(实验组),20例单纯转子下骨折组行PFNA内固定术(PFNA组),32例单纯股骨头缺血性坏死行人工关节置换术(关节置换组),比较3组的手术时间、围术期出血量、术后住院天数;比较实验组与PFNA组骨折愈合时间;比较实验组与关节置换组术后1,3,6月和末次随访的髋关节Harris评分。 结果 实验组手术时间高于PFNA组及关节置换组,差异有统计学意义(P < 0.05);3组围术期出血量、术后下地活动时间及住院天数,差异有统计学意义(P < 0.05);实验组与PFNA组骨折愈合时间,差异无统计学意义,实验组与关节置换组术后髋关节Harris评分,差异无统计学意义(P < 0.05)。 结论 生物型加长柄Ⅰ期行全髋关节置换治疗股骨转子下骨折合并股骨头缺血性坏死可取得良好的临床疗效,骨折愈合时间与PFNA术无明显差异。 Abstract:Objective To investigate the feasibility and clinical effect of total hip replacement with the biologically lengthened stem in the treatment of subtrochanteric fractures combined with the necrosis of femoral head. Methods A total of 88 patients admitted from January 2016 to January 2020 were analyzed retrospectively. Among them, 30 cases of subtrochanteric fractures with the avascular necrosis of the femoral head underwent stage I biotype long-stem joint replacement (experimental group), 20 cases of simple subtrochanteric fracture group underwent PFNA internal fixation (PFNA group), and 32 cases of simple avascular necrosis of the femoral head underwent the artificial joint replacement (joint replacement group). The operation time, perioperative blood loss and postoperative hospitalization were compared among the three groupsand the fracture healing time between the experimental group and the PFNA group was compared so as to compare the hip Harris scores of the experimental group and the joint replacement group 1, 3, 6 months after the surgery and the last follow-up. Results The operation time of the experimental group was higher than those of the PFNA group and the joint replacement group, and the difference was statistically significant; The three groups had the statistically significant differences in perioperative blood loss, time of postoperative activities and the length of hospital stay; There was no significant difference in fracture healing time between the experimental group and the PFNA group and there was no statistically significant difference in the Harris score of the hip joint between the experimental group and the joint replacement group. Conclusion The total hip arthroplasty for the treatment of subtrochanteric fractures with the necrosis of femoral head can achieve good clinical results. There is no significant difference between fracture healing time and PFNA surgery. -
表 1 一般资料比较(n)
Table 1. Comparsion of general data (n)
一般情况 实验组 PFNA组 关节置换组 年龄(岁) 69.43 ± 5.32 71.05 ± 8.47 68.16 ± 6.25 侧别(左) 18 12 20 (右) 12 8 12 骨折分型(RUSSELL-TAYLOR IA型) 6 6 (RUSSELL-TAYLOR IB型) 24 14 股骨头坏死分期(ARCO III期) 0 8 (ARCO IV期) 30 24 表 2 临床疗效比较
Table 2. Comparsion of clinical outcomes
组别 手术时间(min) 术中出血量(mL) 术后下地活动时间(d) 住院天数(d) 骨折愈合时间(d) 实验组 92.97 ± 11.75 198.13 ± 31.74 4.53 ± 1.41 8.20 ± 1.49 12.23 ± 1.26 PFNA组 67.95 ± 14.00 152.25 ± 13.65 12.80 ± 2.02 8.25 ± 1.83 12.25 ± 1.25 关节置换组 64.63 ± 9.07 100.78 ± 22.83 2.41 ± 0.56 8.19 ± 1.80 H/F 61.098 277.314 67.266 0.063 P < 0.001* < 0.001* < 0.001* 0.969 0.975 *P < 0.05。 表 3 随访资料比较(分)
Table 3. Comparsion of follow-up data (scores)
组别 术后1月Harris评分 术后3月Harris评分 术后6月Harris评分 末次随访Harris评分 实验组 78.53 ± 4.754 80.23 ± 4.739 83.90 ± 4.020 86.83 ± 3.788 关节置换组 77.45 ± 5.549 79.75 ± 6.060 85.30 ± 4.857 88.05 ± 4.524 T 0.715 0.301 −1.068 −0.993 P 0.479 0.766 0.293 0.327 -
[1] Egol K A. Subtrochanteric femur fracture below an arthritic hip:Opinion:Open reduction and internal fixation in conjunction with total hip arthroplasty[J]. J Orthop Trauma,2005,19(1):60-61. doi: 10.1097/00005131-200501000-00012 [2] Gallagher C A,Jones C W,Kimmel L,et al. Osteoarthritis is associated with increased failure of proximal femoral fracture fixation.[J]. Int Orthop,2019,43(5):1223-1230. doi: 10.1007/s00264-018-4014-8 [3] Bohndorf K,Roth A. Imaging and classification of avascular femoral head necrosis[J]. Orthopade,2018,47(9):729-734. [4] Rizkalla J M,Nimmons S J B,Jones A L. Classifications in brief:The russell-taylor classification of subtrochanteric hip fracture[J]. Clin Orthop Relat Res,2019,477(1):257-261. [5] 周宗科,翁习生,曲铁兵,等. 中国髋、膝关节置换术加速康复——围术期管理策略专家共识[J]. 中华骨与关节外科杂志,2016,9(1):1-9. doi: 10.3969/j.issn.2095-9985.2016.01.001 [6] 张盘军,王勇,蒋建农,等. Ⅰ期全髋关节置换术治疗股骨转子下骨折合并同侧股骨头坏死[J]. 实用骨科杂志,2020,26(9):778-781. [7] 邓煜,夏于欣,白新文,等. 生物型加长柄髋关节置换治疗老年不稳定性转子间骨折中股骨近端不同重建方法的疗效对比[J]. 中国组织工程研究,2019,23(12):1805-1811. doi: 10.3969/j.issn.2095-4344.1120 [8] Kim J Y,Kong G M. Subcapital femoral neck fracture after treatment of an intertrochanteric fracture with proximal femoral intramedully nail[J]. Coll Physicians Surg Pak,2016,26(1):78-79. [9] 徐风瑞,何明武,姚忠军,等. PFNA内固定与人工股骨头置换术治疗高龄骨质疏松性股骨粗隆间骨折的比较[J]. 中国骨与关节损伤杂志,2016,31(2):130-133. doi: 10.7531/j.issn.1672-9935.2016.02.006 [10] Cui Q,Liu YS,Li DF,et al. Cemented hip hemiarthroplasty clinical observations on unstable intertrochanteric fracture in elderlies[J]. Eur J Trauma Emerg Surg,2016,42(5):651-656. doi: 10.1007/s00068-015-0566-0 [11] 熊健斌,彭伟秋,孙宏志. 髋部骨折高龄患者术后死亡的相关因素回顾性分析[J]. 中国矫形外科杂志,2014,22(18):1066-1069. [12] 陈楠生,林炳基,张子宏. 交锁髓内钉与锁定钢板治疗股骨干骨折的疗效比较[J]. 实用手外科杂志,2019,33(2):245-246. doi: 10.3969/j.issn.1671-2722.2019.02.039 [13] 曹启斌,舒钧,浦波. 股骨转子下骨折手术治疗及分型进展[J]. 中国矫形外科杂志,2012,20(10):906-908. [14] Hassankhani E G,Omidi-Kashani F,Hajitaghi H,et al. How to treat the complex unstable intertrochanteric fractures in elderly patients? DHS or arthroplasty[J]. Arch Bone Jt Surg,2014,2(3):174-179. [15] 李建刚,李超英. 老年股骨颈骨折半髋置换选择骨水泥型和生物型假体的临床观察[J]. 中国矫形外科杂志,2016,24(14):1258-1263. [16] Talsnes O,Vinje T,Gjertsen J E,et al. Perioperative mortality in hip fracture patients treated with cemented and uncemented hemiprosthesis:A register study of 11,210 patients[J]. Int Orthop,2013,37(6):1135-1140. doi: 10.1007/s00264-013-1851-3 [17] Vermesan D,Prejbeanu R,Poenaru D V,et al. Do intramedullary implants improve survival in elderly patients with trochanteric fractures? A retrospective study[J]. Clin Ter,2015,166(3):e140-e145. [18] Middleton R G,Uzoigwe C E,Young P S,et al. Peri-operative mortality after hemiarthroplasty for fracture of the hip:Does cement make a difference?[J]. Bone Joint J,2014,96-B(9):1185-1191. doi: 10.1302/0301-620X.96B9.33935 [19] 蒋垚,张先龙,沈灏,等. 全髋人工关节置换术治疗股骨转子下骨折伴股骨头缺血性坏死[J]. 中华创伤杂志,2005,21(11):16-19. -






 下载:
下载: