Diagnostic Value of Gated Myocardial Perfusion Imaging Combined with NT-proBNP in Chronic Heart Failure
-
摘要:
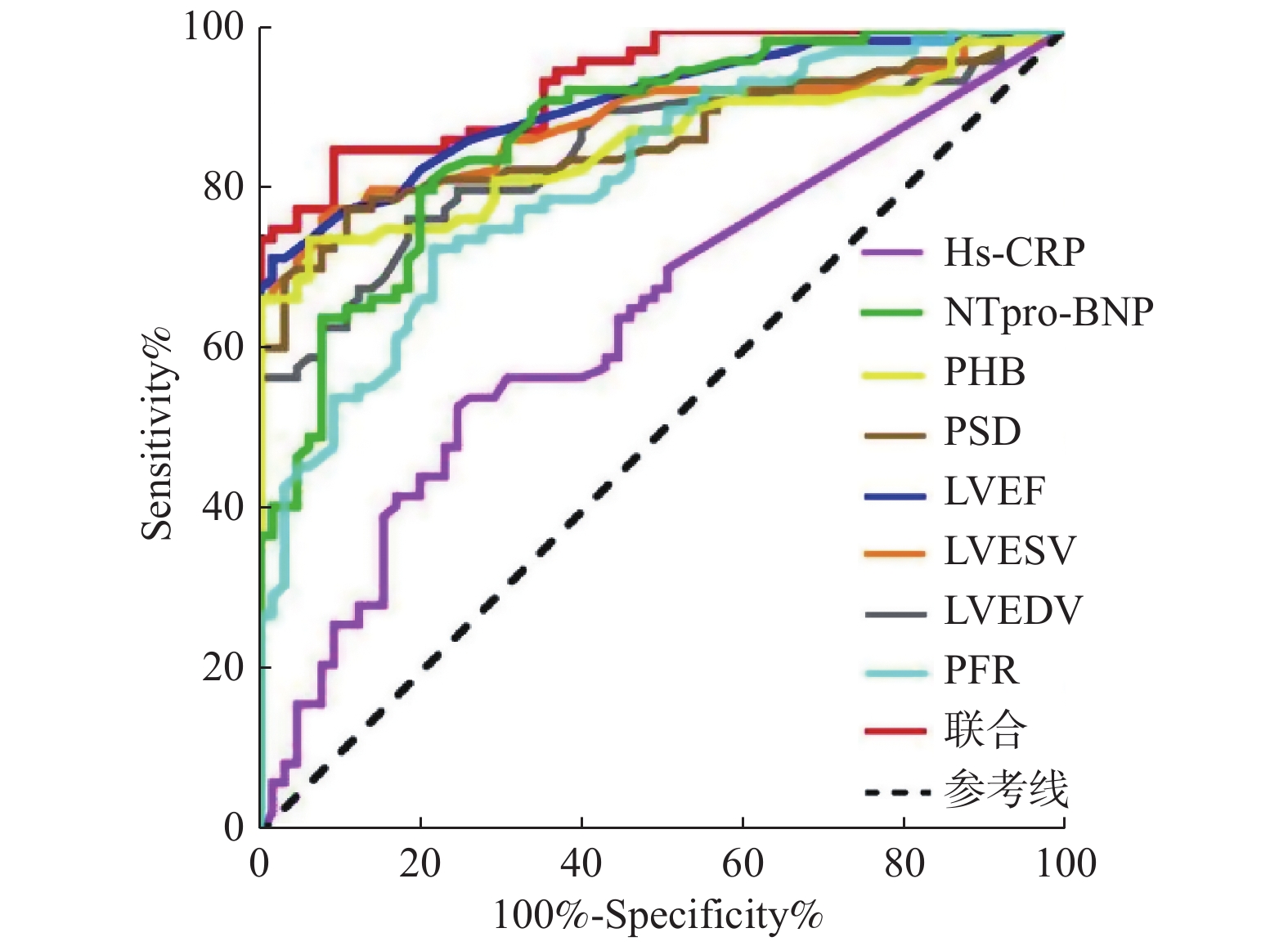
目的 探讨门控心肌灌注显像(GMPI)、超敏C反应蛋白(Hs-CRP)及联合N末端B型利钠肽原(NT-proBNP)检测在慢性心力衰竭鉴别诊断中的临床应用价值。 方法 纳入2020年1月至2021年12月于昆明医科大学附属延安医院行GMPI检查最终确诊为慢性心力衰竭的患者81例作为心力衰竭组,选取同期行GMPI检查最终确诊为非心力衰竭的受检者65例作为非心力衰竭组,收集所有入组对象的GMPI指标:PHB、PSD、LVEF、LVEDV、LVESV、PFR及实验室指标:Hs-CRP、NT-proBNP。分析GMPI的各项参数、Hs-CRP及NT-proBNP指标对慢性心力衰竭的诊断效能。 结果 GMPI各项参数及NTpro-BNP诊断慢性心力衰竭的AUC均 > 0.800, P均 < 0.001;Hs-CRP诊断慢性心力衰竭的AUC为0.640, P < 0.05;使用LVEDV+LVESV+NTpro-BNP联合方案的AUC为0.937, P < 0.001。比较不同参数的AUC大小:GMPI各项参数与NTpro-BNP比较差异无统计学意义( P均 > 0.05),GMPI各项参数、NTpro-BNP的AUC均高于Hs-CRP( P均 < 0.05),LVEDV+LVESV+NTpro-BNP联合方案的AUC高于GMPI各项参数、NTpro-BNP及Hs-CRP( P均 < 0.05)。 结论 单一使用Hs-CRP水平在慢性心力衰竭鉴别诊断方面价值有限;GMPI各项参数与传统心衰指标NTpro-BNP诊断慢性心力衰竭的准确性相当,在鉴别慢性心力衰竭均具有较高的诊断效力;GMPI联合NTpro-BNP使用可取得更高的诊断准确性,值得临床进一步应用。 Abstract:Objectives To investigate the clinical value of gated myocardial perfusion imaging (GMPI), high-sensitivity C-reactive protein (Hs-CRP) and N-terminal B-type natriuretic peptide (NT-proBNP) in the differential diagnosis of chronic heart failure. Methods Eighty one patients ultimately diagnosed with chronic heart failure by GMPI examination at Yanan Hospital Affiliated to Kunming Medical University between January 2020 and December 2021 were included as the heart failure group, sixty five subjects with a final diagnosis of non heart failure by GMPI examination during the same period were selected as the non heart failure group. After that, GMPI indicators: PHB, PSD, LVEF, LVEDV, LVESV, PFR and laboratory indicators: Hs-CRP, NT-proBNP were collected for all enrolled subjects so as to analyze the diagnostic efficacy of each parameter of GMPI, Hs-CRP and NT-proBNP indicators for chronic heart failure. Results All parameters of GMPI and AUC of NTpro-BNP in the diagnosis of chronic heart failure were > 0.800, P < 0.001; the AUC of Hs-CRP in the diagnosis of heart failure was 0.640, P < 0.05; the AUC of the combined scheme of LVEDV + LVESV + NTpro-BNP was 0.937, P < 0.001. Comparing AUC of different parameters: there was no significant difference between GMPI and NTpro-BNP ( P > 0.05), all parameters of GMPI and AUC of NTpro-BNP were higher than Hs-CRP ( P < 0.05), the AUC of the combined scheme of LVEDV + LVESV + NTpro-BNP was higher than that of GMPI, NTpro-BNP and Hs-CRP ( P < 0.05). Conclusion The value of Hs-CRP alone in the differential diagnosis of chronic heart failure is limited; GMPI parameters are equivalent to the accuracy of traditional heart failure index NTpro-BNP in the diagnosis of heart failure and have the high diagnostic efficacy in the differentiation of the heart failure; GMPI combined with NTpro-BNP can achieve the higher diagnostic accuracy, which is worthy of further clinical application. -
表 1 心力衰竭组与非心力衰竭组一般资料的比较[ $ \bar{x} \pm s $/M(P25,P75)/n(%)]
Table 1. Comparison of general data between heart failure group and non heart failure group[ $ \bar{x} \pm s $/M(P25,P75)/n(%)]
项目 心力衰竭组(n = 81) 非心力衰竭组(n = 65) t/Z/χ2 P 基本情况 性别(男/女) 56/25 39/26 1.324 0.250 年龄(岁) 56.1 ± 15.6 53.7 ± 9.7 1.093 0.276 BMI(kg/m2) 24.09(22.22,27.25) 24.46(21.31,25.75) 0.778 0.437 心率(次/min) 70(63.5,79.5) 70(64.5,81.5) 0.282 0.778 合并症情况 高血压 [n(%)] 43(53.1%) 27(41.5%) 1.927 0.165 糖尿病 [n(%)] 24(29.6%) 12(18.5%) 2.421 0.120 高脂血症 [n(%)] 19(23.5%) 7(10.8%) 3.966 0.046* 心律失常[n(%)] 20(24.7%) 22(33.8%) 1.475 0.225 肺炎[n(%)] 3(3.7%) 2(3.1%) 0.043 0.836 冠心病[n(%)] 57(70.4%) 25(38.5%) 14.913 < 0.001* 肺动脉高压[n(%)] 10(12.3%) 3(4.6%) 2.657 0.103 心肌病[n(%)] 10(12.3%) 0(0%) 6.788 0.009* *P < 0.05。 表 2 不同的观察者处理GMPI参数的可信度与可重复性(n = 10)
Table 2. Reliability and repeatability of GMPI parameters processed by different observers (n = 10)
项目 第1次处理 第2次处理 Alpha ICC F P PHB(°) 55.00(32.75,89.75) 46.50(32.00,98.00) 0.981 0.963 0.138 < 0.001* PSD(°) 18.00(9.60,33.03) 15.70(11.05,32.93) 0.988 0.977 0.007 < 0.001* LVEF(%) 70.50(35.75,73.50) 71.50(37.50,73.25) 0.998 0.995 0.000 < 0.001* LVEDV(mL) 77.00(66.75,188.25) 78.50(71.50,191.75) 0.991 0.982 4.075 < 0.001* LVESV(mL) 21.00(18.25,125.75) 22.50(18.75,125.00) 0.993 0.985 1.816 < 0.001* PFR(EDV/s) 3.83(2.19,4.53) 3.39(1.84,4.61) 0.958 0.920 0.571 < 0.001* *P < 0.05。 表 3 心力衰竭组与非心力衰竭组GMPI参数指标、Hs-CRP及NT-proBNP水平的比较[ $\bar x \pm s $/M(P25,P75)]
Table 3. Comparison of GMPI parameters, Hs-CRP and NT-proBNP levels between heart failure group and non heart failure group[ $\bar x \pm s $/M(P25,P75)]
项目 心力衰竭组(n = 81) 非心力衰竭组(n = 65) t/Z P PHB(°) 98.0(49.0,178.5) 37.0(30.5,46.5) 7.404 < 0.001* PSD(°) 39.0(18.9,54.0) 12.0(9.3,15.6) 7.580 < 0.001* LVEF(%) 51(35,66) 72(69,75) 8.487 < 0.001* LVEDV(mL) 131(94,189) 72(59.5,88.0) 7.226 < 0.001* LVESV(mL) 61.0(33.0,118.5) 20(16,27) 8.017 < 0.001* PFR(EDV/s) 2.86 ± 1.07 4.38 ± 1.44 7.295 < 0.001* NTpro-BNP(ng/L) 479.00(173.50,1785.00) 73.00(48.50,140.00) 7.742 < 0.001* Hs-CRP(mg/L) 1.69(0.50,5.07) 0.54(0.50,1.65) 2.994 0.003* *P< 0.05。 表 4 ROC曲线分析
Table 4. ROC curve analysis
项目 AUC P 95%CI 截断值 灵敏度(%) 特异度(%) 准确率(%) Hs-CRP(mg/L) 0.640ab 0.002* 0.557~0.718 1.5 53.09 75.38 62.33 NTpro-BNP(ng/L) 0.873a < 0.001* 0.818~0.929 150 80.25 80.00 80.14 PHB(°) 0.857ac < 0.001* 0.795~0.919 56 74.07 93.85 82.88 PSD(°) 0.866ac < 0.001* 0.805~0.926 17.9 77.78 89.23 82.88 LVEF(%) 0.909ac < 0.001* 0.850~0.950 63 71.60 98.46 83.56 LVEDV(mL) 0.849ac < 0.001* 0.780~0.902 92 76.54 81.54 78.77 LVESV(mL) 0.887ac < 0.001* 0.824~0.933 32 76.54 92.31 83.56 PFR(EDV/s) 0.815ac < 0.001* 0.743~0.875 3.31 72.84 78.46 75.34 联合 0.937 < 0.001* 0.884~0.970 - 85.19 90.77 87.67 注:联合:LVEDV+LVESV+NTpro-BNP:与NTpro-BNP比较,bP < 0.05;与联合组比较, aP < 0.05;与Hs-CRP比较, cP < 0.05; *P < 0.05。 -
[1] 王华,梁延春. 中国心力衰竭诊断和治疗指南2018[J]. 中华心力衰竭和心肌病杂志,2018,46(4):196-197. doi: 10.3760/cma.j.issn.2096-3076.2018.12.002 [2] Ponikowski P,Voors A A,Anker S D,et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure:The task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC[J]. Eur Heart J,2016,37(27):2129-2200. doi: 10.1093/eurheartj/ehw128 [3] 王华,李莹莹,柴坷,等. 中国住院心力衰竭患者流行病学及治疗现状[J]. 中华心血管病杂志,2019,47(11):865-874. [4] Charach G,Grosskopf I,Galin L,et al. Usefulness of cardiac biomarkers for prognosis of better outcomes in chronic heart failure:Retrospective 18-year follow-up study[J]. Medicine (Baltimore),2021,100(5):e23464. [5] 中国医疗保健国际交流促进会循证医学分会,海峡两岸医药卫生交流协会老年医学专业委员会. 心力衰竭生物标志物中国专家共识[J]. 中华检验医学杂志,2020,43(2):130-141. doi: 10.3760/cma.j.issn.1009-9158.2020.02.007 [6] 中华医学会核医学分会,中华医学会心血管病学分会. 核素心肌显像临床应用指南(2018)[J]. 中华心血管病杂志,2019,47(7):519-527. [7] De Amorim Fernandes F,Peix A,Giubbini R,et al. Reproducibility of global LV function and dyssynchrony parameters derived from phase analysis of gated myocardial perfusion SPECT:A multicenter comparison with core laboratory setting[J]. Journal of Nuclear Cardiology,2020,27(5):1-10. [8] McDonagh T A,Metra M,Adamo M,et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J,2021,42(36):3599-3726. doi: 10.1093/eurheartj/ehab368 [9] Hung G U,Zou J,He Z,et al. Left-ventricular dyssynchrony in viable myocardium by myocardial perfusion SPECT is predictive of mechanical response to CRT[J]. Ann Nucl Med,2021,35(8):947-954. doi: 10.1007/s12149-021-01632-5 [10] Chen J,Garcia E V,Bax J J,et al. SPECT myocardial perfusion imaging for the assessment of left ventricular mechanical dyssynchrony[J]. J Nucl Cardiol,2011,18(4):685-694. doi: 10.1007/s12350-011-9392-x [11] Fudim M,Dalgaard F,Fathallah M,et al. Mechanical dyssynchrony:How do we measure it,what it means,and what we can do about it[J]. Journal of Nuclear Cardiology,2019,28(5):2174-2184. [12] Van der Veen B J,Al Y I,Ajmone-Marsan N,et al. Ventricular dyssynchrony assessed by gated myocardial perfusion SPECT using a geometrical approach:A feasibility study[J]. Eur J Nucl Med Mol Imaging,2012,39(3):421-429. doi: 10.1007/s00259-011-1991-x [13] Hendriks T,Al A L,Maagdenberg C G,et al. Agreement of 2D transthoracic echocardiography with cardiovascular magnetic resonance imaging after ST-elevation myocardial infarction[J]. Eur J Radiol,2019,114(1):6-13. [14] Schofield R,Menezes L,Underwood S R. Nuclear cardiology:State of the art[J]. Heart,2021,107(12):954-961. doi: 10.1136/heartjnl-2019-315628 [15] Jacobson A F,Narula J,Tijssen J. Analysis of differences in assessment of left ventricular function on echocardiography and nuclear perfusion imaging[J]. The American Journal of Cardiology,2021,156(1):85-92. [16] Pellikka P A,She L,Holly T A,et al. Variability in ejection fraction measured by echocardiography,gated single-photon emission computed tomography,and cardiac magnetic resonance in patients with coronary artery disease and left ventricular dysfunction[J]. JAMA Netw Open,2018,1(4):e181456. doi: 10.1001/jamanetworkopen.2018.1456 [17] Matsuo H,Yoshimura Y,Fujita S,et al. Role of systemic inflammation in functional recovery,dysphagia,and 1-y mortality in heart failure:A prospective cohort study[J]. Nutrition,2021,91(11):111465. [18] Sheriff A,Kayser S,Brunner P,et al. C-reactive protein triggers cell death in ischemic cells[J]. Frontiers in immunology,2021,12(1):273. [19] Collado A,Domingo E,Piqueras L,et al. Primary hypercholesterolemia and development of cardiovascular disorders:Cellular and molecular mechanisms involved in low-grade systemic inflammation and endothelial dysfunction[J]. Int J Biochem Cell Biol,2021,139(10):106066. [20] 芦珊,韩英,丁栗. 血清hs-CRP、cTnI、BNP及PCT联合检测对慢性心力衰竭的临床诊断价值[J]. 热带医学杂志,2021,21(2):193-196. doi: 10.3969/j.issn.1672-3619.2021.02.016 -






 下载:
下载: