Clinical Study of Extracorporeal Shock Wave Combined with Sodium Hyaluronate in the Treatment of Knee Osteoarthritis
-
摘要:
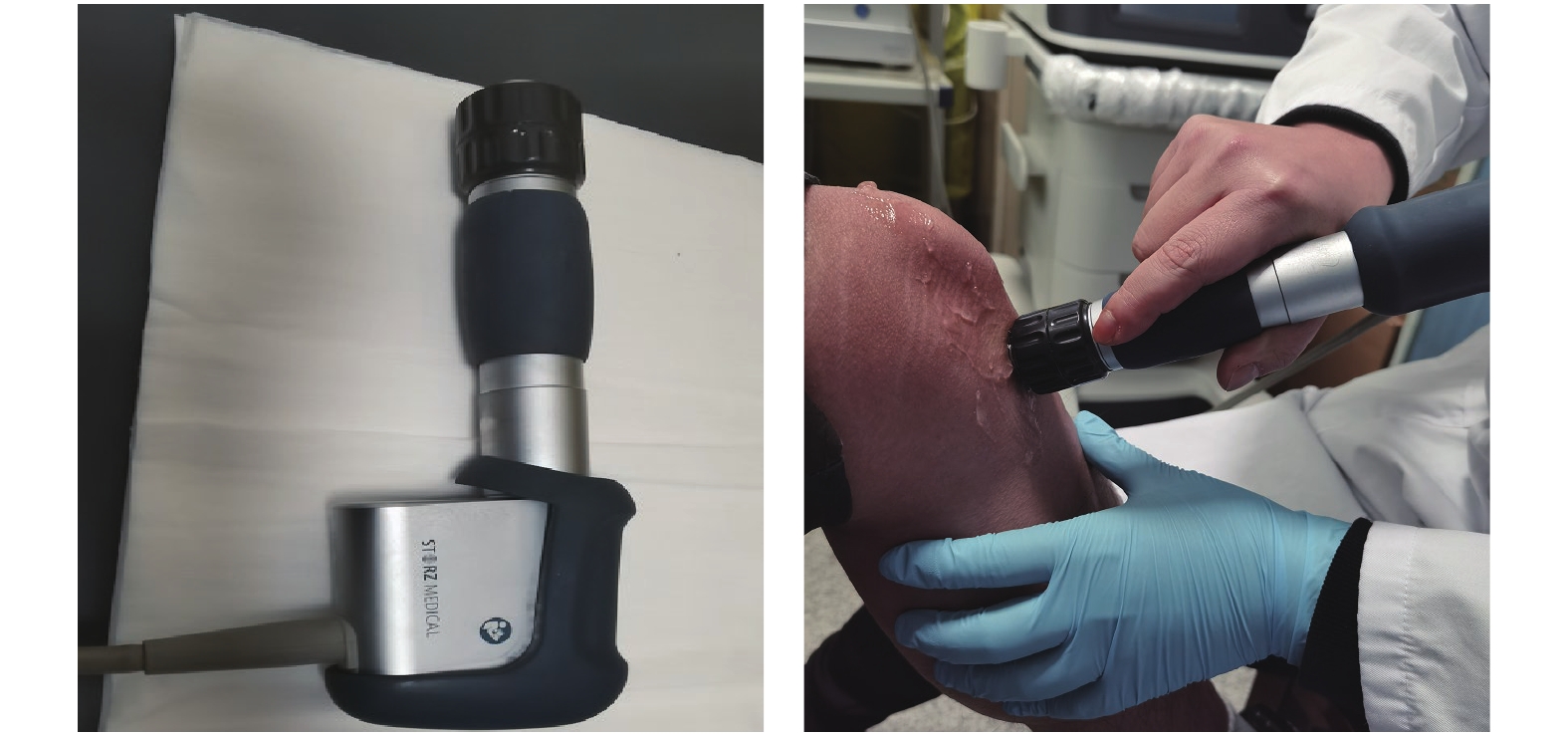
目的 观察体外放射式冲击波联合关节腔注射玻璃酸钠治疗膝关节骨性关节炎(knee osteoarthritis,KOA)的临床疗效。 方法 将62例KOA患者随机分为观察组与对照组,每组各31例,其中观察组男13例,女18例;平均年龄(62.35±9.70)岁,病程(3.06±1.49)a。对照组男16例,女15例;平均年龄(60.87±1.56)岁,病程(2.74±1.53)a。观察组患者先给予体外放射式冲击波治疗(extracorporeal shockwave therapy,ESWT) ,治疗后2d再常规行关节腔内注射玻璃酸钠(intra-articular injections of hyaluronic acid,HA)治疗。对照组患者单纯给予HA治疗。2组患者均每周治疗1次,连续治疗5周。治疗前、治疗结束后1周及治疗结束后3个月分别对2组患者进行疼痛视觉模拟评分(visual analogue scale,VAS)和骨关节炎指数(Western Ontario and McMaster University osteoarthritis index,WOMAC)评分,以评价2组患者的疗效有无差异性;按KOA患者Kellgren-Lawrence分级(Ⅱ、Ⅲ级)将其分为观察组Ⅱ级、对照组Ⅱ级,观察组Ⅲ级、对照组Ⅲ级分别进行治疗前后VAS评分和WOMAC评分比较。 结果 观察组与治疗组2组患者的VAS评分和WOMAC评分在治疗后1周及3月均较治疗前降低(P < 0.05),观察组在治疗后1周及治疗后3月时的VAS评分和WOMAC评分均低于对照组(P < 0.05)。观察组在治疗后3月较治疗后1周时的WOMAC评分进一步降低(P < 0.05),Kellgren-LawrenceⅡ、Ⅲ级患者中观察组和对照组治疗后均较治疗前评分降低(P < 0.05),Ⅱ级组治疗后1周后观察组VAS降低,但差异无统计学意义,WOMAC评分降低(P < 0.05),Ⅱ级组治疗后3月观察组的VAS及WOMAC评分均较对照组降低(P < 0.05),Kellgren-LawrenceⅢ级患者中治疗1周及3月后VAS及WOMAC评分均较对照组降低(P < 0.05)。 结论 ESWT联合HA较单纯行HA治疗KOA疗效更显著,可明显减轻关节疼痛,改善膝关节活动功能。 Abstract:Objective To observe the clinical efficacy of external radiative shock wave combined with sodium hyaluronate injection in the treatment of knee osteoarthritis (KOA). Methods Sixty-two patients with KOA be divided into observation group and control group randomly, with 31 cases in each group. The observation group included 13 males and 18 females, the mean age was (62.35±9.70) years old, and the course of disease was (3.06±1.49) years. There were 16 males and 15 females in the control group, the mean age was (60.87±1.56) years old, and the course of disease was (2.74±1.53) years. The Extracorporeal Shockwave therapy (ESWT) was given firstly , then the Intra-articular injection of hyaluronic acid (HA) was injected 2 days later in the observation group. The control group was treated with HA only 1 week. Both of the groups were treated once a week for 5 weeks. The Visual Analogue Scale (VAS) and Western Ontario and McMaster University Osteoarthritis Index (WOMAC) were used to evaluate the difference in efficacy between the two groups, at the time of before the treatment, 1 week after the treatment and 3 months after that.KOA patients were divided into observation group Ⅱ and control group Ⅱ according to Kellgren-Lawrence grading (Ⅱ, Ⅲ). VAS score and WOMAC score of observation group Ⅲ and control group Ⅲ were compared before and after treatment, respectively. Results The VAS score and WOMAC score in both group were significantly lower than those before at the time of 1 week and 3 months after treatment (P < 0.05), while 1 week after treatment and 3 months after treatment the VAS and WOMAC scores in the observation group were lower than those in the control group (P < 0.05). The WOMAC score of the observation group was further decreased after 3 months than 1 week after treatment (P < 0.05). In kellgren-Lawrence class Ⅱ and Ⅲ patients, the scores of observation group and control group decreased after treatment compared with before treatment (P < 0.05), VAS of observation group decreased 1 week after treatment in class Ⅱ group, but the difference was not statistically significant, WOMAC score decreased (P < 0.05). VAS and WOMAC scores of kellgren-Lawrence grade Ⅲ patients were lower than those of control group 3 months after treatment (P < 0.05), VAS and WOMAC scores of Kellgren-Lawrence grade Ⅲ patients were lower than those of control group 1 week and 3 months after treatment (P < 0.05). Conclusion The ESWT combined with HA can significantly reduce the joint pain and improve knee joint mobility more effectively than HA alone in the treatment of KOA. -
Key words:
- Extracorporeal shock wave /
- Sodium hyaluronate /
- Knee osteoarthritis
-
表 1 2组患者一般情况比较(
$\bar x \pm s $ )Table 1. Comparison of general conditions between the two groups (
$\bar x \pm s $ )基础资料 观察组 对照组 t/χ2 P 年龄(岁) 62.35 ± 9.70 60.87 ± 1.56 0.576 0.567 性别(男/女) 13/18 16/15 0.583 0.611 病程(a) 3.06 ± 1.49 2.74 ± 1.53 0.841 0.404 VAS(分) 5.65 ± 1.08 5.71 ± 0.94 −0.883 0.381 WOMAC(分) 40.39 ± 4.30 40.19 ± 5.80 0.149 0.882 表 2 2组患者治疗前、后 VAS评分的比较[(
$\bar x \pm s $ ),分]Table 2. Comparison of VAS scores between the two groups before and after treatment [(
$\bar x \pm s $ ),scores]组别 治疗前 治疗后1周 治疗后3月 F P 观察组 5.65 ± 1.08 3.97 ± 0.71△ 3.84 ± 0.58△ 48.44 0.001* 对照组 5.71 ± 0.94 4.39 ± 0.56△ 4.29 ± 0.46△ 46.48 0.001* t −0.883 −2.593 −3.382 / / P 0.381 0.012* 0.001* / / *P < 0.05;与治疗前比较,△P < 0.05。 表 3 2组患者治疗前、后WOMAC评分的比较[(
$\bar x \pm s $ ),分]Table 3. Comparison of WOMAC scores between the two groups before and after treatment [(
$\bar x \pm s $ ),scores]组别 治疗前 治疗后1周 治疗后3月 F P 观察组 40.39 ± 4.30 31.61 ± 4.19△ 29.84 + 3.39△# 62.374 0.001* 对照组 40.19 ± 5.80 34.65 + 4.91△ 33.45 + 4.15△ 16.053 0.001* t 0.149 −2.615 −3.753 / / P 0.882 0.011* 0.001* / / *P < 0.05;与治疗前比较,△P < 0.05;与治疗后1周比较,#P < 0.05。 表 4 Kellgren-LawrenceⅡ、Ⅲ级在2组患者治疗前、后VAS及WOMAC评分的比较[(
$\bar x \pm s $ ),分]Table 4. Comparison of VAS and WOMAC scores of Kellgren-Lawrence Ⅱ and Ⅲ in 2 groups before and after treatment [(
$\bar x \pm s $ ),scores]组别 治疗前
(VAS/WOMAC)治疗后1周
(VAS/WOMAC)治疗后3月
(VAS/WOMAC)F P Ⅱ级 观察组 5.17 ± 0.58
37.67 ± 3.454.25 ± 0.75△
30.17 ± 4.32△3.83 ± 0.58△
29.42 ± 3.12△13.564
18.5940.001*
0.001*对照组 5.47 ± 0.74
39.20 ± 6.824.40 ± 0.51△
33.80 ± 4.63△4.33 ± 0.49△
32.93 ± 3.59△17.373
6.4190.001*
0.004*t −1.147
−0.708−0.617
−2.058−2.440
−2.676/ / p 0.262
0.4580.543
0.047*0.022
0.013*/ / Ⅲ级 观察组 5.53 ± 0.84
42.11 ± 3.943.79 ± 0.63△
32.53 ± 3.95△3.84 ± 0.63△
30.11 ± 3.60△#37.900
52.0150.001*
0.001*对照组 5.63 ± 0.62
41.13 ± 4.694.38 ± 0.62△
35.44 ± 5.18△4.25 ± 0.45△
33.94 ± 4.68△28.707
9.7590.001*
0.001*t −0.389
0.672−2.759
−1.886−2.237
−2.735/ / p 0.700
0.5060.009
0.0680.032
0.010*/ / *P < 0.05;与治疗前比较,△P < 0.05;与治疗后1周比较,#P < 0.05。 -
[1] Hussain S M,Neilly D W,Baliga S,et al. Knee osteoarthritis:a review of management options[J]. Scott Med,2016,61(1):7-16. [2] Hutyra C A,Gonzalez J M,Yang J C,et al. Patient preferences forsurgical treatment of knee osteoarthritis:A discrete-choice experiment evaluating total and unicompartmental knee arthroplasty[J]. J Bone Joint Surg Am,2020,102(23):2022-2031. doi: 10.2106/JBJS.20.00132 [3] 王弘德,李升,陈伟,等. 《骨关节炎诊疗指南(2018年版)》膝关节骨关节炎部分的更新与解读[J]. 河北医科大学学报,2019,40(9):993-995+1000. doi: 10.3969/j.issn.1007-3205.2019.09.001 [4] 李溪. 膝关节骨性关节炎危险因素的病例对照研究[D]. 昆明: 昆明医科大学硕士学位论文, 2019. [5] 杨正协. 膝骨性关节炎的临床治疗进展[J]. 临床医药文献电子杂志,2019,6(39):190-191. [6] Wang R,Ma C,Han Y,et al. Effectiveness of denervation therapy on pain and joint function for patients with refractory knee osteoarthritis:A systematic review and meta-analysis[J]. Pain Physician,2019,22(4):341-352. [7] Schroeder Allison N,Tenforde Adam S,Jelsing Elena J. Extracorporeal shockwave therapy in the management of sports medicine injuries[J]. Current Sports Medicine Reports,2021,20(6):298-305. doi: 10.1249/JSR.0000000000000851 [8] 王林伟,刘明廷,曹恒,等. 体外冲击波治疗肌肉骨骼系统疾病的研究进展[J]. 中国矫形外科杂志,2019,27(1):63-66. [9] 中华医学会骨科学分会关节外科学组,中国医师协会骨科医师分会骨关节炎学组,国家老年疾病临床医学研究中心(湘雅医院),等. 中国骨关节炎诊疗指南(2021年版)[J]. 中华骨科杂志,2021,41(18):1291-1314. [10] Kohn M D,Sassoon A A,Fernando N D. Classifications in brief:Kellgren-lawrence classification of osteoarthritis[J]. Clin Orthop Relat Res,2016,474(8):1886-1893. doi: 10.1007/s11999-016-4732-4 [11] Migliorini F,Driessen A,Quack V,et al. Comparison between intra-articular infiltrations of placebo,steroids,hyaluronic and PRP for knee osteoarthritis:a Bayesian network meta-analysis[J]. Arch Orthop Trauma Surg,2021,141(9):1473-1490. doi: 10.1007/s00402-020-03551-y [12] 闫慧玲,赵宏斌,钱传云,等. 膝骨关节炎疗效评估的研究进展[J]. 昆明医科大学学报,2019,40(1):123-127. doi: 10.3969/j.issn.1003-4706.2019.01.027 [13] Kolasinski S L,Neogi T,Hochberg M C,et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand,Hip,and Knee[J]. Arthritis Care & Research,2020,72(2):149-162. [14] Geusens P P,van den Bergh J P. Osteoporosis and osteoarthritis:shared mechanisms and epidemiology[J]. Current Opinion in Rheumatology,2016,28(2):97-103. doi: 10.1097/BOR.0000000000000256 [15] Conaghan P G,Cook A D,Hamilton J A,et al. Therapeutic options for targeting inflammatory osteoarthritis pain[J]. Nature reviews. Rheumatology,2019,15(6):355-363. doi: 10.1038/s41584-019-0221-y [16] 吴江怡,陈昊,杨柳. 骨关节炎的关节腔内注射药物及生物制剂治疗现状[J]. 骨科临床与研究杂志,2019,4(2):113-119. [17] 中国研究型医院学会冲击波医学专业委员会,国际冲击波医学学会中国部. 骨肌疾病体外冲击波疗法中国专家共识(第2版)[J]. 中国医学前沿杂志(电子版),2017,9(2):25-33. [18] 李明真,张元鸣飞,李涛,等. 体外冲击波治疗膝关节骨性关节炎的疗效观察[J]. 中国康复医学杂志,2020,35(12):1444-1449. doi: 10.3969/j.issn.1001-1242.2020.12.007 [19] 王璐璐,董羿,梁爽,等. 放散式冲击波治疗在膝关节骨关节炎中的临床应用[J]. 颈腰痛杂志,2016,37(4):354-355. [20] 中华医学会物理医学与康复学分会,肌肉骨骼疾病体外冲击波治疗专家共识组. 肌肉骨骼疾病体外冲击波治疗专家共识[J]. 中华物理医学与康复杂志,2019,41(7):481-487. doi: 10.3760/cma.j.issn.0254-1424.2019.07.001 [21] 王瑞松,全健,李锐,等. 关节镜下纳米微骨折骨髓刺激增强术联合冲击波治疗膝骨性关节炎软骨损伤临床疗效观察[J]. 陕西医学杂志,2021,50(9):1119-1122. doi: 10.3969/j.issn.1000-7377.2021.09.019 [22] 王彦鹏,孙明林,张伟. 体外冲击波对膝骨关节炎IL-32、DKK-1水平的影响[J]. 实用骨科杂志,2017,23(9):807-810. [23] Lane N E,Shidara K,Wise B L. Osteoarthritis year in review 2016:clinical[J]. Osteoarthritis Cartilage,2017,25(2):209-215. [24] JI Q,WANG P,HE C. Extracorporeal shockwave therapy as a novel and potential treatment for degenerative cartilage and bone disease:Osteoarthritis. A qualitative analysis of the literature[J]. Prog Biophys Mol Biol,2016,121(3):255-265. doi: 10.1016/j.pbiomolbio.2016.07.001 -






 下载:
下载: