Effect of Position on Ultrasonographic Measurement of Ligamentum Flavum Length of Lumbar Intervertebral Space in the Elderly Patients
-
摘要:
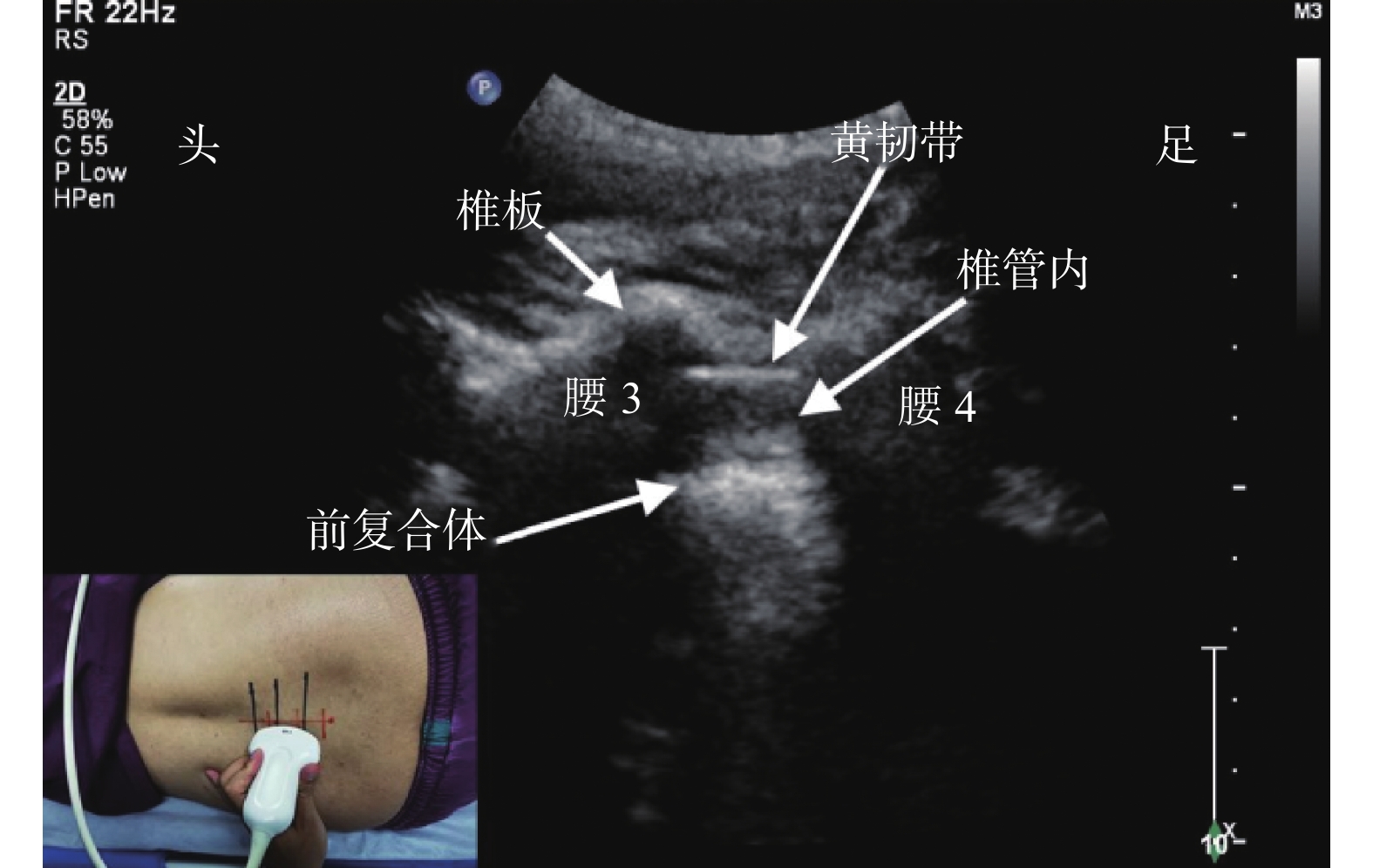
目的 探讨体位对老年患者腰椎间隙黄韧带长度超声测值的影响。 方法 选择年龄超过65岁拟行腰椎管内阻滞的老年患者40例,以旁正中矢状斜切面超声扫查坐位与左侧卧位下腰3/4、腰4/5、腰5/骶1椎间隙。测量并记录各间隙黄韧带前缘长度(anterior edge length of the ligamentum flavum,ALL)及皮肤至黄韧带前缘距离(distance from skin to the ligamentum flavum,DSL);评估并记录图像清晰度。 结果 与左侧卧位测值比较,坐位下腰5/骶1 ALL长,且长于坐位腰3/4值(P < 0.05);与腰3/4测值比较,坐位下腰5/骶1 DSL值浅(P < 0.05)。与腰5/骶1声图像比较,坐位与左侧卧位下腰3/4、4/5间隙左右两侧清晰度良好率较低(P < 0.05)。 结论 老年患者坐位下腰5/骶1 ALL超声测值长于左侧卧位相应值,也长于同一体位下腰3/4、腰4/5值,且其深度及声图像较其它间隙浅而清晰;建议此类患者采用旁正中穿刺入路行椎管内阻滞时,坐位下选择相对浅宽的腰5/骶1,左右两侧相当,尤其超声引导下。 Abstract:Objective To investigate effect of body position on ultrasonographic measurement of ligamentum flavum lengthin lumbar intervertebral space in the elderly patients. Methods 40 patients over 65 years of age who underwent spinal anesthesia were selected to examine the L 3/4, L 4/5 and L 5 / S1 intervertebral spaces. Anterioredge length oftheligamentum flavum (ALL) and distance from skin to theligamentum flavum (DSL) of L3/4, L4/5 and L5/S1 intervertebral spaces were measured by ultrasonic parasagittal oblique view in both sitting and left lateral decubitus position, and definition degree of each ultrasonic image were analyzed. Results Compared with the measurement in left lateral position, ALL at L5/S1 level in sitting position was longer, and longer than that at L3/4 in the same position (P < 0.05); DSL at L5/S1 was lower than that at L3/4 in sitting position (P < 0.05). Compared with ultrasonic definition of L5/S1, the fine definition rate of the left and right sides of L3/4 and L4/5 in both positions was lower (P < 0.05) . Conclusion The ALL ultrasonic measurement at L5/S1 level in sitting position was longer than that in left lateral decubitus position, and also longer than that at L3/4 and L4/5 in the same position, its depth and image were shallower and clearer than other spaces. It is recommended for elderly patients to use the paramidian puncture approach for lumbar anesthesia. The relatively shallow width of L5/ S1 should be selected under the sitting position, and the left and right sides are equivalent, especially under the guidance of ultrasound. -
Key words:
- Position /
- Elderly /
- Ligamentum flavum /
- Ultrasonography
-
表 1 不同体位下各间隙两侧ALL、DSL、DSA测值的比较[(
$\bar x \pm s $ ) mm]Table 1. Comparison of ALL,DSL and DPM measurements of both sides in different positions [(
$\bar x \pm s $ )mm]指标与部位 坐位 左侧卧位 F P 腰3/4 腰4/5 腰5/骶1 腰3/4 腰4/5 腰5/骶1 ALL 左 7.7 ± 3.1 9.7 ± 3.4 12.1 ± 2.3*# 7.1 ± 2.7 7.9 ± 2.6 9.4 ± 3.0 17.918 0.001 右 7.9 ± 3.0 9.8 ± 2.9 11.6 ± 2.4*# 6.7 ± 3.0 7.5 ± 3.2 9.4 ± 2.1 16.514 0.001 DSL 左 40.3 ± 4.7 35.2 ± 5.2 33.0 ± 4.9# 37.8 ± 11.3 33.8 ± 4.6 32.4 ± 6.1 8.728 0.001 右 39.7 ± 5.5 36.3 ± 4.5 32.1 ± 5.4# 36.3 ± 4.5 34.4 ± 5.0 32.5 ± 5.3 12.614 0.001 DPM 左 12.3 ± 3.1 13.5 ± 3.4 14.4 ± 3.7 13.3 ± 3.4 13.0 ± 3.1 15.0 ± 3.9 3.199 0.008 右 14.1 ± 3.6 13.1 ± 4.0 13.7 ± 4.0 12.9 ± 3.9 12.5 ± 2.8 14.5 ± 4.2 1.633 0.152 与左侧卧位腰5/骶1值比较,*P < 0.05;与腰3/4值比较,#P < 0.05。 表 2 不同体位下各间隙两侧声图像清晰度比较[n(%)]
Table 2. Comparison of ultrasonographic definition of each intervertebral space in different positions [n(%)]
部位与清晰度 坐位 左侧卧位 χ2 P 腰3/4 腰4/5 腰5/骶1 腰3/4 腰4/5 腰5/骶1 左 良好 19(47.5)* 21(52.5)* 32(80.0) 18(45.0)* 22(55.0)* 31(77.5) 17.089 0.004 一般 5(12.5) 5(12.5) 2(5.0) 7(17.5) 5(12.5) 1(2.5) 差 16(40.0) 14(35.0) 6(15.0) 15(37.5) 13(32.5) 8(20.0) 右 良好 18(45.0)* 20(50.0)* 30(75.0) 19(47.5)* 21(52.5)* 32(80.0) 18.521 0.002 一般 8(20.0) 5(12.5) 6(15.0) 11 (27.5) 5(12.5) 2(5.0) 差 14(35.0) 15(37.5) 4(10.0) 10 (25.0) 14(35.0) 6(15.0) 与腰5/骶1比较,*P < 0.05。 表 3 声像图清晰度良好患者各间隙两侧ALL、DSL、DPM测值比较[(
$\bar x \pm s $ ),mm]Table 3. Comparison of ALL,DSL and DPM measurements on both sides of each space in patients with fine ultrasonographic definition in different positions [(
$\bar x \pm s $ ),mm]部位与指标 坐位 左侧卧位 F P 腰3/4 腰4/5 腰5/骶1 腰3/4 腰4/5 腰5/骶1 左 n 19 21 32 18 22 31 ALL 7.8 ± 3.6 10.1 ± 4.0 12.3 ± 3.1*# 7.3 ± 3.2 8.4 ± 3.0 9.1 ± 2.9 8.067 0.001 DSL 41.2 ± 3.9 36.1 ± 6.3 33.2 ± 4.7# 37.7 ± 9.7 33.8 ± 4.6 33.2 ± 5.6 6.397 0.001 DPM 11.8 ± 3.2 13.0 ± 3.6 13.8 ± 3.9 12.9 ± 4.3 13.4 ± 4.0 14.3 ± 3.6 1.211 0.307 右 n 18 20 30 19 21 32 ALL 7.6 ± 3.2 9.7 ± 3.2 11.9 ± 3.6*# 6.8 ± 3.4 7.4 ± 3.4 9.2 ± 3.0 8.136 0.001 DSL 40.1 ± 5.6 36.8 ± 6.1 33.8 ± 5.8# 36.9 ± 4.9 34.7 ± 4.7 32.9 ± 5.9 4.929 0.001 DPM 13.7 ± 4.1 13.5 ± 4.5 13.2 ± 3.3 13.2 ± 4.0 12.7 ± 3.2 14.6 ± 4.1 0.763 0.578 与左侧卧位腰5/骶1值比较,*P < 0.05;与腰3/4值比较,#P < 0.05。 -
[1] Tang Z,Zhang C,Xu Z,et al. Observation of single spinal anesthesia by 25G needle puncture through a lateral crypt for hip surgery in elderly patients[J]. Medicine (Baltimore),2019,98(27):16334. [2] Hulmani D,Garg B,Mehta N,et al. Morphological changes in the ligamentum flavum in degenerative lumbar canal stenosis:A prospective,comparative study[J]. Asian Spine J,2020,14(6):773-781. doi: 10.31616/asj.2020.0041 [3] Rabinowitz A,Bourdet B,Minville V,et al. The paramedian technique:A superior initial approach to continuous spinal anesthesia in the elderly[J]. Anesth Analg,2007,105(6):1855-1857. doi: 10.1213/01.ane.0000287655.95619.fa [4] Park S K,Yoo S,Kim W H,et al. Ultrasound-Assisted vs. landmark-guided paramedian spinal anaesthesia in the elderly:A randomised controlled trial[J]. Eur J Anaesthesiol,2019,36(10):763-771. doi: 10.1097/EJA.0000000000001029 [5] Elsharkawy H,Maheshwari A,Babazade R,et al. Real-time ultrasound guided spinal anesthesia in patients with predicted difficult anatomy[J]. Minerva Anestesiol,2017,83(5):465-473. [6] Bae J,Park S K,Yoo S,et al. Influence of age,laterality,patient position,and spinal level on the interlamina space for spinal puncture[J]. Reg Anesth Pain Med,2020,45(1):27-31. doi: 10.1136/rapm-2019-100980 [7] Kallidaikurichi S K,Iohom G,Loughnane F,et al. Conventional landmark-guided midline versus preprocedure ultrasound-guided paramedian techniques in spinal anesthesia[J]. Anesth Analg,2015,121(4):1089-1096. doi: 10.1213/ANE.0000000000000911 [8] Chin K J,Ramlogan R,Arzola C,et al. The utility of ultrasound imaging in predictingease of performance of spinal anesthesia in an orthopedic patient population[J]. Reg Anesth Pain Med,2013,38(1):34-38. [9] Xu C S,Qu X D,Qu Z J,et al. Effect of subarachnoid anesthesia combined with propofol target-controlled infusion on blood loss and transfusion for posterior total hip arthroplasty in elderly patients[J]. Chin Med J (Engl),2020,133(6):650-656. [10] 陈燕,何亮,衡新华. 椎管内麻醉后神经并发症600例分析[J]. 昆明医学院学报,2011,32(11):99-102. [11] Vogt M,Van Gerwen D J,Lubbers W,et al. Optimal point of insertion and needle angle in neuraxial blockade using a midline approach:A study in computed tomography scans of adult patients[J]. Reg Anesth Pain Med,2017,42(5):600-608. doi: 10.1097/AAP.0000000000000653 [12] Kim H,Won D,Chang J E,et al. Ultrasound assessment of the anatomic landmarks for spinal anesthesia in elderly patients with hip fracture:A prospective observational study[J]. Medicine (Baltimore),2019,98(27):16388. [13] 费昱达,崔旭蕾. 超声引导下老年患者硬膜外穿刺二例[J]. 临床麻醉学杂志,2018,34(1):98-99. [14] Srinivasan K K,Leo A M,Iohom G,et al. Pre-procedure ultrasound-guided paramedian spinal anaesthesia at L5-S1:Is this better than landmark-guided midline approach? A randomised controlled trial[J]. Indian J Anaesth,2018,62(1):53-60. doi: 10.4103/ija.IJA_448_17 [15] Da Silva L C,Pacheco P F,Sellera F P,et al. The use of ultrasound to assist epidural injection in obese dogs[J]. Vet Anaesth Analg,2020,47(1):137-140. doi: 10.1016/j.vaa.2019.10.003 [16] Soni P,Punj J. Ultrasound-guided lumbar transforaminal epidural injection:A narrative review[J]. Asian Spine J,2021,15(2):261-270. doi: 10.31616/asj.2019.0245 [17] Di Filippo A,Falsini S,Adembri C. Minimum anesthetic volume in regional anesthesia by using ultrasound-guidance[J]. Braz J Anesthesiol,2016,66(5):499-504. doi: 10.1016/j.bjan.2014.05.007 -






 下载:
下载: