Effect of MDT Model in the Treatment of Anterior Displacement of Irreducible Disc of Temporomandibular Joint
-
摘要:
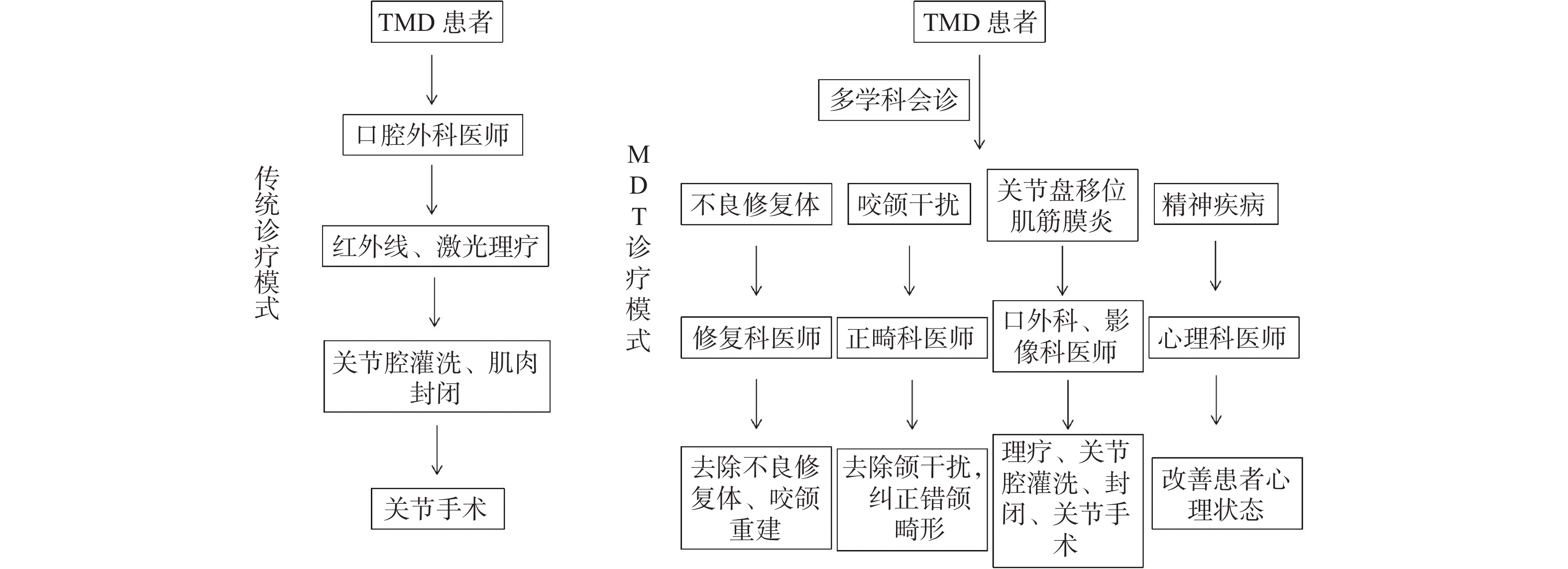
目的 探讨多学科诊疗团队(multidisciplinary team,MDT)诊疗模式在颞下颌关节盘不可复性盘前移位的治疗效果。 方法 选取云南大学附属医院2018年9月至2021年3月收治的60例颞下颌关节不可复性盘前移位患者,随机分为MDT组和非MDT组。MDT组给予MDT诊疗模式;非MDT组给予常规诊疗模式。比较2组患者临床相关指标、治疗前后心理状况、近期临床疗效及患者满意率。 结果 MDT组治疗前等待时间及平均住院时间均低于非MDT组(P < 0.05);MDT组近期疗效总有效率为96.67%,高于非MDT组的90.00%(P < 0.05);MDT组患者满意率为96.66%,高于非MDT组的86.67%(P < 0.05)。 结论 颞下颌关节紊乱病MDT团队诊疗模式,能为颞下颌关节不可复性盘前移位患者提供与病情相适应的最佳治疗,更好的保障患者围手术期安全。同时可以缩短医疗周期,提高疗效。 Abstract:Objective To explore the effect of multidisciplinary team (MDT) in the treatment of irreducible anterior displacement of temporomandibular joint disc. Methods 60 patients with irreducible anterior disc displacement of tempor omandibular joint treated in The Affiliated Hospital of Yunnan University from September 2018 to March 2021 were randomly divided into MDT group and non-MDT group. MDT group received MDT diagnosis and treatment model; The non-MDT group received routine treatment. Clinical indicators, psychological status before and after treatment, shart-term clinical efficacy and satisfaction rate of patients in 2 groups were compared. Results The waiting time and average hospital stay in MDT group were lower than those in non-MDT group (P < 0.05).The total effective rate of MDT was 96.67%, which was higher than 90.00% in non-MDT group. The satisfaction rate of patients in MDT group was 96.66%, which was higher than 86.67% in non-MDT group (P < 0.05). Conclusion The MDT team diagnosis and treatment model for temporomandibular joint disorders can provide the best treatment appropriate to the condition of patients with irreversible anterior displacement of TMJ, and better guarantee the perioperative safety of patients. At the same time, it can shorten the medical cycle and improve the curative effect. -
表 1 患者基本信息及病情的Wilkes分期统计[n(%)]
Table 1. Statistics of basic information and Wilkes staging of patients’condition[n(%)]
项目 性别 Wilkes分期 平均年龄
[($ \bar x \pm s $)岁]男 女 Wilkes III Wilkes IV Wilkes V MDT组(n = 30) 13(43.33) 17(56.67) 18(60.00) 10(33.33) 2(6.67) (25.85 ± 7.41) 非MDT组(n = 30) 12(40.00) 18(60.00) 19(63.33) 9(30.00) 2(6.67) (28.25 ± 7.95) P 0.834 0.246 0.584 表 2 2组患者时间成本比较(
$ \bar x \pm s $ )Table 2. Comparison of time cost between the two groups
分组 治疗前等待时间(d) 平均住院时间(d) MDT组(n = 30) 2.65 ± 0.79 5.25 ± 1.00 非MDT组(n = 30) 4.35 ± 1.02 9.85 ± 1.18 t 3.046 2.486 P 0.005* 0.035* *P < 0.05。 表 3 2组患者近期临床疗效比较[n(%)]
Table 3. Comparison of short-term clinical efficacy between the two groups[n(%)]
分组 完全缓解 部分缓解 无变化 有效率(%) MDT组
(n=30)20(66.67 ) 9(30.00 ) 1(3.33 ) 96.67 非MDT组
(n = 30)15(50.00 ) 11(36.67 ) 4(13.33 ) 86.67 P 0.042* *P < 0.05。 表 4 2组患者满意度比较[n(%)]
Table 4. Comparison of patient satisfaction between the two groups[n(%)]
分组 非常满意 基本满意 不满意 有效率(%) MDT组
(n = 30)16(53.33 ) 13(43.33 ) 1(3.33 ) 96.66 非MDT组
(n = 30)10(33.33 ) 15(50.00 ) 4(13.33 ) 83.33 P 0.008* *P < 0.05。 -
[1] 李琼,石慧清,郭立娜. 颞下颌关节紊乱病的治疗进展[J]. 内蒙古医科大学学报,2019,41(2):207-210. [2] 张志愿. 口腔颌面外科学[M]. 北京: 人民卫生出版社, 2013: 376 [3] Manfredini D,Guarda-nardini L,Winocur E,et al. Research diagnostic criteriafor temporomandibular disorders:A systematic review of axis I epidemiologic findings[J]. Oral Surgery,Oral Medicine,Oral Pathology,Oral Radiology & Endodontics,2011,112(4):453-462. [4] Ingawalé S,Goswami T. Temporomandibular joint:Disor- ders,treatments and biomechanics[J]. Ann Biomed Eng,2009,37(5):976-996. doi: 10.1007/s10439-009-9659-4 [5] Lamb B W,Sevdalis N,Benn J,et al. Multidisciplinary cancer team meeting structure and treatment decisions:A prospective correlational study[J]. Ann Surg Oncol,2013,20(3):715-722. doi: 10.1245/s10434-012-2691-x [6] 张东升,郑家伟,张陈平,等. 口腔癌合并全身系统性疾病患者的多学科协作诊疗模式专家共识[J]. 华西口腔医学杂志,2020,38(6):603-615. doi: 10.7518/hxkq.2020.06.001 [7] 张颖,卢锦芬,张清彬. 改良后牙咬合板治疗颞下颌关节盘不可复性前移位的效果评价[J]. 上海口腔医学,2021,30(2):210-213. [8] 沈达,柳江太,李健. 改良切口关节盘锚固术治疗颞下颌关节盘不可复性前移位的临床评价[J]. 中国口腔颌面外科志,2018,16(1):69-72. [9] Wilkes C H. Internal derangements of the temporomandibular joint. Pathological variations[J]. Arch Otolaryngol Head Neck Surg,1989,115(4):469-477. doi: 10.1001/archotol.1989.01860280067019 [10] 徐高丽,肖芳,霍光. 颞下颌关节盘前移位后关节的适应性改建[J]. 口腔颌面外科杂志,2016,26(1):61-64. doi: 10.3969/j.issn.1005-4979.2016.01.013 [11] 黄淑琼,顾颖,邱宁宁,等. 稳定型咬合板治疗青少年颞下颌关节可复性盘前移位的疗效分析[J]. 广东医科大学学报,2019,37(4):449-451. [12] 张栩,李松. 应力下髁突软骨中相关因子对髁突生长发育作用的研究进展[J]. 昆明医科大学学报,2017,38(04):142-146. doi: 10.3969/j.issn.1003-4706.2017.04.035 [13] 张晓虎,吴勇. 青少年单侧颞下颌关节盘移位患者颌骨三维变化的测量分析[J]. 口腔医学,2017,37(12):1070-1074. [14] 谢千阳,杨驰,马志贵. 青少年关节盘移位与下颌偏斜相关性研究进展[J]. 口腔颌面外科杂志,2012,22(2):140-143. doi: 10.3969/j.issn.1005-4979.2012.02.019 [15] 张陈平. 口腔癌的多学科协作诊疗模式[J]. 中国肿瘤临床,2015,42(16):787-790. doi: 10.3969/j.issn.1000-8179.2015.16.857 [16] 郑宇,王金华. 江苏省某肿瘤专科医院网络MDT实践探索[J]. 江苏卫生事业管理,2020,31(11):1480-1483. doi: 10.3969/j.issn.1005-7803.2020.11.025 [17] 李蕊,王晓虎,周末,等. 安徽省某三级综合医院多学科综合诊疗模式实施影响因素分析与对策研究[J]. 安徽预防医学杂志,2020,26(2):96-98. [18] 韩悦,翁卫群,黄馨仪,等. 多学科协作诊疗模式的发展现状与实践探索[J]. 基层医学论坛,2020,24(22):3239-3241. [19] 姜中豪,戴朝六. 多学科综合治疗时代肝癌外科新理念[J]. 中华普通外科学文献(电子版),2020,14(6):401-405. doi: 10.3877/cma.j.issn.1674-0793.2020.06.001 [20] Loizzo M,Gallo F,Caruso D. Reducing complications and overall healthcare costs of hip fracture management:A retrospective study on the application of a diagnostic therapeutic pathway in the cosenza general hospital[J]. Indian J Orthopaed,2018,52(2):161-169. [21] 刘闪闪,梁爱群,舒惠萍. 肝癌手术患者中开展积极健康教育对提升耐受性、遵医行为的作用研究[J]. 包头医学院学报,2020,36(7):65-68. [22] Patel A,Franko E R,Fleshman J W. Utilizing the multidisciplinary team for planning and monitoring care and quality improvement[J]. Clin Colon Rectal Surg,2015,28(1):12-20. doi: 10.1055/s-0035-1545065 -






 下载:
下载: