Predictive Model of Risk Factors for the Recurrence of Liver Cirrhosis with Pleural Effusion
-
摘要:
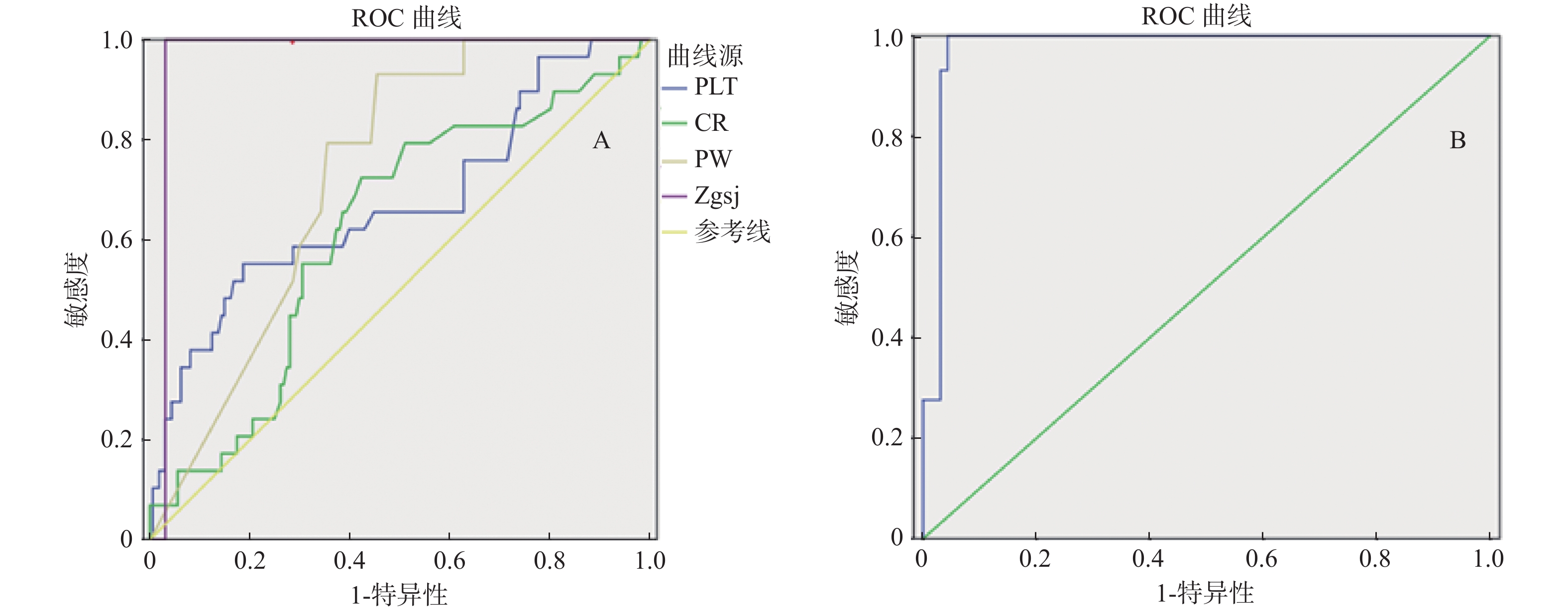
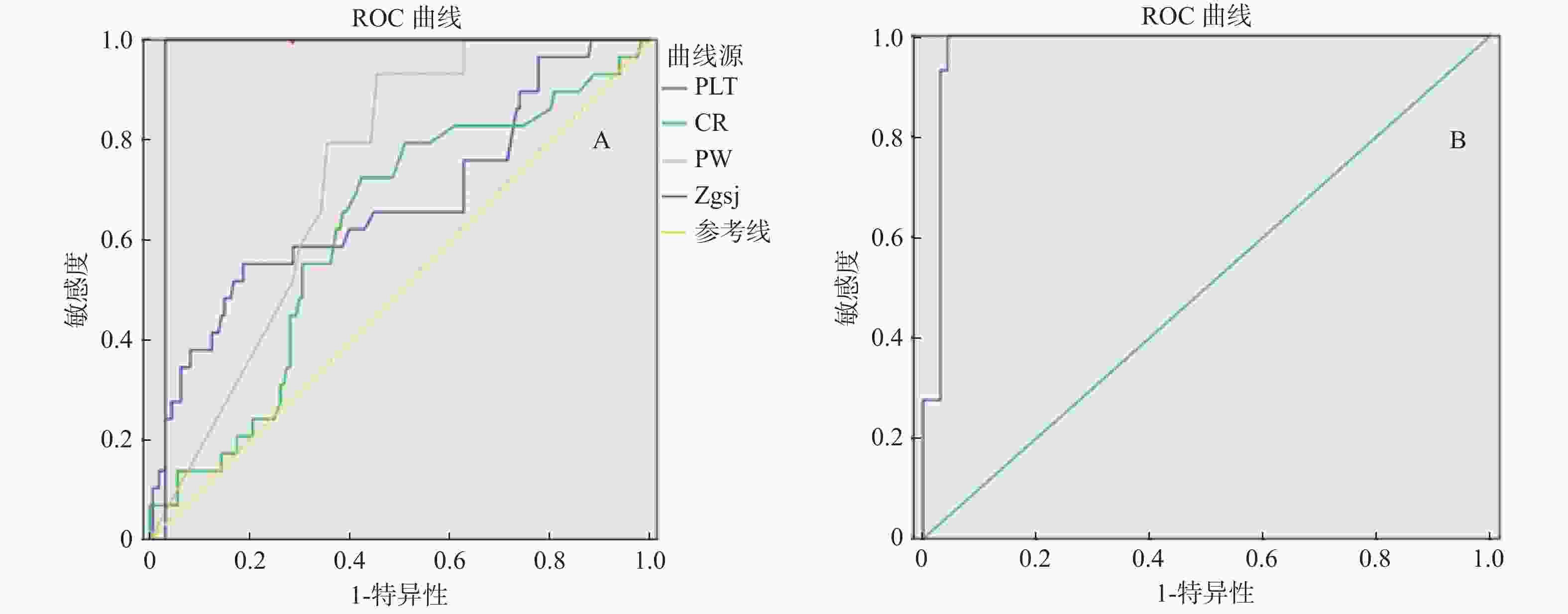
目的 探讨肝硬化合并胸水患者胸水再发的独立危险因素并建立预测模型。 方法 收集2014年4月至2019年12月入住传染科的肝硬化合并大量胸水病例190例,经治疗胸水均消退,随访患者胸水再发情况。将其是否胸水再发分为无胸水再发组(n = 161)和胸水再发组(n = 29),收集2组的性别、年龄、血常规、肝功能、血生化、彩超、置管时间等行Logistic单因素和多因素回归分析,并建立预测模型,绘制AUROC曲线验证模型的敏感性、特异性。 结果 190例患者中,经治疗胸水消失后再发29例(15%),将190例患者基线的年龄、性别、血常规、肝功能等因素行Logistic回归分析,血小板(OR = 1.018,P = 0.028)、血肌酐(OR = 0.978,P = 0.024)、门静脉流速(OR = 0.660,P = 0.048)、置管时间(OR = 1.801,P < 0.001)是肝硬化患者胸水再发的独立危险因素。4个危险因素和模型的AUC分别为:0.673、0.619、0.831、0.969、0.977,模型的敏感性、特异性和正确率分别为89.7%、92.9%、91.8%。 结论 肝硬化合并胸水患者胸水再发预测模型能准确地预测胸水再发风险,对影响因素的早期干预,能减少肝硬化患者胸水再发,并为医务人员及时采取预防性管理措施提供参考。 Abstract:Objective To explore the independent risk factors of the recurrence of pleural effusion in patients with liver cirrhosis and complicated with pleural effusion and to establish a predictive model. Methods 190 cases of liver cirrhosis complicated with massive pleural effusion and admitted to the department of infectious diseases from April 2014 to December 2019 were inquired. The recurrence of pleural effusion after the treatment was followed up, and the relevant clinical data and laboratory indexes were collected. The patients were divided into non pleural effusion recurrence group (n = 161) and pleural effusion recurrence group (n = 29) and ROC curve was used to verify the prediction efficiency of the prediction model. Results Among the 190 patients, 29 (15%) recurred after the disappearance of pleural effusion after the treatment. The factors such as baseline age, gender, blood routine and liver function of 190 patients were analyzed by logistic regression. Platelet (or = 1.018), blood creatinine (or = 0.978), portal vein velocity (or = 0.660) and catheterization time (or = 1.801) were independent risk factors for the recurrence of pleural effusion in patients with liver cirrhosis. The AUC of the four risk factors and the model were 0.673, 0.619, 0.831, 0.969 and 0.977 respectively. The sensitivity, specificity and accuracy of the model were 89.7%, 92.9% and 91.8% respectively. Conclusion The prediction model of pleural effusion recurrence in patients with liver cirrhosis and combined with pleural effusion could better predict the risk of pleural effusion recurrence.Early intervention of influencing factors could reduce the recurrence of pleural effusion in patients with liver cirrhosis, and provide the reference for medical staff to take the preventive management measures in time. -
Key words:
- Liver cirrhosis /
- Recurrence of pleural effusion /
- Risk factors /
- Prediction model
-
表 1 190例肝硬化失代偿期患者一般资料(
$\bar{x}\pm s$ )Table 1. General data of 190 patients with decompensated liver cirrhosis (
$\bar{x}\pm s$ )一般指标 ( $\bar x \pm s $) 年龄 (岁) 52.8 ± 12.16 住院天数 (d) 26.39 ± 11.97 总胆红素(µmmol/L) 56.98 ± 5.28 门冬氨酸氨基转移酶 (U/L) 61.21 ± 4.46 丙氨酸氨基转移酶 (U/L) 31.61 ± 3.97 谷氨酰转肽酶 (U/L) 85.32 ± 9.95 总蛋白(g/L) 62.35 ± 11.79 胸水总蛋白(g/L) 25.24 ± 2.09 前白蛋白(mg/L) 78.22 ± 12.65 白蛋白(g/L) 28.44 ± 6.32 血红蛋白(g/L) 97.45 ± 33.27 血小板(×109/L) 112.21 ± 7.84 凝血酶原时间(S) 25.26 ± 1.78 血肌酐(µmol/L) 105.27 ± 7.54 空腹血糖(mmol/L) 6.56 ± 2.57 胰岛素 (pmol/L) 115.21 ± 36.15 C肽 (nmol/L) 1.47 ± 0.59 门静脉内径(mm) 13.56 ± 1.30 门静脉流速(cm/s) 14.24 ± 3.98 置管时间 (d) 10.70 ± 7.44 脾脏长度 (cm) 174.90 ± 16.00 脾脏厚度(cm) 53.82 ± 8.33 脾静脉内径(mm) 8.75 ± 1.43 白细胞(×109/L) 5.15 ± 3.73 表 2 190例肝硬化失代偿期胸水再发单因素分析(
$\bar{x}\pm s$ )Table 2. Single factor analysis of 190 cases of pleural effusion in decompensated stage of liver cirrhosis (
$\bar{x}\pm s$ )一般指标 胸水再发(n = 29) 胸水未发(n = 161) t P 年龄(岁) 52.21 ± 11.73 52.91 ± 12.27 0.285 0.776 住院天数(d) 30.45 ± 17.23 25.60 ± 10.39 −2.011 0.046* 总胆红素(µmmol/L) 34.87 ± 4.57 60.96 ± 6.13 1.787 0.076 门冬氨酸氨基转移酶(U/L) 55.52 ± 17.41 62.24 ± 16.61 0.615 0.540 丙氨酸氨基转移酶(U/L) 31.61 ± 8.25 31.79 ± 9.00 0.240 0.811 谷氨酰转肽酶(U/L) 143.74 ± 42.37 74.89 ± 8.74 −2.538 0.012* 碱性磷酸酶(U/L) 143.11 ± 49.68 30.62 ± 11.25 −4.382 < 0.001* 总蛋白(g/L) 62.55 ± 8.72 62.31 ± 12.29 −0.100 0.921 胸水总蛋白(g/L) 46.76 ± 11.75 21.36 ± 10.04 −4.606 < 0.001* 前白蛋白(mg/L) 91.07 ± 33.82 75.90 ± 34.86 −2.070 0.040* 白蛋白(g/L) 29.17 ± 5.39 28.31 ± 6.48 −0.678 0.499 血红蛋白(g/L) 92.79 ± 25.28 98.28 ± 34.51 0.818 0.415 血小板(×109/L) 193.90 ± 58.68 97.49 ± 49.13 4.661 < 0.001* 凝血酶原时间(S) 42.94 ± 14.27 22.10 ± 13.21 −4.428 < 0.001* 异常凝血酶原(µg/L) 7541.79 ± 1127.71 1409.24 ± 707.37 −2.888 0.004* 血肌酐(µmol/L) 148.48 ± 37.11 79.48 ± 25.77 −2.466 0.015* 空腹血糖(mmol/L) 7.30 ± 3.45 6.42 ± 2.37 −1.696 0.092 胰岛素(pmol/L) 139.73 ± 49.98 110.79 ± 41.51 −2.917 0.004* C肽(nmol/L) 1.77 ± 0.68 1.42 ± 0.56 −3.011 0.003* 门静脉内径(mm) 12.97 ± 1.72 13.66 ± 1.19 2.704 0.007* 门静脉流速(cm/s) 16.95 ± 2.70 13.75 ± 3.99 3.324 0.048* 置管时间(d) 23.38 ± 7.47 8.42 ± 5.53 −14.459 < 0.001* 脾脏长度(cm) 147.17 ± 16.81 148.03 ± 15.91 0.265 0.791 脾脏厚度(cm) 54.66 ± 9.63 53.67 ± 8.10 0.585 0.559 脾静脉内径(mm) 8.93 ± 1.462 8.71 ± 1.42 0.753 0.452 白细胞(×109/L) 4.70 ± 2.30 5.23 ± 3.93 0.717 0.475 *P< 0.05。 表 3 肝硬化失代偿期患者胸水再发Logistic 回归多因素分析结果
Table 3. Results of logistic regression multivariate analysis of recurrent pleural effusion in patients with decompensated liver cirrhosis
危险因素 回归系数 标准误差 WALS P OR 95%C.I. 血小板(×109/L) 0.017 0.008 4.799 0.028 1.018 1.002~1.003 血肌酐(µmol/L) 0.013 0.006 5.101 0.024 0.978 0.975~0.988 门静脉流速(cm/s) 0.415 0.228 3.324 0.048 0.660 0.423~0.832 引流置管时间(d) 0.588 0.155 14.421 < 0.001 1.801 1.329~2.493 常量 −0.873 8.304 0.732 0.392 0.001 − 表 4 曲线下面积
Table 4. Area under curve
检验结果变量 面积 血小板(PLT) 0.673 血肌酐(CR) 0.69 门静脉流速(cm/s) 0.831 置管时间(d) 0.969 预测模型 0.977 -
[1] Gilbert C R,Shojaee S,Maldonado F,et al. Pleural interventions in the management of hepatic hydrothorax[J]. Chest,2022,161(1):276-283. doi: 10.1016/j.chest.2021.08.043 [2] Yoon J H,Kim H J,Jun C H,et al. Various treatment modalities in hepatic hydrothorax:What is safe and effective?[J]. Yonsei Med J,2019,60(10):944-951. doi: 10.3349/ymj.2019.60.10.944 [3] 陈盛鹏,傅世祥,李敏,等. 体位改变辅助治疗右侧肝性胸水1例[J]. 肝脏,2020,25(6):657. doi: 10.3969/j.issn.1008-1704.2020.06.037 [4] Mouelhi L,Daboussi O,Cheffi N,et al. Hepatic hydrothorax:About a hospital serie of 63 cases.[J]. Tunis Med,2016,94(12):867. [5] 聂深钰,时宇,高普均. 难治性肝性胸水的治疗[J]. 中国老年学杂志,2015,35(11):3171-3173. doi: 10.3969/j.issn.1005-9202.2015.11.142 [6] 中华医学会肝病学分会. 肝硬化诊治指南[J]. 临床肝胆病杂志,2019,35(11):2408-2425. doi: 10.3969/j.issn.1001-5256.2019.11.006 [7] 田莉婷,傅琪琳,李兴国,等. 麻芪桂术汤配合西药治疗阳虚水停型肝性胸水临床观察[J]. 陕西中医,2016,37(7):860-861. doi: 10.3969/j.issn.1000-7369.2016.07.048 [8] 叶珣. 漏出性胸腔积液46例临床病因及分析[J]. 中国保健营养,2018,28(17):273. doi: 10.3969/j.issn.1004-7484.2018.17.361 [9] 马陈斌. 肝硬化腹水的临床治疗应用效果观察[J]. 世界最新医学信息文摘(连续型电子期刊),2019,19(27):72-83. [10] Kamath P S,Wiesner R H,Malinchoc M,et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology,2001,33(2):464-470. doi: 10.1053/jhep.2001.22172 [11] 林殿杰,孙洪军,黄琛,等. 胸腔镜对肝性胸水病人的诊断和治疗价值[J]. 中华肝脏病杂志,2002,10(6):462. doi: 10.3760/j.issn:1007-3418.2002.06.022 [12] 李海军,郭志梅,杨新英,等. 不同频次胸腔穿刺抽液及置管引流对肝硬化失代偿期合并顽固性胸水患者的影响[J]. 国际流行病学传染病学杂志,2017,44(2):85-89. doi: 10.3760/cma.j.issn.1673-4149.2017.02.003 [13] 楼良潮,陆文博. 食管癌伴肝硬化的手术治疗[J]. 中国实用医刊,2015,42(12):75-76. doi: 10.3760/cma.j.issn.1674-4756.2015.12.034 [14] 张骏,孙文兵. 肝性胸水[J]. 中国临床医生,2013,41(8):558-559. -





 下载:
下载: