Clinical Application of Laparoscopic Cholecystectomy with Fluorescence Cholangiography of Indocyanine Green in the Difficult Cholecystectomy
-
摘要:
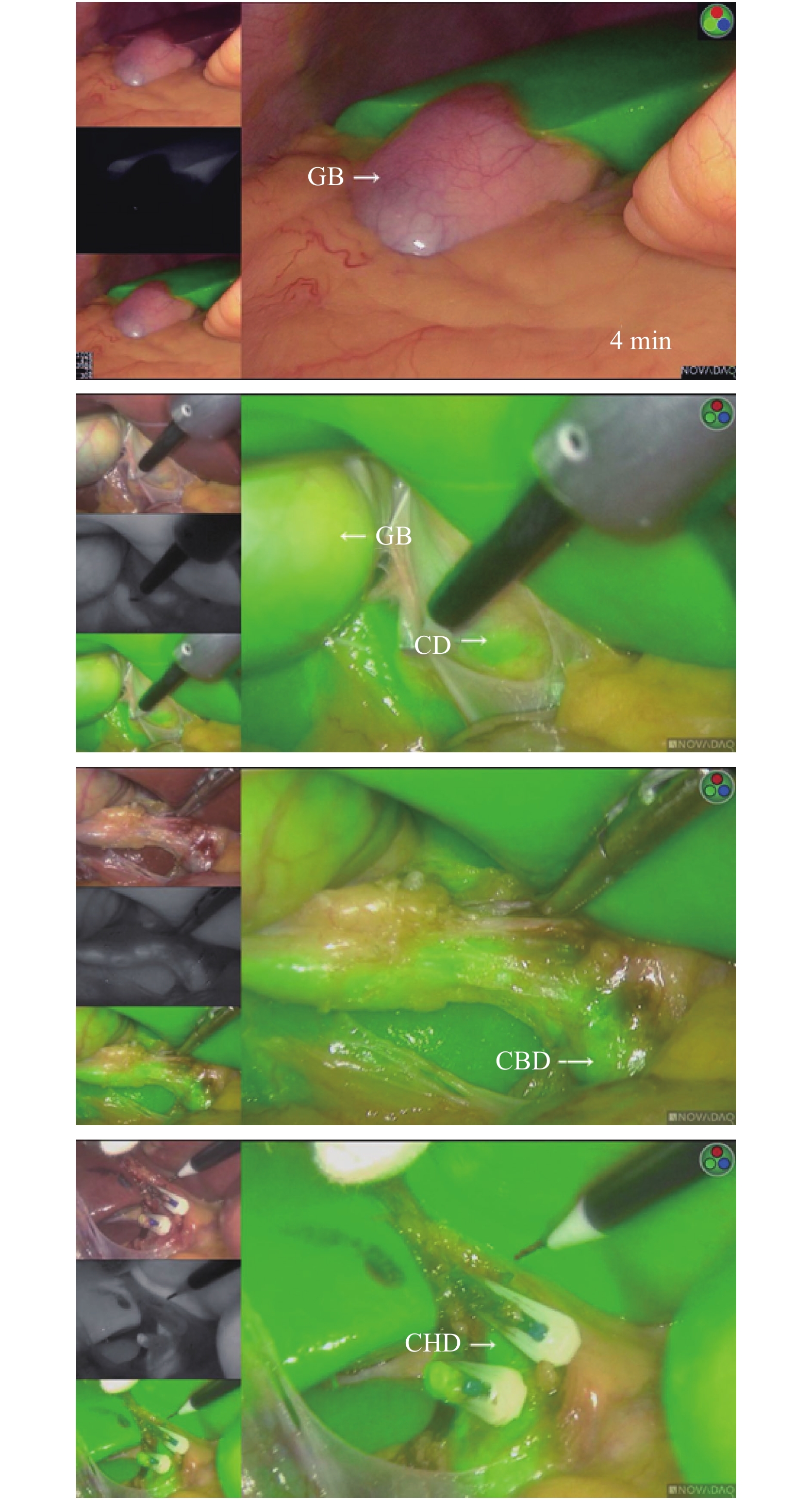
目的 研究吲哚菁绿荧光染色在腹腔镜胆囊切除术中的安全性、可行性及可靠性,能否有效避免胆道损伤,探讨吲哚菁绿荧光腹腔镜技术在困难胆囊切除中的不足与优势。 方法 回顾性分析,收集昆明医科大学第二附属医院自2017年12月1日至2019年12月1日因胆囊结石并反复胆囊炎发作行胆囊切除术65例,男性27例,女性38例,年龄29~67岁,符合困难胆囊切除术入组标准的患者临床资料。65例患者随机分组,其中常规腹腔镜手术组35例(对照组,男性14例,女性21例),吲哚菁绿荧光腹腔镜组30例(实验组,男性13例,女性17例)。分析比较2组患者性别、年龄、基础疾病等一般资料,以及手术时间、术中出血量、术后排气时间、术后住院天数、住院总费用、术前及术后肝功(ALT、AST、血清白蛋白、总胆红素)、肾功(肌酐)、能否有效识别胆管解剖结构以及识别胆道时间。 结果 对照组手术时间较实验组长(P < 0.05);在分离寻找胆囊三角解剖结构的时间上,对照组时间长于实验组时间(P < 0.05);对照组术中出血量与实验组无统计学意义(P > 0.05);对照组术后通气时间、住院总费用、住院时间与实验组无明显差异(P > 0.05);实验组与对照组术后肝功能、血常规、肾功能统计学无明显差异(P > 0.05)。 结论 吲哚菁绿荧光显像腹腔镜在困难胆囊切除术中辨别胆道解剖结构的可操作性高,安全性强,能有效识别胆囊三角的解剖结构,能有效避免胆道及血管损伤;吲哚菁绿荧光显像腹腔镜技术较传统的腹腔镜技术在困难胆囊切除术中存在手术时间短的优势,在术后肝功、感染指标以及住院周期及住院总费用中无明显差异。 Abstract:Objective To study the safety, feasibility and reliability of indocyanine green fluorescence staining in laparoscopic cholecystectomy, whether it can effectively avoid bile duct injury, and to explore the shortcomings and advantages of indocyanine green fluorescence laparoscopic technology in difficult cholecystectomy. Methods The method of retrospective analysis was adopted, and the clinical data of patients meeting inclusion criteria for difficult cholecystectomy in 65 cases of cholecystectomies with the causes of the gallstone and recurrent cholecystitis in The Second Affiliated Hospital of Kunming Medical University from December 1, 2018 to December 1, 2019 were collected. All patients had signed the informed consent and had no history of iodine allergy. 65 patients were assigned randomly with 35 cases of laparoscopic cholecystectomy (LC) and 30 cases of laparoscopic cholecystectomy (LC) with fluorescence cholangiography of indocyanine green (ICG). All kinds of the preoperative, intraoperative and postoperative data were collected to compare between the conventional group and cholangiography group. The application effect, safety and feasibility of the laparoscopic technologies with fluorescence cholangiography in the difficult cholecystectomy were explored, including whether the anatomic structure of the bile duct and the biliary tract time can be identified effectively. Results The time of laparoscopic cholecystectomy (LC) group was significantly longer than that of fluorescence cholangiography group (P < 0.05); in terms of the time to isolate the anatomy of biliary tract, the time of fluorescence cholangiography group was significantly shorter than that of laparoscopic cholecystectomy (LC) group (P < 0.05); the amount of bleeding in laparoscopic cholecystectomy (LC) was no statistically significant combined with fluorescence cholangiography group (P > 0.05); there was no significant difference in length of stay (LOS) and all-in cost of stay between the two groups (P > 0.005). Conclusions Indocyanine green fluorescence imaging laparoscopy has high operability and strong safety in identifying the anatomical structure of biliary tract in difficult cholecystectomy. It can effectively identify the anatomical structure of gallbladder triangle and effectively avoid the injury of biliary tract and blood vessels; Indocyanine green fluorescence imaging laparoscopic technology has the advantage of short operation time compared with traditional laparoscopic technology in Difficult Cholecystectomy, and there is no significant difference in postoperative liver function, infection index, hospitalization cycle and total hospitalization cost. -
Key words:
- Indocyanine green /
- Laparoscopic cholecystectomy /
- Biliary tract injury
-
表 1 2组一般资料比较(
$ \bar x \pm s $ )Table 1. General information comparison of two groups (
$ \bar x \pm s $ )实验组 对照组 t P 体重(kg) 62.28 ± 7.37 63.3 ± 6.5 −1.49 0.143 年龄(岁) 48.2 ± 11.49 50.7 ± 9.47 −0.807 0.424 性别 0.786 ALT(U/L) 36.53 ± 13.99 32.19 ± 14.22 1.069 0.290 AST(U/L) 34.28 ± 16.56 35.07 ± 15.02 −0.171 0.865 GGT(U/L) 33.78 ± 10.68 28.22 ± 11.23 1.766 0.084 TP (g/L) 80.06 ± 16.57 80.11 ± 15.69 −0.010 0.992 TBIL(μmol/L) 12.57 ± 3.17 13.36 ± 2.99 −0.881 0.383 DBIL(μmol/L) 5.66 ± 2.54 6.35 ± 2.18 −0.994 0.325 IBIL(μmol/L) 3.59 ± 2.21 3.42 ± 2.16 0.282 0.779 WBC(109/L) 9.12 ± 2.98 9.73 ± 2.89 −0.721 0.474 Hb(g/L) 123.61 ± 13.7 130.24 ± 13 −1.710 0.094 Cre(μmol/L) 75.67 ± 19.92 78.16 ± 20.47 −1.018 0.314 表 2 术后各指标的组间差异比较(
$ \bar x \pm s $ )Table 2. Comparison of two groups after surgery(
$ \bar x \pm s $ )项目 实验组 对照组 t P ALT(U/L) 40.21 ± 11.54 40.92 ± 12.78 −0.205 0.838 AST(U/L) 34.98 ± 16 37.87 ± 12.8 −0.674 0.504 GGT(U/L) 35.15 ± 9.05 34.58 ± 9.11 0.219 0.827 TP(g/L) 76.28 ± 15.29 76.97 ± 14.32 −0.161 0.873 TBIL(μmol/L) 13.91 ± 3.46 14.73 ± 3.5 −0.813 0.420 DBIL(μmol/L) 7.4 ± 2.62 8.2 ± 2.17 −1.129 0.264 IBIL(μmol/L) 1.01 ± 0.34 0.97 ± 0.31 0.383 0.703 WBC(109/L) 11.58 ± 1.72 11.35 ± 2.08 0.429 0.670 Hb(g/L) 122.86 ± 13.02 129.83 ± 12.94 −1.860 0.069 Cre(μmol/L) 0.64 ± 0.28 0.65 ± 0.24 −0.086 0.932 手术时间(d) 65.91 ± 20.75 90.16 ± 27.34 −3.562 *0.001 术中出血量(mL) 17.1 ± 8.17 22.95 ± 13.96 −1.691 0.102 分离胆囊三角解剖寻找胆道时间(min) 7.59 ± 2.75 11.24 ± 3.75 −3.963 *< 0.001 术后通气时间(h) 14.27 ± 7.9 14.11 ± 8.53d 0.067 0.947 术后住院时间(d) 4.1 ± 1.47 3.58 ± 1.54 1.187 0.241 表 3 术后各指标的组间差异比较
Table 3. Comparison of postoperative complications between the two groups
名称 是否胆漏(%) 总计 精确Sig(双侧) 未胆漏 胆漏 实验组 30(48.39) 0(0.00) 30(46.15) 0.243 对照组 32(51.61) 3(100.00) 35(53.85) 总计 62 3 65 -
[1] Misawa T,Saito R,Shiba H,et al. Analysis of bile duct injuries (Stewart-Way classification)during laparoscopic cholecystectomy[J]. J Hepatobiliary Pancllatsurs,2006,13(5):427-434. [2] 吲哚菁绿标记荧光腹腔镜技术在腹腔镜胃癌根治术中的应用专家共识[J]. 腹腔镜外科杂志, 2019, 24(5): 395-400. DOI: 10.13499/j.cnki.fqjwkzz.2019.05.395. [3] 文峰. 吲哚菁绿血管造影术及其临床应用[J]. 眼科研究,2006(2):113-118. [4] Huang L,Vore M. Multidrug resistance p-glycoprotein 2 is essential for the biliary excretion of indocyanine green[J]. Drug Metab Dispos,2001,29(5):634-637. [5] Ishizawa T,Masuda K,Urano Y,et al. Mechanistic background and clinical applications of indocyanine green fluorescence imaging of hepatocellular carcinoma[J]. Ann Surg Oncol,2014,21(2):440-448. doi: 10.1245/s10434-013-3360-4 [6] 吲哚菁绿荧光染色在腹腔镜肝切除术中应用的专家共识[J]. 腹腔镜外科杂志, 2019, 24(5): 388-394. DOI: 10.13499/j.cnki.fqjwkzz.2019.05.388. [7] 雷光林,李媛媛,胡雄伟,洪智贤. 吲哚菁绿荧光染色技术在肝细胞癌合并肝硬化患者中行腹腔镜解剖性肝切除术的应用[J]. 肝胆胰外科杂志,2019,31(9):517-521. [8] LSF B,Handgraaf HJM,Huurman VAL,et al. The best approach for laparoscopic fluorescence cholangiography:overview of the literature and optimization of dose and dosing time[J]. Surg Innov,2017,24(4):386-396. doi: 10.1177/1553350617702311 [9] Liu YY,Liao CH,Diana M,et al. Near-infrared cholecystocholangiography with direct intragallbladder indocyanine green injection:preliminary clinical results[J]. Surg Endosc,2018,32(3):1506-1514. doi: 10.1007/s00464-017-5838-9 [10] Ankersmit M,Dam DA,Rijswijk AS,et al. Fluorescent imaging with indocyanine green during laparoscopic cholecystectomy in patients at increased risk of bile duct injury[J]. Surg Innov,2017,24(3):245-252. doi: 10.1177/1553350617690309 [11] Ishizawa T,Bandai Y,Kokudo N. Fluorescent cholangiography using indocyanine green for laparoscopic cholecystectomy:an initial experience[J]. Arch Surg,2009,144(4):381-382. doi: 10.1001/archsurg.2009.9 [12] 雷泽华,高峰畏,赵欣,蒋康怡,谢青云,龚杰,乌建平,付金强,杜波,王志旭. 吲哚菁绿荧光显像技术在腹腔镜胆囊切除术中的应用初探[J]. 肝胆胰外科杂志,2019,31(9):522-525. [13] 王坚. 困难腹腔镜胆囊切除应对策略[J]. 中国实用外科杂志,2015,35(9):947-950. [14] Thomson BN, Parks RW, Madhavan KK. et a1. Liver resection and transplantation in the management of [15] iatrogenic biliary injury. World J Surg,2007,31(12):2363-2369 Kern KA. Malpractice litigation involving laparoscopic cholecystec—tomy. Cost,cause,and consequences[J]. Arch Surg,1997,132(4):392-397. doi: 10.1001/archsurg.1997.01430280066009 [16] Aoki T,Yasuda D,Shimizu Y,et al. Image-guided liver mapping using fluorescence navigation system with indocyanine green for anatomical hepatic resection[J]. World J Surg,2008,32(8):1763-1767. doi: 10.1007/s00268-008-9620-y [17] 黄磊. 不同浓度吲哚菁绿在胆囊手术中的应用及其对肝功能的影响[J]. 肝脏,2019,24(7):800-802. doi: 10.14000/j.cnki.issn.1008-1704.2019.07.026 [18] Ishizawa T,Bandai Y,Ijichi M,Kaneko J,Hasegawa K,Kokudo N. Fluorescent cholangiography illuminating the biliary tree during laparoscopic cholecystectomy[J]. Br J Surg,2010,97:1369-1377. doi: 10.1002/bjs.7125 -






 下载:
下载: