Exploring the Efficacy of Different Mathematical Models with Multi-b Value DWI in Predicting Lymphatic Vascular Invasion of Endometrial Cancer
-
摘要:
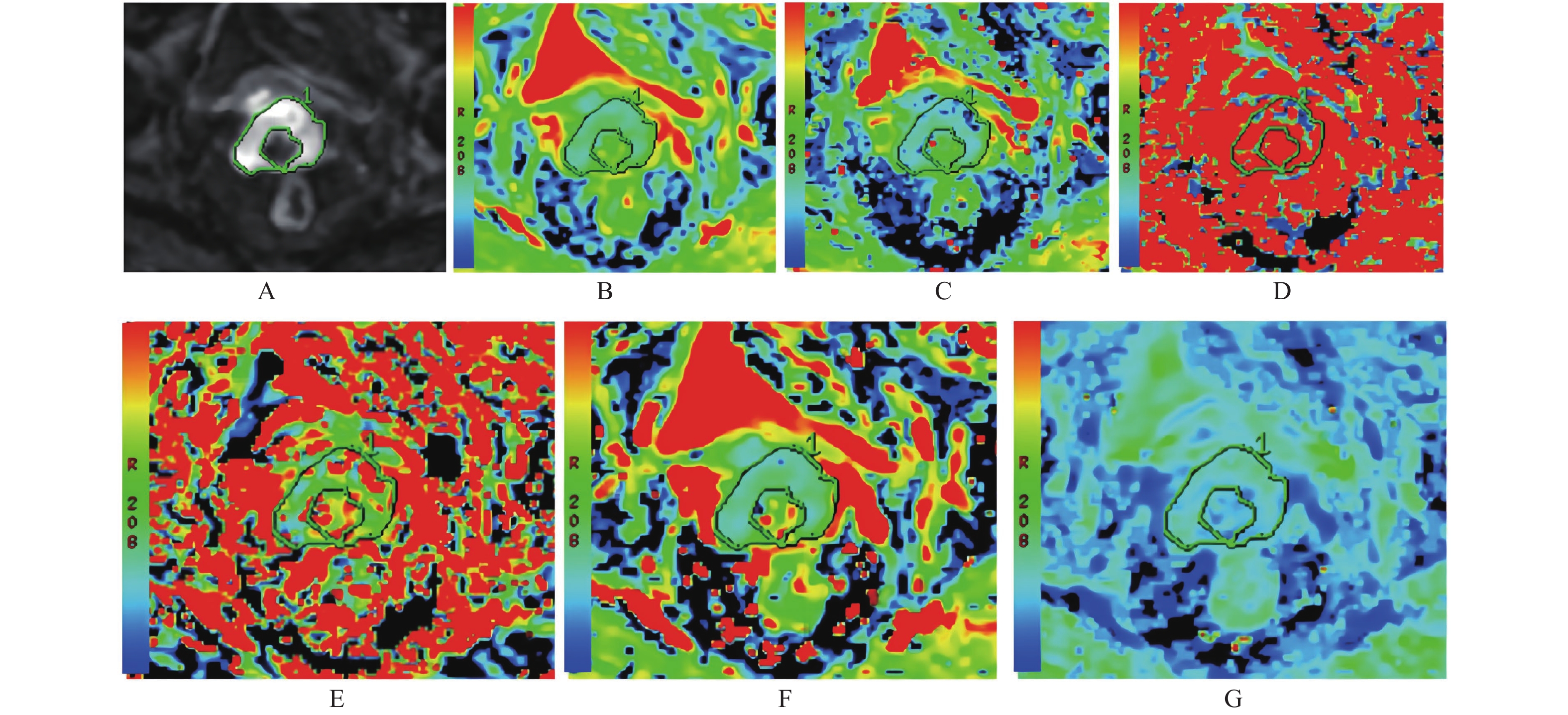
目的 评估不同数学模型多b值扩散加权成像(diffusion-weighted imaging,DWI)在预测子宫内膜癌(endometrial cancer,EC)淋巴血管侵犯(lymphovascular space invasion,LVSI)中的能力。 方法 收集2019年9月至2021年5月期间接受多b值DWI盆腔磁共振成像(magnetic resonance imaging,MRI)检查的患者61例。测量并比较表观扩散系数(apparent-diffusion-coefficient,ADC)、双指数模型参数(D、D*和f)和拉伸指数模型参数(DDC和α),分析经病理证实的预后相关危险因素:组织学分级和淋巴血管侵犯(lymphovascular space invasion,LVSI)。进行受试者工作特征曲线评估不同模型参数在预测EC肿瘤分级和LVSI中的诊断性能。通过多元Logistic回归模型确定EC肿瘤分级和LVSI相关DWI模型参数。使用组内相关系数(ICC)评估观察者间一致性。 结果 高级别组的ADC、D、f和DDC显著低于低级别组(AUC:0.699~0.882,P < 0.05)。与没有LVSI的肿瘤相比,有LVSI肿瘤的ADC、D*、f和DDC值显著降低(AUC:0.671~0.759,P < 0.05)。联合f和DDC在区分高级别和LVSI肿瘤方面具有最大AUC(0.895、0.797)。多元Logistic回归分析显示,f和DDC均可作为肿瘤分级和LVSI独立相关的预测因子。ICC分析显示,D(ICC = 0.973;95%CI = 0.956~0.985)、D*(ICC = 0.911;95%CI = 0.851~0.946)、ADC(ICC = 0.968;95%CI = 0.947~0.980)、f(ICC = 0.957;95%CI = 0.922~0.974)、DDC(ICC = 0.947;95 %CI = 0.912~0.968)和α值(ICC = 0.931;95%CI = 0.884~0.958)的观察者间一致性非常好。 结论 不同数学模型多b值DWI是一种有用且无创的方法,可用于预测EC预后相关的高组织学分级和LVSI,具有更全面的生物学信息。 Abstract:Objective To evaluate the efficacy of different mathematical models of multi-b-value DWI in predicting lymphatic vascular invasion (LVSI) of endometrial cancer (EC). Methods The study population comprised 61 women who underwent multi-b-value DWI pelvic MRI between September 2019 and May 2021. The apparent-diffusion-coefficient (ADC), bi-exponential model parameters (D, D* and f) and stretched-exponential model parameters (DDC and α) were measured and compared to analyze the following prognosis-related risk factors confirmed by pathology: histological grade and LVSI. The receiver operating characteristic (ROC) curve was performed to evaluate the diagnostic performance of these parameters in predicting EC histological grade and LVSI. The EC histological grade and LVSI related DWI model parameters were determined by multiple logistic regression model. The intra-group correlation coefficient (ICC) was used to assess the inter-observer agreement. Results The ADC, D, f, and DDC of the high histological grade group were significantly lower than those of the low histological grade group (P < 0.05, AUC: 0.699-0.882). Compared with tumors without LVSI, tumors with LVSI had significantly lower ADC, D*, f and DDC values ( P < 0.05, AUC: 0.671-0.759). The combination of f and DDC showed higher AUC (0.895, 0.797) than a single parameter in distinguishing high histological grade and LVSI tumors. Multivariate logistic regression analysis showed that both f and DDC can be used as independent predictors of histological grade and LVSI. ICC analysis showed that the inter-observer agreement for the D (ICC = 0.973; 95%CI = 0.956-0.985), D* (ICC = 0.911; 95%CI = 0.851-0.946), ADC (ICC = 0.968; 95%CI = 0.947-0.980), f (ICC = 0.957; 95%CI = 0.922-0.974), DDC (ICC = 0.947; 95%CI = 0.912−0.968) and α value (ICC = 0.931; 95%CI = 0.884-0.958) were very good. Conclusions Multi-b value DWI with different mathematical models is a useful and noninvasive approach for prediction of prognosis-related risk factors in EC with more comprehensive biological information. -
表 1 EC预后相关的高组织学分级和LVSI的不同DWI模型参数差异
Table 1. High histological grades related to EC prognosis and differences in parameters of different DWI models of LVSI
指标 ADC(×10−3 mm2/s) D(×10−3 mm2/s) D*(×10−3 mm2/s) f DDC(×10−3 mm2/s) α 肿瘤分级 低级 1.05 ± 0.12 0.66 ± 0.09 7.76(4.00~87.85) 0.26 ± 0.07 0.93 ± 0.16 0.73 ± 0.04 高级 0.87 ± 0.12 0.55 ± 0.06 7.10(4.64~29.20) 0.22 ± 0.06 0.69 ± 0.15 0.71 ± 0.07 t/U 6.472 5.417 1.062 2.523 9.471 1.245 P < 0.001* < 0.001* 0.635 0.041* < 0.001* 0.219 LVSI 阴性 1.03 ± 0.14 0.64 ± 0.01 7.32(4.00~87.85) 0.26 ± 0.07 0.91 ± 0.18 0.73 ± 0.05 阳性 0.93 ± 0.13 0.59 ± 0.08 10.2(4.96~56.95) 0.21 ± 0.08 0.75 ± 0.16 0.71 ± 0.05 t/U 4.233 1.938 2.755 3.981 4.520 1.742 P 0.018* 0.065 0.039* 0.017* 0.002* 0.051 *P < 0.05。 表 2 DWI模型得出的单个和组合参数在预测EC肿瘤分级和LVSI中的诊断性能
Table 2. Diagnostic performance of individual and combined parameters derived from DWI models in predicting EC tumor grade and LVSI
参数 截止值 AUC P 敏感度(%) 特异度(%) 肿瘤分级 ADC ≤ 0.945 0.862 < 0.001* 83.3 83.7 D ≤ 0.619 0.848 < 0.001* 94.4 58.1 f ≤ 0.233 0.699 0.005* 83.3 65.1 DDC ≤ 0.821 0.882 < 0.001* 88.9 79.1 联合f和DDC 0.895 < 0.001* 88.9 79.1 LVSI ADC(×10−3 mm2/s) ≤ 0.922 0.686 0.019* 58.8 81.8 D*(×10−3 mm2/s) > 5.805 0.671 0.017* 94.1 40.9 f ≤ 0.203 0.711 0.007* 58.8 77.3 DDC ≤ 0.931 0.759 < 0.001* 88.2 54.6 联合f和DDC 0.797 < 0.001* 76.5 70.5 *P < 0.05。 表 3 多元Logistic回归模型确定EC肿瘤分级和LVSI相关DWI模型参数
Table 3. Multivariate Logistic regression model to determine EC tumor grade and LVSI related DWI model parameters
参数 OR 95 %CI P 方差膨胀因子a 模型拟合 肿瘤分级 常量 0.904 0.325~1.842 0.129 f 0.001 0~0.720 0.044 1.029 DDC 0.001 0~0.007 < 0.001* 1.029 LVSI 常量 0.823 0.394~1.438 0.321 f 0.001 0~0.336 0.030* 1.029 DDC 0.004 0~0.214 0.006* 1.029 a方差膨胀因子小于5,表明回归模型不存在多重共线性。*P < 0.05。 -
[1] 王成艳. 子宫内膜癌组织学分型和淋巴脉管间隙浸润的多模态MR成像研究进展[J]. 临床放射学杂志,2020,39(9):1885-1889. [2] 蓝喜,何文雯,郑成军,等. Ⅱ型子宫内膜癌预后因素的COX回归分析[J]. 昆明医科大学学报,2020,41(7):160-164. doi: 10.3969/j.issn.1003-4706.2020.07.032 [3] Daix M,Angeles M A,Migliorelli F,et al. Concordance between preoperative ESMO-ESGO-ESTRO risk classification and final histology in early-stage endometrial cancer[J]. J Gynecol Oncol,2021,32(4):48. doi: 10.3802/jgo.2021.32.e48 [4] 郝建成,孙丽娟,郝金钢. 乳腺结节状病变的MRI诊断[J]. 昆明医科大学学报,2021,42(10):127-131. doi: 10.12259/j.issn.2095-610X.S20211007 [5] Lin M,Yu X,Chen Y,et al. Contribution of mono-exponential,bi-exponential and stretched exponential model-based diffusion-weighted MR imaging in the diagnosis and differentiation of uterine cervical carcinoma[J]. Eur Radiol,2017,27(6):2400-2410. doi: 10.1007/s00330-016-4596-8 [6] Wang Y,Hu D,Yu H,et al. Comparison of the diagnostic value of monoexponential,biexponential,and stretched exponential diffusion-weighted MRI in differentiating tumor stage and histological grade of bladder cancer[J]. Acad Radiol,2019,26(2):239-246. doi: 10.1016/j.acra.2018.04.016 [7] Lin L,Xue Y,Duan Q,et al. Grading meningiomas using mono-exponential,bi-exponential and stretched exponential model-based diffusion-weighted MR imaging[J]. Clin Radiol,2019,74(8):15-23. [8] 张箭,薛旭涛,刘燕,等. 肿瘤全域ADC直方图在鉴别子宫内膜癌组织级别中的应用[J]. 临床放射学杂志,2019,38(4):678-683. [9] 范婵媛,闵祥德,方俊华,等. 基于ADC图的纹理分析在低,高级别前列腺癌诊断中的价值[J]. 中华放射学杂志,2019,53(10):859-863. doi: 10.3760/cma.j.issn.1005-1201.2019.10.013 [10] Yue W,Meng N,Wang J,et al. Comparative analysis of the value of diffusion kurtosis imaging and diffusion-weighted imaging in evaluating the histological features of endometrial cancer[J]. Cancer Imaging,2019,19(1):9. doi: 10.1186/s40644-019-0196-6 [11] Thieme S F,Collettini F,Sehouli J,et al. Preoperative evaluation of myometrial invasion in endometrial carcinoma:Prospective intra-individual comparison of magnetic resonance volumetry,diffusion-weighted and dynamic contrast-enhanced magnetic resonance imaging[J]. Anticancer Res,2018,38(8):4813-4817. doi: 10.21873/anticanres.12791 [12] Lavaud P,Fedida B,Canlorbe G,et al. Preoperative MR imaging for ESMO-ESGO-ESTRO classification of endometrial cancer[J]. Diagn Interv Imaging,2018,99(6):387-396. doi: 10.1016/j.diii.2018.01.010 [13] Wang F,Wang Y,Zhou Y,et al. Comparison between types I and II epithelial ovarian cancer using histogram analysis of monoexponential,biexponential,and stretched-exponential diffusion models[J]. J Magn Reson Imaging,2017,46(6):1797-1809. doi: 10.1002/jmri.25722 [14] Yabuuchi H,Kamitani T,Sagiyama K,et al. Characterization of parotid gland tumors:Added value of permeability MR imaging to DWI and DCE-MRI[J]. Eur Radiol,2020,30(12):6402-6412. doi: 10.1007/s00330-020-07004-3 [15] Gurney Champion O J,Klaassen R,Froeling M,et al. Comparison of six fit algorithms for the intra-voxel incoherent motion model of diffusion-weighted magnetic resonance imaging data of pancreatic cancer patients[J]. PloS One,2018,13(4):0194590. [16] Liang C Y,Chen M D,Zhao X X,et al. Multiple mathematical models of diffusion-weighted magnetic resonance imaging combined with prognostic factors for assessing the response to neoadjuvant chemotherapy and radiation therapy in locally advanced rectal cancer[J]. Eur J Radiol,2019,110(5):249-255. -






 下载:
下载: