EGFR Gene Mutation State and Its Clinical Significance in Multi-nodular Lung Adenocarcinoma in Yunnan Province
-
摘要:
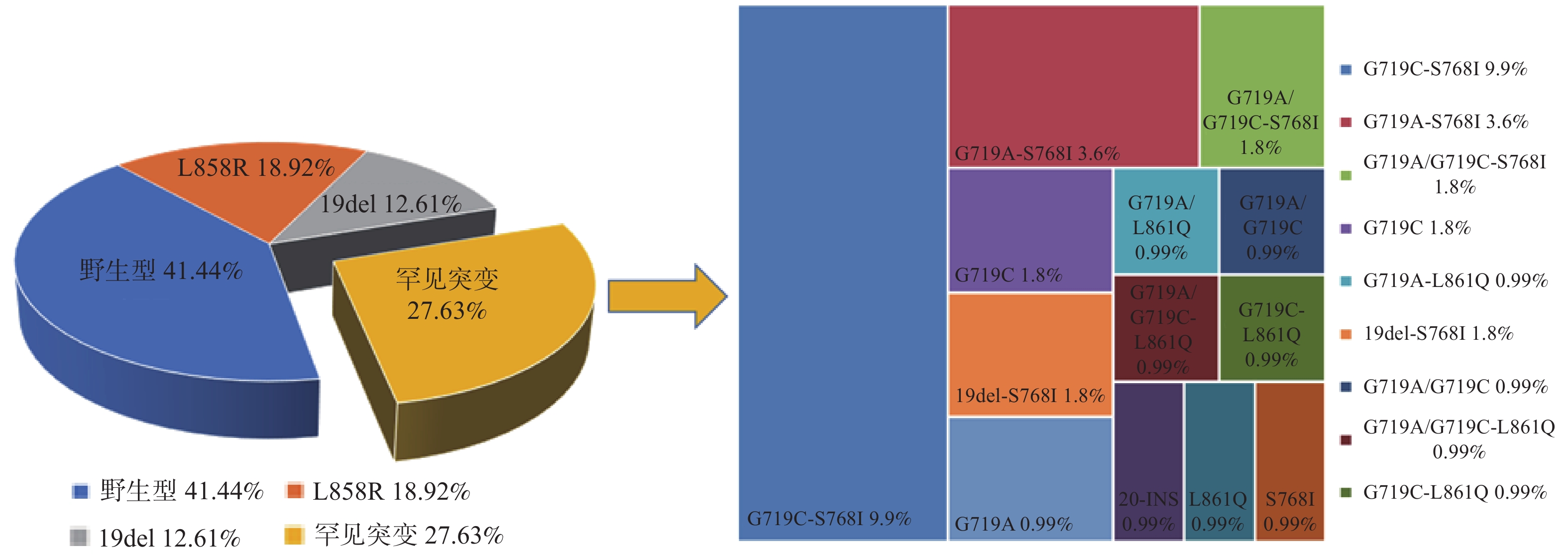
目的 探讨使用下一代测序(Next-generation sequencing,NGS)技术检测云南地区多结节肺腺癌患者肿瘤组织中EGFR基因突变与临床病理特征的关系。 方法 收集2018年1月至2020年5月云南省分子诊断中心共检测的79例多结节肺腺癌患者送检的111枚肺结节肿瘤组织样本,以NGS法检测EGFR突变情况分析其与临床病理特征的关系,Logistic回归分析其独立危险因素。 结果 111枚肺结节组织样本中EGFR总突变率58.55%(65/111),其中L858R点突变和19号外显子缺失最常见,占总突变的53.8%(35/65)。稀有突变率27.02%(30/111),单点突变率37.84%(42/111),复合突变率20.72%(23/111)。χ2检验显示女性、年龄≥56岁、无吸烟史、云南区域性高发肺癌地区患者EGFR基因突变率较高,差异具有统计学意义(P = 0.024、P = 0.008、P < 0.001、P = 0.024)。Logistic回归分析显示:年龄≥56岁、无吸烟史、云南区域性高发肺癌地区是EGFR基因突变的独立危险因素(P < 0.05)。同一患者配对结节样本的EGFR突变状态异质率高达87.5% (28/32)。 结论 云南地区多结节肺腺癌患者中,老年、无吸烟史、来自云南区域性高发肺癌地区是多发肺结节EGFR基因突变的独立危险因素。多结节肺腺癌患者病灶间驱动突变的高水平异质性提示多发结节倾向多原发肿瘤起源,这将为多结节肺腺癌的诊疗策略提供更多的选择。 Abstract:Objective To investigate the relationship between EGFR gene mutations and clinicopathological characteristics of patients with multinodular lung adenocarcinoma in Yunnan province by using NGS method. Methods A total of 111 pulmonary nodule samples from 79 patients with multifocal lung adenocarcinoma were collected between January 2018 to May 2020 in the Molecular Diagnostic Center of Yunnan Cancer Hospital. The NGS method was used to detect the EGFR mutation of multiple lung nodules to analyze its relationship with clinicopathological characteristics, and Logistic regression to analyze its independent risk factors. Results The total EGFR mutation rate in 111 lung nodule tissue samples was 58.55% (65/111), among which L858R point mutation and exon 19 deletion were the most common, accounting for 53.8%of the total mutations (35/65).The rare mutation rate was 27.02% (30/111), the single point mutation rate was 37.84% (42/111), and the compound mutation rate was 20.72% (23/111). χ2 test showed that females, age ≥56 years, non-smoker, areas with a high incidence of lung cancer in Yunnan, earlier pathological stages (stages Ⅰ to Ⅱ), and invasive adenocarcinoma had a higher EGFR gene mutation rate, and the difference was statistically significant (P = 0.036、P = 0.001、P < 0.001、P = 0.006、P = 0.006、P = 0.034).Multivariate Logistic regression analysis showed thatage ≥56 years, non-smoker, areas with a high incidence of lung cancer in Yunnan, and earlier pathological stages (stages Ⅰ to Ⅱ) are independent risk factors for EGFR gene mutations (P<0.05).The heterogeneity rate of EGFR gene expression between paired nodules in the same patient was as high as 87.5% (28/32). Conclusions Among patients with multinodular lung adenocarcinoma in Yunnan, the elderly, non-smoker, areas with a high incidence of lung cancer in Yunnan, and earlier pathological stages (stages Ⅰ to Ⅱ) are independent risk factors for EGFR gene mutations.The high-level heterogeneity of driver mutations among the lesions of patients with multinodular lung adenocarcinoma suggests that multiple nodules tend to be independent of the origin of the primary tumor, which will provide more options for the diagnosis and treatment of multinodular lung adenocarcinoma. -
表 1 多结节肺腺癌患者组织样本中 EGFR突变与临床病理特征关系分析
Table 1. Analysis of the relationship between EGFR mutations and clinicopathological characteristics in tissue samples from patients with multinodular lung adenocarcinoma
病理特征 总数(n = 79) EGFR 突变 χ2 P 突变数(n) 突变率(%) 性别 5.097 0.024 男 26 14 53.84 女 53 39 73.58 年龄(岁) 6.980 0.008 < 56 35 18 51.42 ≥56 44 35 79.54 吸烟状态 无吸烟 57 45 78.94 13.037 < 0.001 吸烟 22 8 36.36 地区 5.126 0.024 高发 53 40 75.47 非高发 26 13 50.00 病理分期 1.853 0.176 Ⅰ~Ⅱ 42 31 73.80 Ⅲ~Ⅳ 37 22 59.45 位置 0.244 0.176 右肺 58 38 65.51 左肺 21 15 71.42 浸润程度 1.871 0.171 浸润前AAH+AIS 12 6 50.00 浸润性 67 47 70.14 密度 1.806 0.405 pGGNs 33 22 66.67 mGGNs 28 28 64.28 Solid 18 13 72.22 表 2 多结节肺腺癌患者EGFR基因突变的多因素分析
Table 2. Multivariate analysis of clinicopathological characteristics of multi-nodular lung adenocarcinoma patient
病理特征 Exp(β) OR (95%CI) P Low Upper 年龄(岁) 3.673 1.368 9.864 0.010 云南区域性高发肺癌地区 3.007 1.142 8.291 0.026 吸烟状态 0.152 0.052 0.447 0.001 性别 0.419 0.157 1.120 0.083 表 3 32例多结节肺腺癌患者配对结节的EGFR突变状态
Table 3. EGFR mutation status of paired nodules in 32 patients with multinodular lung adenocarcinoma
病人编号 结节1 结节 2 病人编号 结节1 结节 2 1 L858R WT 17 L858R WT 2 20-INS L858R 18 G719C-S768I WT 3 L861Q 19del 19 WT WT 4 G719C-S768I WT 20 G719A/G719C L858R 5 G719A-S768I G719A 21 L858R WT 6 L858R 19del 22 G719C-S768I WT 7 G719C G719C-S768I 23 WT G719A/G719C -S768I 8 G719C-S768I WT 24 19del-S768I 19del-S768I 9 G719C-L861Q 19del 25 L858R L858R 10 G719A-L861I L858R 26 L858R L858R 11 WT G719C-S768I 27 G719C-S768I 19del 12 WT G719C 28 WT G719A 13 19del WT 29 19del WT 14 G719A/C-L861Q WT 30 WT WT 15 WT WT 31 L858R WT 16 WT WT 32 L858R L858R -
[1] Bray F,Ferlay J,Soerjomataram I,et al. Global cancer statistics 2018:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin,2018,68(6):394-424. doi: 10.3322/caac.21492 [2] Zhang Y,Jheon S,Li H,et al. Results of low-dose computed tomography as a regular health examination among Chinese hospital employees[J]. J Thorac Cardiovasc Surg,2019,160(3):110-116. [3] Park E,Ahn S,Kim H,et al. Targeted Sequencing Analysis of Pulmonary Adenocarcinoma with Multiple Synchronous Ground-Glass/Lepid ic Nodules[J]. J Thorac Oncol,2018,13(11):1776-1783. doi: 10.1016/j.jtho.2018.07.097 [4] Chen K N. The diagnosis and treatment of lung cancer presented as ground-glass nodule[J]. Gen Thorac Cardiovasc Surg,2020,68(7):697-702. doi: 10.1007/s11748-019-01267-4 [5] Detterbeck F C,Nicholson A G,Franklin W A,et al. The IASLC Lung Cancer Staging Project:Summary of Proposals for Revisions of the Classification of Lu ng Cancers with Multiple Pulmonary Sites of Involvement in the Forthcoming Eighth Edition of the TNM Classification[J]. J Thorac Oncol,2016,11(5):639-650. doi: 10.1016/j.jtho.2016.01.024 [6] John A,Yang B,Shah R. Clinical Impact of Adherence to NCCN Guidelines for Biomarker Testing and First-Line Treatment in Adv anced Non-Small Cell Lung Cancer (aNSCLC) Using Real-World Electronic Health Record Data[J]. Adv Ther,2021,38(3):1552-1566. doi: 10.1007/s12325-020-01617-2 [7] Liu Y,Zhang J,Li L,et al. Genomic heterogeneity of multiple synchronous lung cancer[J]. Nat Commun,2016,7:13200. doi: 10.1038/ncomms13200 [8] Travis W D,Brambilla E,Nicholson A G,et al. The 2015 World Health Organization Classification of Lung Tumors:Impact of Genetic,Clinical and Rad iologic Advances Since the 2004 Classification[J]. J Thorac Oncol,2015,10(9):1243-1260. doi: 10.1097/JTO.0000000000000630 [9] Hattori A,Matsunaga T,Takamochi K,et al. Surgical Management of Multifocal Ground-Glass Opacities of the Lung:Correlation of Clinicopathologi c and Radiologic Findings[J]. Thorac Cardiovasc Surg,2017,65(2):142-149. [10] 中华医学会呼吸病学分会肺癌学组,中国肺癌防治联盟专家组. 肺结节诊治中国专家共识(2018年版)[J]. 中华结核和呼吸杂志,2018,10(41):110-116. [11] Naderi S,Ghorra C,Haddad F,et al. EGFR mutation status in Middle Eastern patients with non-squamous non-small cell lung carcinoma:A si ngle institution experience[J]. Cancer Epidemiol,2015,39(6):1099-1102. doi: 10.1016/j.canep.2015.08.016 [12] Passaro A,Prelaj A,Bonanno L,et al. Activity of EGFR TKIs in Caucasian Patients With NSCLC Harboring Potentially Sensitive Uncommon EGFR Mutations[J]. Clin Lung Cancer,2019,20(2):186-194. doi: 10.1016/j.cllc.2018.11.005 [13] Fan J,Dai X,Wang Z,et al. Concomitant EGFR Mutation and EML4-ALK Rearrangement in Lung Adenocarcinoma Is More Frequent in Multi focal Lesions[J]. Clin Lung Cancer,2019,20(4):517-530. doi: 10.1016/j.cllc.2019.04.008 [14] Chen K,Chen W,Cai J,et al. Favorable prognosis and high discrepancy of genetic features in surgical patients with multiple prima ry lung cancers[J]. J Thorac Cardiovasc Surg,2018,155(1):371-391. doi: 10.1016/j.jtcvs.2017.08.141 [15] Zhou Y,Yang Y,Yang C,et al. Epidermal growth factor receptor (EGFR) mutations in non-small cell lung cancer (NSCLC) of Yunnan in southwestern China[J]. Oncotarget,2017,8(9):15023-15033. doi: 10.18632/oncotarget.14706 [16] Hsu C H,Tseng C H,Chiang C J,et al. Characteristics of young lung cancer:Analysis of Taiwan's nationwide lung cancer registry focusing o n epidermal growth factor receptor mutation and smoking status[J]. Oncotarget,2016,7(29):46628-46635. doi: 10.18632/oncotarget.9338 [17] 王玉婕,冯昊,马山蕊,等. 同时性多原发肺腺癌表皮生长因子受体基因突变相关因素分析[J]. 中华医学杂志,2019,99(29):2297-301. doi: 10.3760/cma.j.issn.0376-2491.2019.29.010 [18] Bao S M,Hu Q H,Yang W T,et al. Targeting Epidermal Growth Factor Receptor in Non-Small-Cell-Lung Cancer:Current State and Future Pe rspective[J]. Anticancer Agents Med Chem,2019,19(8):984-991. doi: 10.2174/1871520619666190313161009 [19] Liu M,He W X,Song N,et al. Discrepancy of epidermal growth factor receptor mutation in lung adenocarcinoma presenting as multipl e ground-glass opacities[J]. Eur J Cardiothorac Surg,2016,50(5):909-913. doi: 10.1093/ejcts/ezw113 [20] Chen G,Sun X,Ren H,et al. The mortality patterns of lung cancer between 1990 and 2013 in Xuanwei,China[J]. Lung Cancer,2015,90(2):155-160. doi: 10.1016/j.lungcan.2015.08.006 [21] 周永春,林艳苹,李权,等. 云南省肺癌患者表皮生长因子受体基因突变的临床特征分析[J]. 中华肿瘤杂志,2020,42(9):6. [22] Takahashi Y,Shien K,Tomida S,et al. Comparative mutational evaluation of multiple lung cancers by multiplex oncogene mutation analysis[J]. Cancer Sci,2018,109(11):3634-3642. doi: 10.1111/cas.13797 [23] Saab J,Zia H,Mathew S,et al. Utility of Genomic Analysis in Differentiating Synchronous and Metachronous Lung Adenocarcinomas from Primary Adenocarcinomas with Intrapulmonary Metastasis[J]. Transl Oncol,2017,10(3):442-449. doi: 10.1016/j.tranon.2017.02.009 [24] Wu C,Zhao C,Yang Y,et al. High Discrepancy of Driver Mutations in Patients with NSCLC and Synchronous Multiple Lung Ground-Glas s Nodules[J]. J Thorac Oncol,2015,10(5):778-783. doi: 10.1097/JTO.0000000000000487 -






 下载:
下载: