Nutritional Status of Elderly Tuberculosis Patients in Yunnan
-
摘要:
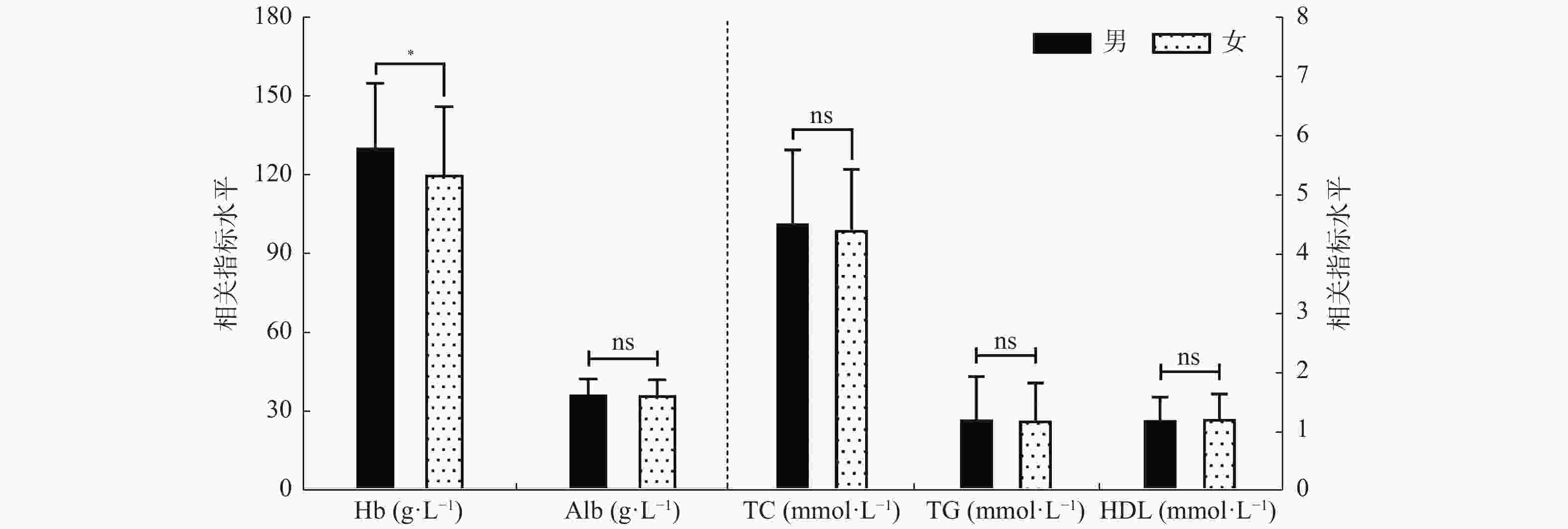
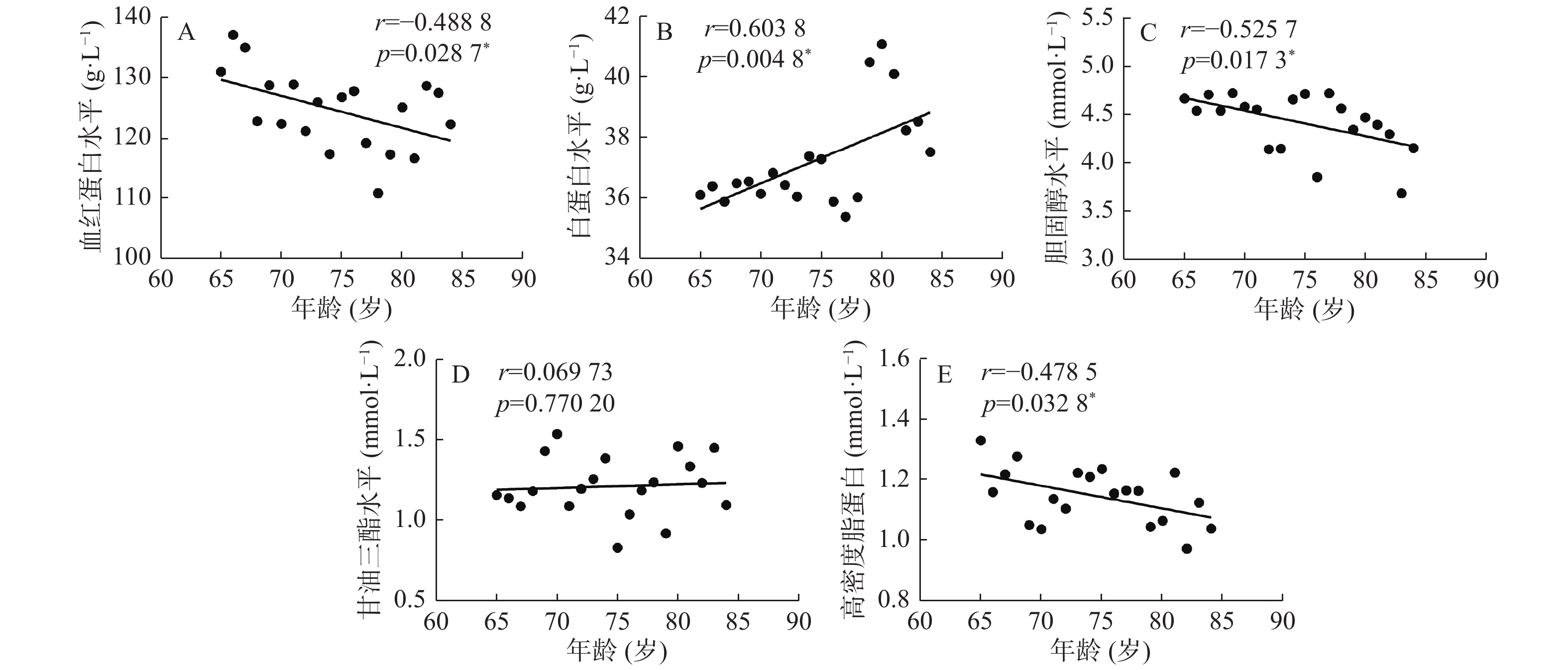
目的 分析云南省老年结核病患者营养状况,为预防老年结核病患者营养不良及营养干预提供参考依据。 方法 收集2019年6月至2021年6月在昆明市第三人民医院收治的1316例年龄≥65岁老年结核病患者为病例组,另选同期健康体检人群520例作为对照组。比较2组营养相关指标水平,分析老年结核病患者的营养状况。 结果 与对照组比较,结核病患者血红蛋白(Hb)[(126.40±25.51) g/L]、淋巴细胞计数(LYM) [(1.24±0.59)×109/L]、血清总蛋白(TP) [ (66.00±8.22) g/L]、白蛋白(Alb) [ (36.03±6.04) g/L]、白/球比(A/G) [1.25±0.33]、胆固醇(TC) [(4.48±1.18) mmol/L]、甘油三酯(TG) [(1.19±0.70) mmol/L]和高密度脂蛋白(HDL-C) [(1.19±0.40) mmol/L]水平均低于对照组(t=15.640,26.240,14.770,35.900,35.080,8.272,7.986,7.381;P均<0.05);红细胞计数(Rbc) [ (4.92±0.52)×1012/L]、球蛋白(Glob) [(29.97±6.06) g/L]水平高于对照组(t = 13.060,15.490;P均< 0.05)。结核病患者贫血[10.50% (105/1000)]、低蛋白血症[30.30% (303/1000)]、高密度脂蛋白偏低 [27.00% (270/1000)] 比例高于对照组(χ2 = 28.900,147.900,53.490;P均< 0.05);高胆固醇血症[11.00% (110/1000)]、高甘油三酯血症[7.20% (72/1000)]比例低于对照组 (χ2 = 56.640,179.900;P < 0.05)。结核病患者营养相关指标程度以轻度和中度为主,结核合并糖尿病患者Alb[(32.24±6.90) g/L]水平低于单纯结核病组[(36.03±6.04) g/L] (t = 3.18;P < 0.01);Hb[(146±23.23) g/L]、TC[(5.54±0.85) mmol/L]水平高于单纯结核病组[分别为(126.40±25.51) g/L、(4.48±1.18) mmol/L] (t = 3.720,8.420;P < 0.05)。结核病患者中,Hb、Alb、TC、HDL-C水平与年龄都有相关性(r = -0.489,0.604,-0.526,-0.479;P < 0.05),TG水平与年龄不相关(r = 0.070;P = 0.770);Alb、TC、TG、HDL-C水平在性别表达中差异无统计学意义 (t = 0.601,0.942,0.299,0.485;P = 0.548,0.347,0.765,0.628)。 结论 云南省老年结核病患者营养不良发生率较健康人高,营养不良程度与年龄相关,营养相关疾病以轻度和中度为主,此外,糖尿病可加重老年结核病患者的营养不良程度。 Abstract:Objective To investigate the nutritional status of elderly tuberculosis patients in Yunnan and provide evidence for the prevention of malnutrition of elderly tuberculosis patients and nutritional intervention. Methods A total of 1316 elderly tuberculosis patients aged ≥65 years who were admitted to The Third People’s Hospital of Kunming from June 2019 to June 2021 were selected as the case group, and 520 healthy people who underwent physical examination during the same period were selected as the control group. The nutrition-related indexes of the two groups were compared to analyze the nutritional status of elderly tuberculosis patients. Results Compared with the control group, TB patients’ hemoglobin (Hb) (126.40 + 25.51) g/L, lymphocyte count (LYM) [(1.24 + 0.59) x 109/L], serum total protein (TP) (66.00 + 8.22) g/L, albumin [(36.03) +/-6.04 g/L), albumin/globulin ratio (A/g) [1.25 +/-0.33), cholesterol (TC) [(4.48 +/-1.18) mmol/L], triglycerides (TG) (1.19 +/-0.70) mmol/L and high-density lipoprotein (HDL -C) [(1.19 ± 0.40) mmol/L] levels were lower than those in the control group (t =15.640, 26.240, 14.770, 35.900, 35.080, 8.272, 7.986, 7.381; P < 0.05); The RBC conut [(4.92 ± 0.52)×1012/L] and globulin level [(29.97 ± 6.06) g/L] were higher than those in the control group (t = 13.060, 15.490; P < 0.05). The prevalence of anemia [10.50% (105/1000)], hypoproteinemia [30.30% (303/1000)] and low high-density lipoprotein [27.00% (270/1000)] in tuberculosis patients were higher than those in control group (χ2 = 28.900, 147.900, 53.490; P < 0.05). The prevalence of hypercholesterolemia [11.00% (110/1000)] and hypertriglyceridemia [7.20% (72/1000)] were lower than that of the control group (χ2 = 56.640, 179.900; P < 0.05). The degree of nutrition-related diseases in TB patients are mild and moderate. The level of Alb[(32.24±6.90) g/L] in patients with tuberculosis combined with diabetes was lower than that in patients with tuberculosis alone [(36.03 ± 6.04) g/L] (t = 3.18; P < 0.01); The levels of Hb[(146±23.23) g/L] and TC[(5.54±0.85) mmol/L] were higher than those of the tuberculosis group [(126.40 ± 25.51) g/L and (4.48 ± 1.18) mmol/L] (t = 3.720, 8.420; P < 0.05). In tuberculosis patients, Hb, Alb, TC, HDL-C levels were correlated with age (r = -0.489, 0.604, -0.526, -0.479; P < 0.05), while TG level was not correlated with age (r = 0.070; P = 0.770). There were no significant differences in the levels of Alb, TC, TG and HDL-C in gender (t = 0.601, 0.942, 0.299, 0.485; P = 0.548, 0.347, 0.765, 0.628). Conclusion The incidence of malnutrition in elderly tuberculosis patients in Yunnan was higher than healthy people, The degree of malnutrition is age-related, and nutrition-related diseases are mainly mild and moderate, in addition, diabetes can aggravate the degree of malnutrition in elderly tuberculosis patients. -
Key words:
- Tuberculosis /
- The elderly /
- Patient /
- Nutritional status
-
表 1 对照组和病例组一般情况 [n(%)]
Table 1. Demographic data of control group and case group [n(%)]
分类 对照组
(n = 520)病例组
(n = 1000)χ2 P 性别 1.892 0.169 男 273(52.50) 562(56.20) 女 247(47.50) 438(43.80) 年龄组(岁) 1.801 0.615 65~ 197(37.88) 406(40.60) 70~ 152(29.23) 267(26.70) 75~ 94(18.08) 189(18.90) 80~84 77(14.81) 138(13.80) 表 2 对照组和病例组相关指标分析(
$\bar x \pm s $ )Table 2. Analysis of related indicators in control group and case group (
$\bar x \pm s $ )相关指标 对照组(n=520) 实验组(n=1000) t P Hb(g/L) 153.50 ± 16.11 126.4 ± 25.51 15.640 0.0010* Rbc(1012/L) 4.17 ± 0.85 4.92 ± 0.52 13.060 0.0008* LYM(109/L) 2.38 ± 0.71 1.24 ± 0.59 26.240 0.0013* TP(g/L) 71.55 ± 4.34 66.00 ± 8.22 14.770 0.0015* Alb(g/L) 45.97 ± 3.33 36.03 ± 6.04 35.900 0.0011* Glob(g/L) 25.58 ± 4.01 29.97 ± 6.06 15.490 0.0005* A/G 1.85 ± 0.36 1.25 ± 0.33 35.080 0.0012* TC(mmol/L) 5.11 ± 1.16 4.48 ± 1.18 8.272 0.0018* TG(mmol/L) 1.60 ± 0.86 1.19 ± 0.70 7.986 0.0007* HDL-C(mmol/L) 1.37± 0.35 1.19 ± 0.40 7.381 0.0016* Hb:血红蛋白;Rbc:红细胞计数;LYM :淋巴细胞;TP:总蛋白;Alb:白蛋白;Glob:球蛋白;A/G:白/球比;TC:胆固醇;TG:甘油三酯;HDL-C:高密度脂蛋白;*P < 0.05。 表 3 对照组和病例组营养相关疾病分析(%)
Table 3. Analysis of nutrition-related diseases in control group and case group (%)
组别 贫血 低蛋白血症 高胆固醇血症 高甘油三酯血症 高密度脂蛋白缺乏症 对照组(n = 520) 14 (2.69) 18 (3.46) 135 (25.96) 177 (34.03) 56 (10.77) 实验组(n = 1000) 105 (10.50) 303 (30.30) 110 (11.00) 72 (7.20) 270 (27.00) χ2 28.900 147.900 56.640 179.900 53.490 P 0.001* 0.001* 0.001* 0.002* 0.003* *P < 0.05。 表 4 病例组相关指标程度分析[n(%)]
Table 4. Analysis of the degree of relevant indicators in the case group [n(%)]
组别 贫血 低蛋白血症 高胆固醇血症 高甘油三酯血症 高密度脂蛋白缺乏症 χ2 P 轻度 32 (30.5) 225 (74.3) 42 (38.2) 40 (55.5) 78 (28.9) 195.6 0.001* 中度 61 (58.1) 73 (24.0) 61 (55.4) 30 (41.7) 120 (44.4) 重度 12 (11.4) 5 (1.7) 7 (6.4) 2 (2.8) 72 (26.7) 合计 105 303 110 72 270 *P < 0.05。 表 5 结核合并糖尿病营养状况分析(
$\bar x \pm s $ )Table 5. Analysis of nutritional status of tuberculosis complicated with diabetes mellitus (
$\bar x \pm s $ )相关指标 结核病(n = 960) 结核合并糖尿病(n = 40) t P Hb (g/L) 126.40 ± 25.51 146 ± 23.23 3.720 0.001* Alb (g/L) 36.03 ± 6.04 32.24 ± 6.90 3.180 0.003* TC (mmol/L) 4.48 ± 1.18 5.54 ± 0.85 8.420 0.000* TG (mmol/L) 1.19 ± 0.69 1.22 ± 0.65 0.260 0.799 HDL-C (mmol/L) 1.19 ± 0.40 1.11 ± 0.36 1.590 0.118 *P < 0.05。 表 6 相关指标与性别关系分析 (
$\bar x \pm s $ )Table 6. Analysis of the relationship between related indicators and gender (
$\bar x \pm s $ )相关指标 男 女 t P Hb(g/L) 130.40 ± 24.40 119.90 ± 25.95 7.386 0.001* Alb(g/L) 36.10 ± 6.10 35.92 ± 5.95 0.601 0.548 TC(mmol/L) 4.52 ± 1.25 4.41 ± 1.02 0.942 0.347 TG(mmol/L) 1.12 ± 0.72 1.18 ± 0.66 0.299 0.765 HDL-C(mmol/L) 1.19 ± 0.39 1.20 ± 0.42 0.485 0.628 *P < 0.05。 -
[1] Anuradha R,Munisankar S,Bhootra Y,et al. Coexistent malnutrition is associated with perturbations in systemic and antigen-specific cytokine responses in latent tuberculosis infection[J]. Clin Vaccine Immunol,2016,23(4):339-345. doi: 10.1128/CVI.00009-16 [2] Campos-Gongora E,Lopez-Martinez J,Huerta-Oros J,et al. Nutritional status evaluation and nutrient intake in adult patients with pulmonary tuberculosis and their contacts[J]. J Infect Dev Ctries,2019,13(4):303-310. doi: 10.3855/jidc.11267 [3] 宣兆元,孙建军,杨燕,等. 结核病与营养状况关系研究[J]. 药物与人,2014,27(6):315. [4] 马艳,高微微. 老年结核病防治现状与展望[J]. 结核病与肺部健康杂志,2018,7(3):161-166. [5] 陆涛. 老年结核病流行病学研究现状[J]. 职业与健康,2019,35(12):1725-1728. [6] 周林,刘二勇,孟庆琳,等. 《WS 288—2017肺结核诊断》标准实施后肺结核诊断质量评估分析[J]. 中国防痨杂志,2020,42(9):910-915. doi: 10.3969/j.issn.1000-6621.2020.09.005 [7] 刘梦文,殷春杰,肖开提·米吉提,等. 结核病患者营养状况调查分析[J]. 临床肺科杂志,2021,26(4):538-542. doi: 10.3969/j.issn.1009-6663.2021.04.012 [8] 中国高血压防治指南修订委员会. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志,2019,24(1):24-56. doi: 10.3969/j.issn.1007-5410.2019.01.002 [9] 王晋文,芮章茹,任晓燕. 云南慢性肾衰竭患者病因与转归分析[J]. 昆明医学院学报,2010,31(10):102-104. [10] 陈薇,丁芹,顾颖,等. 上海市900例老年住院结核病患者营养状况调查分析[J]. 中国防痨杂志,2020,42(7):725-730. doi: 10.3969/j.issn.1000-6621.2020.07.015 [11] 顾景范, 杜寿玢, 郭长江, 等. 现代临床营养学[M]. 第2版. 延吉: 吉林延吉出版社, 2009: 1-746. [12] 高雅竹,唐芳馨. 老年住院患者营养风险和营养状况的评估[J]. 中国临床医生杂志,2020,48(7):784-786. doi: 10.3969/j.issn.2095-8552.2020.07.008 [13] Kim D K,Kim H J,Kwon S Y,et al. Nutritional deficit as a negative prognostic factor in patients with miliary tuberculosis[J]. Eur Respir J,2008,32(4):1031-1036. doi: 10.1183/09031936.00174907 [14] 高微微. 老年肺结核患者治疗问题探讨[J]. 中华结核和呼吸杂志,2014,37(10):732-733. doi: 10.3760/cma.j.issn.1001-0939.2014.10.006 [15] Xiong J,Wang M,Zhang Y,et al. Association of geriatric nutritional risk index with mortality in hemodialysis patients:A meta-analysis of cohort studies[J]. Kidney Blood Press Res,2018,43(6):1878-1889. doi: 10.1159/000495999 [16] Saghafi-Asl M,Vaghef-Mehrabany E,Karamzad N,et al. Geriatric nutritional risk index as a simple tool for assessment of malnutrition among geriatrics in northwest of iran:Comparison with mini nutritional assessment[J]. Aging Clin Exp Res,2018,30(9):1117-1125. doi: 10.1007/s40520-018-0892-2 [17] 陆涛,陈文才. 2012—2016年南宁市老年结核病流行特征与防治策略[J]. 职业与健康,2018,34(3):352-355. [18] 谭守勇. 不容忽视耐多药结核病患者营养支持治疗的作用[J]. 中国防痨杂志,2019,41(2):121-123. doi: 10.3969/j.issn.1000-6621.2019.02.001 [19] Dye C,Bourdin T B,Lonnroth K,et al. Nutrition,diabetes and tuberculosis in the epidemiological transition[J]. PLoS One,2011,6(6):21161. doi: 10.1371/journal.pone.0021161 [20] 诸骏仁,高润霖,赵水平,等. 中国成人血脂异常防治指南(2016年修订版)[J]. 中华心血管病杂志,2016,44(10):833-853. doi: 10.3760/cma.j.issn.0253-3758.2016.10.005 [21] Muchsin M,Siregar F A,Sudaryati E. The influence of nutritional status and ventilation on the incidence of pulmonary tuberculosis at langsa[J]. Open Access Maced J Med Sci,2019,7(20):3421-3424. doi: 10.3889/oamjms.2019.436 -






 下载:
下载: