Analysis of Misdiagnosis of Endometrial Polyps under Vaginal Ultrasonography
-
摘要:
目的 评估超声影像对子宫内膜息肉的误诊率,如何应用简单、经济、节约时间的超声影像方法提高内膜息肉的诊断符合率。 方法 2019年1月至2021年5月在云南省第二人民医院超声诊断为内膜息肉及病理诊断结果为内膜息肉的484例患者纳入研究分析。根据超声类型将患者分为二维超声组、彩色多普勒(CDFI)组、能量多普勒(CDE)组,在不同组别内进行病理结果对照分析,寻找超声影像对子宫内膜息肉的误诊因素。 结果 与二维超声相比,CDE可以降低误诊率[OR(95%CI):0.172(0.048~0.625),P < 0.001],二维超声组、CDE组和CDFI组的误诊率分别为33.3%,7.9%和46% (P < 0.001)。 结论 在二维超声的基础上,应用CDE可以降低内膜息肉的误诊率,为临床医生短时间内提供有价值的信息。 Abstract:Objective To evaluate the misdiagnosis rate of endometrial polyps by ultrasound imaging, and to explore simple, cost-effective, and time-saving ultrasound imaging methods to improve the diagnostic compliance rate of endometrial polyps. Methods A total of 484 patients with endometrial polyp ultrasound and pathological diagnosis in the Second People’s Hospital of Yunnan Province from January 2019 to May 2021 were included in the study. The patients were divided into two dimensional ultrasound group, color Doppler (CDFI) group and power Doppler (CDE) group. The pathological results were analyzed in different groups to find the misdiagnosis factors of endometrial polyps by ultrasound images. Results Compared with 2D ultrasound, CDE reduced the misdiagnosis rate [OR (95% CI): 0.172 (0.048~0.625)] .The misdiagnosis rates of the two-dimensional ultrasound group, CDE group, and CDFI group were 33.3%, 7.9%, and 46.0%, respectively (P < 0.001). Conclusions Based on two-dimensional ultrasound, the application of CDE can reduce the misdiagnosis rate of endometrial polyps and provide clinicians with valuable information in a short time. -
表 1 不同类型超声的误诊分析
Table 1. Misdiagnosis analysis of different types of ultrasound
超声类型 总例数(n) 误诊例数(n) 误诊率(%) 二维超声 21 7 33.3* 二维超声 + CDE 63 5 7.9 二维超声 + CDFI 400 184 46.0* 与CDE组相比,*P < 0.05。 表 2 息肉超声诊断的误诊影响因素分析[n(%)]
Table 2. Analysis of influencing factors of misdiagnosis of uterine polyps [n(%)]
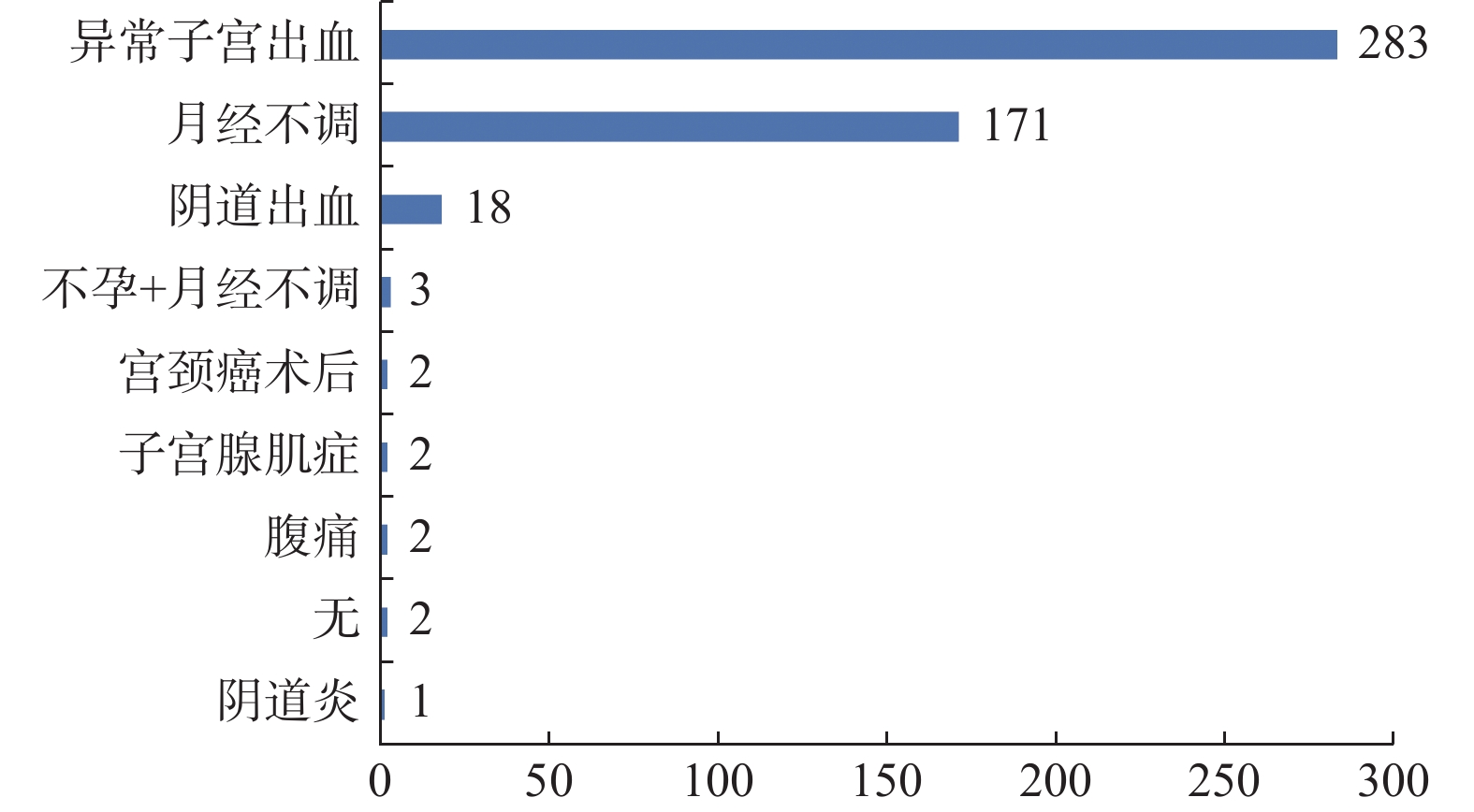
变量 正确组
(n = 288)误诊组
(n = 196)t/χ2 P 多因素分析 OR(95%CI) P 年龄,Median(Q1,Q3) 40(31,46) 38(32,45.25) 29045.500 0.586 类型 二维超声 14(67) 7(33) CDE 58(92) 5(8) 0.172(0.048~0.625) 0.001* CDFI 216(54) 184(46) 33.192 0.001* 1.704(0.673~4.311) 0.674 症状 腹痛 2(1) 0(0) Fisher 0.517 宫颈癌术后 1(0) 1(1) Fisher 1.000 不孕 3(1) 0(0) Fisher 0.276 月经不调 97(34) 77(39) 1.357 0.244 阴道炎 1(0) 0(0) Fisher 1.000 阴道出血 13(5) 5(3) 0.767 0.381 异常子宫出血 170(59) 113(58) 0.043 0.836 子宫腺肌症 2(1) 0(0) Fisher 0.517 绝经 34(12) 12(6) 3.744 0.053 节育环 14(5) 8(4) 0.033 0.856 *P < 0.05。 -
[1] 张嘉洁, 张静, 张嘉丽, 等 子宫内膜息肉、黏膜下肌瘤、内膜癌超声及病理鉴别诊断[J]. 中国超声医学杂志, 2016, 32(11): 1015-1018. [2] 陈会娟 经阴道彩色多普勒超声对老年性子宫黏膜下肌瘤与子宫内膜息肉的鉴别诊断意义[J]. 基层医学论坛, 2020, 24 (19): 2759-2760 [3] Vitale S G,Haimovich S,AS Laganà,et al. Endometrial Polyps:An evidence-based diagnosis and management guide[J]. European Journal of Obstetrics & Gynecology and Reproductive Biology,2021,260(7):70-77. [4] 董燕,柳建华. 阴道彩色多普勒超声对子宫内膜息肉及子宫内膜癌的诊断价值[J]. 广州医科大学学报,2017,45(2):29-31. doi: 10.3969/j.issn.2095-9664.2017.02.07 [5] 严霞瑜,罗红. 卵巢和子宫骶韧带息肉样子宫内膜异位症超声表现[J]. 中国超声医学杂志,2020,36(7):665-667. doi: 10.3969/j.issn.1002-0101.2020.07.031 [6] 高敏,史铁梅,张原溪,等. 超声弹性成像在子宫内膜病变中的研究进展[J]. 中国医学影像技术,2018,34(5):783-786. [7] Tanos V,Berry K E,Seikkula J,et al. The management of polyps in female reproductive organs[J]. International Journal of Surgery (London,England),2017,43:7-16. [8] 刘雨声,郭银树,段华,等. 绝经期子宫内膜息肉临床特点分析[J]. 中国微创外科杂志,2017,17(7):627-629. [9] 任美杰,杨敬春,杜岚,等. 静脉声学造影与经阴道彩色多普勒超声诊断子宫内膜息肉价值的比较[J]. 首都医科大学学报,2017,38(4):43-44. [10] 曹杰,胡尚英,田立碧,等. 宫腔镜和经阴道B超对子宫内膜息肉的诊断价值[J]. 重庆医学,2017,46(24):3348-3350. [11] 李晋. 经阴道二维及三维超声对子宫内膜息肉诊断的时效性及准确率对比分析[J]. 中外医学研究,2019,17(21):57-59. [12] Uglietti A,Buggio L,Farella M,et al. The risk of malignancy in uterine polyps:A systematic review and meta-analysis[J]. European Journal of Obstetrics & Gynecology and Reproductive Biology,2019,237:48-56. [13] Zolotukhin P,Aleksandrova A,Goncharova A,et al. Oxidative status shifts in uterine cervical incompetence patients[J]. Systems Biology in Reproductive Medicine,2014,60(2):98-104. doi: 10.3109/19396368.2013.864343 [14] 严霞瑜,罗红. 卵巢和子宫骶韧带息肉样子宫内膜异位症超声表现[J]. 中国超声医学杂志,2020,36(7):665-667. -






 下载:
下载: