Pathogen Distribution and Antimicrobial Susceptibility of Bacterial Bloodstream Infection in AIDS Patients
-
摘要:
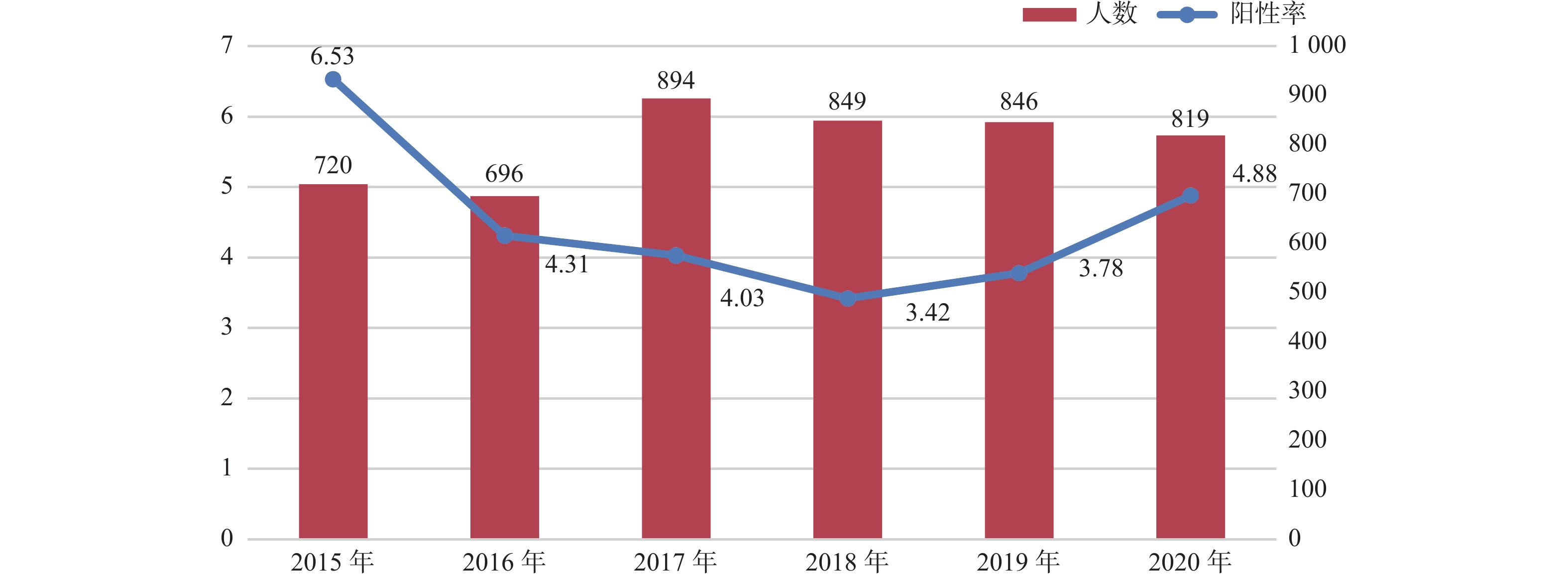
目的 了解艾滋病住院患者细菌血流感染的患病率、病原菌种类及耐药情况。 方法 回顾性收集上海市公共卫生临床中心2015年至2020年血培养分离出细菌的艾滋病患者资料,分析病原菌种类及相应抗菌药物的耐药情况多重耐药的比例。 结果 艾滋病患者中 2015年至2020年间血流感染细菌检出率为4.48%。革兰阳性菌检出128株(59.3%),83株有耐药报告,对青霉素的耐药率为94%,对红霉素的耐药率为91.4%,未检出利奈唑胺、替加环素、万古霉素、喹奴普汀/达福普汀耐药者,多重耐药率38.6%,39.7%的细菌对5类以上抗菌药耐药。革兰阴性菌检出88株(40.7%),70株有耐药报告,对氨苄西林的耐药率为81.6%,喹诺酮类、碳青霉烯类和头孢菌素对革兰阴性菌都有较高的敏感性,多重耐药率14.4%,12.8%的细菌对5类以上抗菌药耐药。 结论 艾滋病合并细菌性血流感染者,革兰阳性菌多重耐药率更高,治疗时可以选择利奈唑胺、替加环素、万古霉素及喹奴普汀/达福普汀。喹诺酮类、碳青霉烯类和头孢菌素对革兰阴性菌较敏感。 Abstract:Objective To explore the prevalence of bacterial bloodstream infection in AIDS patients, and to learn the pathogen species drug resistance among AIDS patients . Methods We retrospectively collected the data of AIDS patients with bacteria isolated from blood culture in Shanghai Public Health Clinical Center from 2015 to 2020. The species of pathogenic bacteria and the antibiotic resistance were analyzed, and the proportion of multiple resistance was also calculated. Results The positive rate of bacteria in bloodstream between 2015 and 2020 was 4.48% in AIDS patients. 128 strains (59.3%) of gram-positive bacteria were detected, 83 strains were reported to be resistant to penicillin, and the resistance rate to erythromycin was 94% and 91.4% No Linezolide, Tigecycline, Vancomycin, Quinolputin/ Dapoptine resistance were detected. The multiple drug resistance rate was 38.6%, and 39.7% of the bacteria were resistant to more than 5 classes of antibiotics. Gram-negative bacteria were detected in 88 patients (40.7%), and drug resistance was reported in 70 patients , the resistance rate to Ampicillin was 81.6%. Quinolones, Carbopenems and Cephalosperins all had high sensitivity to gram-negative bacteria. The multiple drug resistance rate was 14.4%, and 12.8% of the bacteria were resistant to more than 5 classes of antibiotics. Conclusions For AIDS patients with bacterial blood flow infection, the multiple drug resistance rate of gram-positive bacteria is higher, linezolid, tigecycline, vancomycin and quinuptine/daphoputin can be selected for treatment . Quinolones, Carbopenems, and Cephalosperins all have high sensitivity to gram-negative bacteria. -
Key words:
- HIV /
- AIDS /
- Bloodstream infection /
- Bacterium /
- Drug sensitivity
-
表 1 2015-2020年血培养检出细菌的艾滋病患者基本情况[n(%)]
Table 1. Basic information of AIDS patients with bacteria detected in blood cultures from 2015 to 2020 [n(%)]
项目 2015年(n = 45) 2016年(n = 30) 2017年(n = 34) 2018年(n = 29) 2019年(n = 30) 2020年(n = 39) 年龄(岁) 44.4 ± 15.84 42.3 ± 15.3 45.3 ± 12.9 39.3 ± 13.2 45.2 ± 14.9 48.9 ± 18.8 性别 男 42(93.3) 26(86.7) 32(94.1) 28(96.6) 27(90) 37(94.9) 女 3(6.7) 4(13.3) 2(5.9) 1(3.4) 3(10) 2(5.1) CD4(个/μL) 35(13,151) 32(9.5,134) 37.5(9,164.7) 20(3.5,146.2) 40(13,165) 84(10.5,274) 白细胞(×109/L) 5.3(3.8,8.6) 5.2(3.8,8.4) 4.9(3.7,8.6) 3.9(2.9,7.9) 6.27(3.2,9.1) 5.4(2.7,10.2) 中性粒细胞(×109/L) 3.5(.1,4.9) 3.4(1.9,6.8) 3.6(2.6,5.9) 3.3(2.2,6.6) 4.8(2.1,8.2) 4.1(2.0,8.5) 血红蛋白(g/L) 101(84,115) 112(98,128) 109(78,121) 91(69,107) 113(91,128) 102(81,119) 白蛋白(g/L) 30(16.2,36.3) 34.6(26.2,38.4) 30.3(25.2,34.6) 28.8(24.7,32.7) 32.9(28.4,35.6) 30.6(27,34.9) C反应蛋白(mg/L) 26(9.7,112.5) 27.9(7.2,126.2) 30(7,98) 78.6(32.2,124.0) 53.6(10.5,131.5) 63(19.8,110.8) 降钙素原( ng/mL) 0.19(0.07,0.8) 0.37(0.06,1.6) 0.17(0.07,1.1) 0.58(0.1,1.9) 0.35(0.14,0.71) 0.4(0.2,1.56) 表 2 2015-2020年艾滋病住院患者中血培养细菌构成情况[n(%)]
Table 2. Composition of blood culture bacteria in AIDS inpatients from 2015 to 2020 [n(%)]
病原菌 2015年
(n = 720)2016年
(n = 696)2017年
(n = 894)2018年
(n = 849)2019年
(n = 846)2020年
(n = 819)革兰阳性菌(n = 128) 表皮葡萄球菌 (n = 21) 4(0.56) 2(0.29) 3(0.34) 3(0.35) 4(0.47) 5(0.61) 凝固酶阴性葡萄球菌 (n = 18) 8(1.11) 5(0.72) 2(0.22) 2(0.23) 1(0.12) 0(0) 溶血葡萄球菌 (n = 15) 5(0.69) 1(0.14) 1(0.11) 3(0.35) 2(0.24) 3(0.37) 人葡萄球菌 (n = 17) 3(0.42) 3(0.43) 1(0.11) 2(0.23) 1(0.12) 7(0.85) 金黄色葡萄球菌 (n = 14) 4(0.56) 0(0) 3(0.34) 3(0.35) 1(0.12) 3(0.37) 头状葡萄球菌 (n = 9) 0(0) 2(0.29) 3(0.34) 0(0) 2(0.24) 2(0.24) 链球菌属(n = 9) 2(0.28) 2(0.29) 2(0.22) 0(0) 2(0.24) 1(0.12) 其他少见G+菌(n = 25) 8(1.11) 4(0.57) 5(0.56) 1(0.12) 3(0.35) 4(0.49) 革兰阴性菌(n = 88) 沙门菌属 (n = 24) 3(0.42) 3(0.43) 5(0.56) 6(0.71) 4(0.47) 3(0.37) 大肠埃希菌 (n = 19) 3(0.42) 4(0.57) 2(0.22) 3(0.35) 3(0.35) 4(0.49) 肺炎克雷伯杆菌 (n = 12) 3(0.42) 0(0) 3(0.34) 0(0) 5(0.59) 1(0.12) 铜绿假单胞菌 (n = 10) 1(0.14) 0(0) 1(0.11) 2(0.23) 4(0.47) 2(0.24) 鲍曼不动杆菌 (n = 4) 1(0.14) 0(0) 1(0.11) 0(0) 0(0) 2(0.24) 其他少见G-菌(n = 19) 2(0.28) 4(0.57) 5(0.56) 4(0.47) 1(0.12) 3(0.37) 表 3 2015-2020年艾滋病住院患者血培养革兰阳性细菌耐药情况 [n(%)]
Table 3. Drug resistance of Gram-positive bacteria in blood culture of AIDS inpatients from 2015 to 2020 [n(%)]
革兰阳性细菌 克林霉素 环丙沙星 莫西沙星 左氧氟沙星 红霉素 青霉素G 庆大霉素 四环素 苯唑西林 利福平 SMZ 表皮葡萄球菌 n = 15 n = 14 n = 12 n = 14 n = 15 n = 13 n-14 n = 14 n = 14 n = 13 n = 12 S 3(20) 4(28.6) 4(33.3) 4(28.6) 0(0) 0(0) 6(42.8) 9(64.3) 2(14.3) 7(53.8) 2(16.7) I 0(0) 9(64.3) 1(8.3) 1(7.1) 0(0) 0(0) 3(21.4) 0(0) 0(0) 0(0) 0(0) R 12(80) 1(7.1) 7(58.3) 9(64.3) 15(100) 13(100) 5(35.7) 5(35.7) 12(85.7) 6(46.1) 10(83.3) 金黄色葡萄球菌 n = 14 n = 14 n = 9 n = 12 n = 13 n = 12 n = 14 n = 13 n = 13 n = 13 n = 13 S 5(35.7) 10(71.4) 8(88.9) 11(91.7) 3(23.1) 1(8.3) 12(85.7) 9(69.2) 9(69.2) 12(92.3) 8(61.5) I 0(0) 1(7.1) 0(0) 0(0) 0(0) 0(0) 1(7.1) 0(0) 0(0) 0(0) 0(0) R 9(64.3) 3(21.4) 1(11.1) 1(8.3) 10(76.9) 11(91.7) 1(7.1) 4(30.7) 4(30.8) 1(7.7) 5(38.5) 溶血葡萄球菌 n = 13 n = 13 n = 12 n = 13 n = 13 n = 13 n = 12 n = 12 n = 13 n = 12 n = 12 S 3(23.1) 1(7.7) 1(7.7) 1(7.7) 0(0) 1(7.7) 3(25) 10(83.3) 1(7.7) 7(58.3) 5(41.7) I 0(0) 0(0) 4(30.8) 0(0) 0(0) 0(0) 1(8.3) 0(0) 0(0) 0(0) 0(0) R 10(76.9) 12(92.3) 7(53.8) 12(92.3) 13(100) 12(92.3) 8(66.7) 2(16.6) 12(92.3) 5(41.7) 7(58.3) 人葡萄球菌 n = 14 n = 14 n = 14 n = 14 n = 14 n = 12 n = 13 n = 14 n = 14 n = 14 n = 14 S 2(14.3) 3(21.4) 3(21.4) 3(21.4) 1(7.1) 0(0) 12(92.3) 5(35.7) 3(21.4) 10(71.4) 4(28.6) I 1(7.1) 2(14.3) 3(21.4) 1(7.1) 0(0) 0(9) 1(7.7) 0(0) 0(0) 0(0) 0(0) R 11(78.6) 9(64.3) 8(57.1) 10(71.4) 13(92.9) 12(100) 0(0) 9(64.3) 11(78.6) 4(28.6) 10(71.4) 头状葡萄球菌 n = 8 n = 8 n = 7 n = 7 nN=8 n = 7 n = 8 n = 8 n = 8 n = 8 n = 8 S 6(75) 5(62.5) 4(57.1) 4(57.1) 2(25) 0(0) 7(87.5) 6(75) 5(62.5) 6(75) 6(75) I 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) R 2(25) 3(37.5) 3(42.8) 3(42.8) 6(75) 7(100) 1(12.5) 2(25) 3(37.5) 2(25) 2(25) 注:S:敏感,I:中介,R:耐药。 表 4 2015~2020年艾滋病住院患者血培养革兰阴性细菌耐药情况[n(%)]
Table 4. Drug resistance of Gram-negative bacteria in blood culture of AIDS inpatients from 2015 to 2020 [n(%)]
革兰阴性细菌 环丙沙星 左氧氟沙星 庆大霉素 氨苄西林 头孢曲松 头孢他啶 头孢比肟 氨曲南 阿米卡星 亚胺培南 美罗培南 大肠埃希菌 n = 17 n = 18 n = 18 n = 18 n = 18 n = 18 n = 15 n = 18 n = 17 n = 17 n = 5 S 6(35.3) 6(33.3) 13(72.2) 2(11.1) 5(27.8) 15(83.3) 13(86.7) 13(72.2) 17(100) 17(100) 5(100) I 0(0) 2(11.1) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) R 11(64.7) 10(55.6) 5(27.8) 16(88.9) 13(72.2) 3(16.7) 2(13.3) 5(27.8) 0(0) 0(0) 0(0) 沙门菌属 n = 12 n = 4 - n = 15 n = 11 n = 11 n = 1 n = 1 - n = 1 - S 6(50) 1(25) - 3(20) 10(90.9) 10(90.9) 1(100) 1(100) - 1(100) - I 6(50) 3(75) - 0(0) 0(0) 0(0) 0(0) 0(0) - 0(0) - R 0(0) 0(0) - 12(80) 1(9.1) 1(9.1) 0(0) 0(0) - 0(0) - 肺炎克雷伯杆菌 n = 11 n = 11 n = 11 n = 7 n = 11 n = 11 n = 11 n = 11 n = 11 n = 11 n = 5 S 5(45.4) 6(54.5) 6(54.5) 0(0) 5(45.5) 6(54.5) 6(54.5) 6(54.5) 8(72.7) 8(72.7) 3(60) I 1(9.2) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) R 5(45.4) 5(45.5) 5(45.5) 7(100) 6(54.5) 5(45.5) 5(45.5) 5(45.5) 3(27.3) 3(27.3) 2(40) 铜绿假单胞菌 n = 6 n = 6 n = 7 n = 2 n = 2 n = 6 n = 6 n = 4 n = 6 n = 6 n = 2 S 6(100) 5(83.3) 6(85.7) 0(0) 0(0) 5(83.3) 6(100) 3(75) 6(100) 5(83.3) 2(100) I 0(0) 1(16.7) 0(0) 0(0) 0(0) 1(16.7) 0(0) 0(0) 0(0) 0(0) 0(0) R 0(0) 0(0) 1(14.3) 2(100) 2(100) 0(0) 0(0) 1(25) 0(0) 1(16.7) 0(0) 鲍曼不动杆菌 n = 2 n = 3 n = 3 n = 2 n = 3 n = 2 n = 3 n = 1 n = 1 n = 3 n = 2 S 1(50) 1(33.3) 1(33.3) 0(0) 0(0) 1(50) 1(33.3) 0(0) 0(0) 1(33.3) 1(50) I 0(0) 1(33.3) 0(0) (0) 1(33.3) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) R 1(50) 1(33.3) 2(66.7) 2(100) 2(66.7) 1(50) 2(66.7) 1(100) 1(100) 2(66.7) 1(50) 注:S:敏感,I:中介,R:耐药。 表 5 2015-2020年艾滋病住院患者血培养细菌多重耐药情况[n(%)]
Table 5. Multiple drug resistance of blood culture bacteria of AIDS inpatients from 2015 to 2020 [n(%)]
细菌 R0 R1 R2 R3 R4 R5 ≥R6 革兰阳性菌(n = 83) 表皮葡萄球菌(n = 15) 0(0) 0(0) 0(0) 4(26.7) 1(6.6) 3(20) 7(46.7) 人葡萄球菌(n = 14) 0(0) 0(0) 1(7.1) 0(0) 4(28.6) 2(14.3) 7(50) 金黄色葡萄球(n = 14) 0(0) 2(14.3) 4(28.6) 1(7.1) 4(28.6) 2(14.3) 1(7.1) 溶血葡萄球菌(n = 13) 0(0) 0(0) 1(7.7) 0(0) 4(30.8) 1(7.7) 7(53.8) 头状葡萄球菌(n = 8) 0(0) 1(12.5) 4(50) 0(0) 1(12.5) 0(0) 2(25) 链球菌属(n = 6) 0(0) 1(16.7) 1(16.7) 3(50) 1(16.7) 0(0) 0(0) 其他少见G+(n = 13) 1(7.6) 1(7.6) 3(23.1) 1(7.6) 2(15.5) 0(0) 1(7.6) 革兰阴性菌(n = 70) 沙门菌属(n = 21) 7(33.3) 13(61.9) 1(4.8) 0(0) 0(0) 0(0) 0(0) 大肠埃希菌(n = 18) 1(5.6) 5(27.8) 2(11.1) 7(38.9) 3(16.6) 0(0) 0(0) 肺炎克雷伯杆菌(n = 11) 4(36.4) 1(9.1) 1(9.1) 0(0) 1(9.1) 1(9.1) 3(27.2) 铜绿假单胞菌(n = 7) 4(57.1) 0(0) 2(28.6) 0(0) 0(0) 1(14.3) 0(0) 鲍曼不动杆菌(n = 3) 1(33.3) 0(0) 0(0) 0(0) 0(0) 1(33.3) 1(33.3) 其他少见G-菌(n = 10) 3(30) 2(20) 1(10) 2(20) 0(0) 2(20) 0(0) 注:R0:对检测的抗菌药种类都敏感,R1:对1类抗菌药耐药,R2:对2类抗菌药耐药,R3:对3类抗菌药耐药,R4:对4类抗菌药耐药,R5:对5类抗菌药耐药,R6:对6类及以上抗菌药耐药。 -
[1] 杨宗兴,叶荣夏,闫俊,等. 艾滋病合并血流感染病原体种类及耐药分析[J]. 预防医学,2018,30(9):874-878. [2] Archibald L K,McDonald L C,Nwanyanwu O,et al. A hospital-based prevalence survey of bloodstream infections in febrile patients in Malawi:implications for diagnosis and therapy[J]. J Infect Dis,2000,181(4):1414-1420. doi: 10.1086/315367 [3] Ogunsola F T,Arewa D G,Akinsete I E,et al. Aetiology of bacteraemia among adult AIDS patients attending Lagos University Teaching Hospital (LUTH),Lagos,Nigeria[J]. Niger Postgrad Med J,2009,16(3):186-192. [4] 赵贺红,冯萍,肖贵宝,等. 艾滋病合并机会性感染的临床特征和诊疗分析[J]. 华西医学,2011,26(10):1496-1500. [5] B-Lajoie M R,Drouin O,Bartlett G,et al. Incidence and prevalence of opportunistic and other infections and the impact of antiretroviral therapy among HIV-infected children in low- and middle-income countries:A systematic review and meta-analysis[J]. Clin Infect Dis,2016,62(12):1586-1594. doi: 10.1093/cid/ciw139 [6] Kitila K T,Boja D T,Tinsae K M H,et al. Assessment of bacterial profile and antimicrobial resistance pattern of bacterial isolates from blood culture in Addis Ababa Regional Laboratory,Addis Ababa,Ethiopia[J]. Clinical Microbiology,2018,7(312):586-597. [7] Kiertiburanakul S,Watcharatipagorn S,Chongtrakool P,et al. Epidemiology of bloodstream infections and predictive factors of mortality among HIV-infected adult patients in Thailand in the era of highly active antiretroviral therapy[J]. Jpn J Infect Dis,2012,65(1):28-32. doi: 10.7883/yoken.65.28 [8] 肖科,曹汴川,罗瑜,等. 艾滋病合并血流感染病人预后不良的危险因素[J]. 中国艾滋病性病,2019,25(07):691-694. [9] Taramasso L,Tatarelli P,Di Biagio A. Bloodstream infections in HIV-infected patients[J]. Virulence,2016,7(3):320-328. doi: 10.1080/21505594.2016.1158359 [10] 高慧,施理,林锋,等. 艾滋病合并败血症的临床特征与病原菌及耐药性分析[J]. 中华医院感染学杂志,2019,29(23):3544-3547. [11] Sezgin E,Van Natta M L,Thorne J E,et al. Secular trends in opportunistic infections,cancers and mortality in patients with AIDS during the era of modern combination antiretroviral therapy[J]. HIV Med,2018,19(6):411-419. doi: 10.1111/hiv.12609 [12] Manyahi J,Moyo S,Aboud S,et al. High rate of antimicrobial resistance and multiple mutations in the dihydrofolate reductase gene among Streptococcus pneumoniae isolated from HIV-infected adults in a community setting in Tanzania[J]. J Glob Antimicrob Resist,2020,22:749-753. [13] Reda A A,Seyoum B,Yimam J,et al. Antibiotic susceptibility patterns of Salmonella and Shigella isolates in Harar, Eastern Ethiopia[J]. Journal of Infectious Diseases and Immunity,2011(8):6. [14] Gebrekidan A, Dejene T A, Kahsay G, et al. Prevalence and antimicrobial susceptibility patterns of Shigella among acute diarrheal outpatients in Mekelle hospital, Northern Ethiopia[J]. BMC Res Notes, 2015,8(1):1-7.Gebrekidan A,Dejene T A,Kahsay G,et al. Prevalence and antimicrobial susceptibility patterns of Shigella among acute diarrheal outpatients in Mekelle hospital,Northern Ethiopia[J]. BMC Res Notes,2015,8(1):1-7. [15] Belay A,Ashagrie M,Seyoum B,et al. Prevalence of enteric pathogens,intestinal parasites and resistance profile of bacterial isolates among HIV infected and non-infected diarrheic patients in Dessie Town,Northeast Ethiopia[J]. PLoS One,2020,15(12):e243479. [16] 胡丽萍,张志珊,林永年,等. 艾滋病血流感染病原体分布及耐药性分析[J]. 中国艾滋病性病,2020,26(10):1057-1060. [17] 丁秀荣,于艳华,陈铭,等. HIV/AIDS病人合并血流感染的病原菌分布特点[J]. 中国艾滋病性病,2016,22(5):317-319. [18] Jemal M,Deress T,Belachew T,et al. Antimicrobial Resistance Patterns of Bacterial Isolates from Blood Culture among HIV/AIDS Patients at Felege Hiwot Referral Hospital,Northwest Ethiopia[J]. Int J Microbiol,2020,2020:8893266. [19] Gelila A,Brhanu T,Mengistu E,et al. Etiologic agents of bacterial sepsis and their antibiotic susceptibility patterns among patients living with human immunodeficiency virus at Gondar University Teaching Hospital,Northwest Ethiopia[J]. Bio Med Research International,2016,5(23):1-8. -






 下载:
下载: