Clinical Analysis of Cervical Lymph Node Metastatic Squamous Cell Carcinoma of Unknown Primary Site
-
摘要:
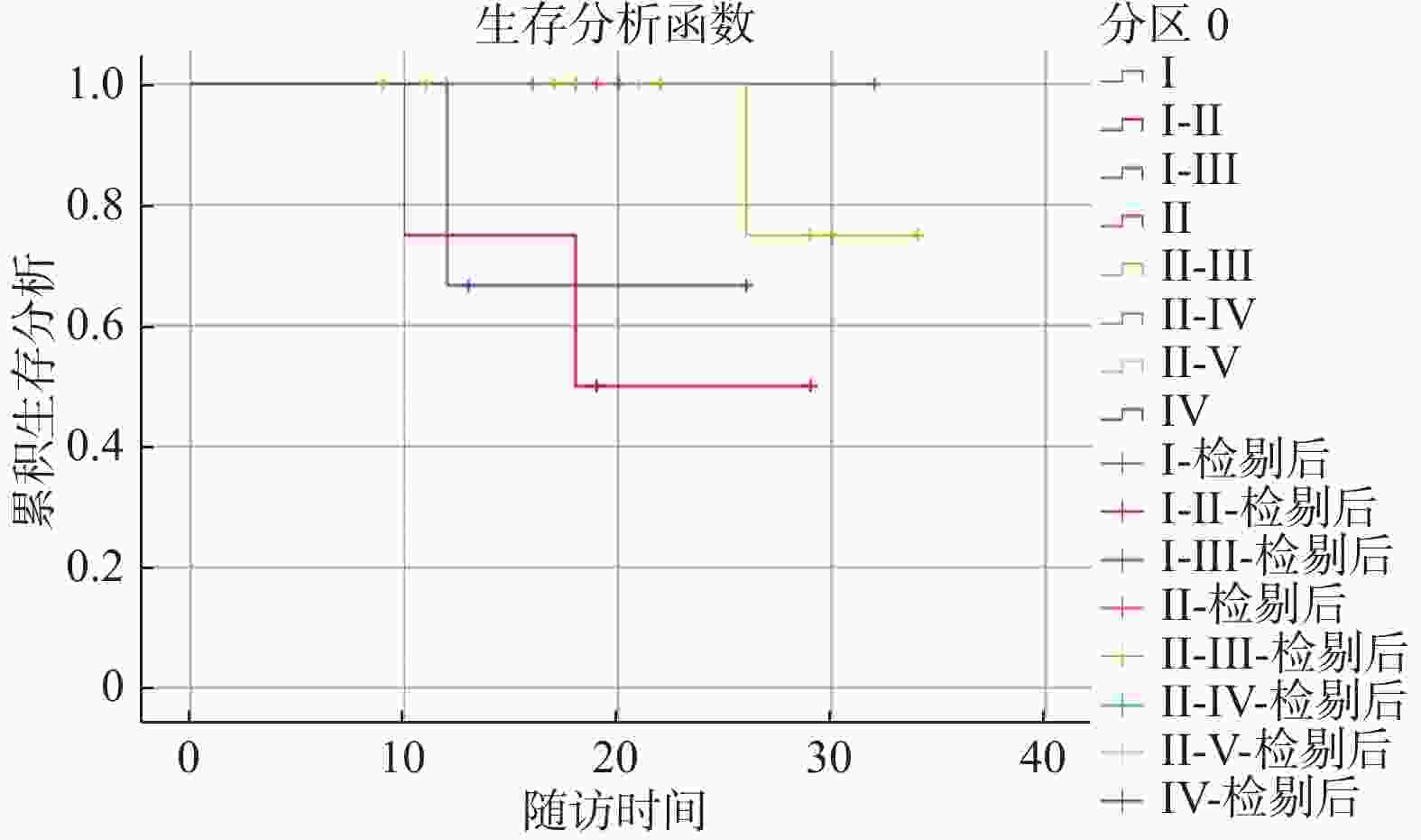
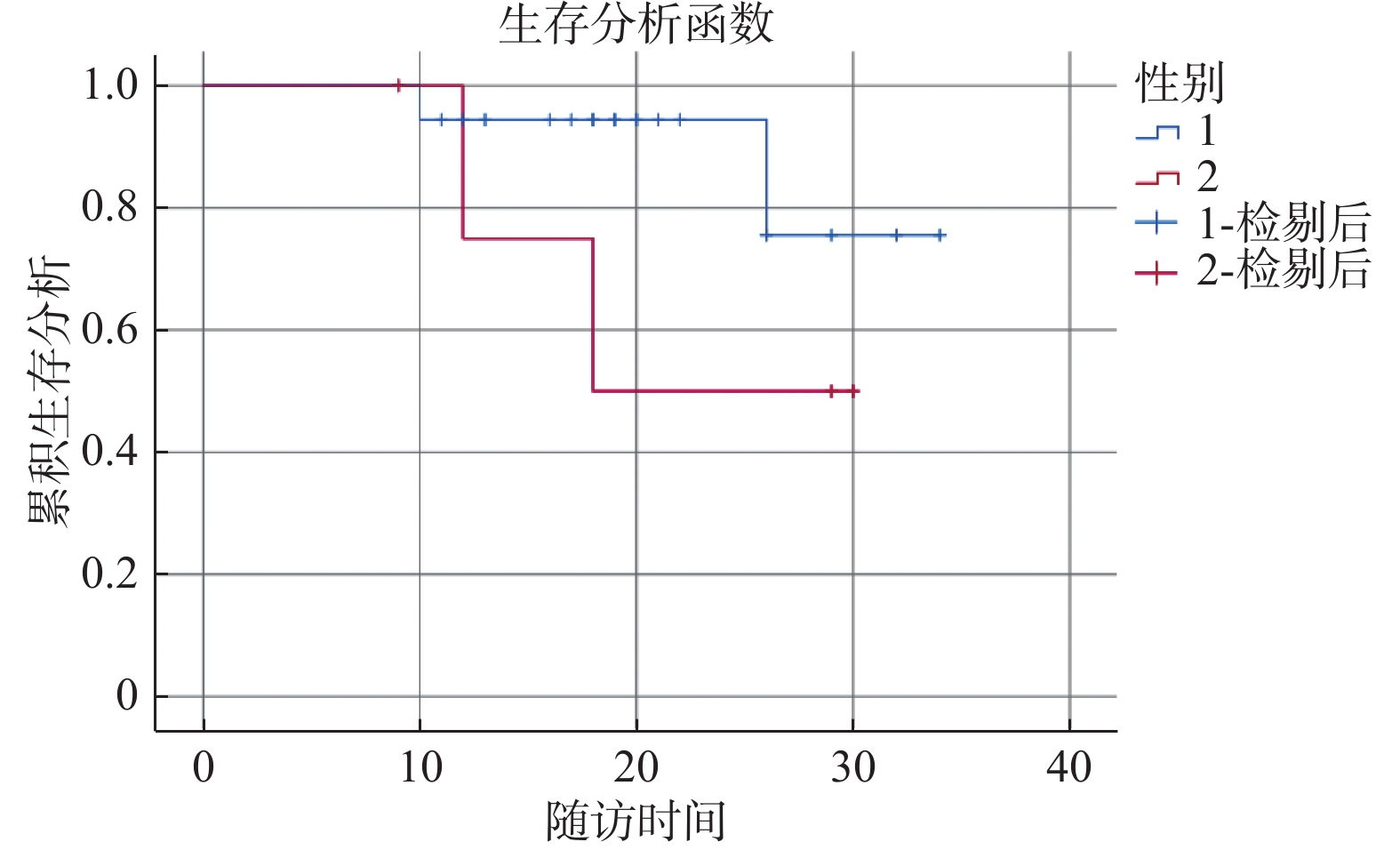
目的 分析原发灶不明颈部淋巴结转移鳞状细胞癌的临床特征,探讨影响预后相关因素,为临床诊治提供依据。 方法 回顾性分析昆明医科大学第一附属医院2018年9月至2020年12月收治的23例原发灶不明的颈部淋巴结转移鳞状细胞癌患者的临床资料,以患者年龄、性别、是否明确原发灶、颈部淋巴结转移区域、肿瘤分期、P16+等作为指标,采用单因素和多因素Cox回归分析方法,分析影响预后因素。 结果 截至随访时间结束,19例生存,4例死亡。患者的生存预后与性别、病程、烟酒史、EBV+、淋巴结转移区域、P16+、是否明确原发灶均无相关性,差异均无统计学意义(P > 0.05),但与患者的年龄相关(P = 0.024 < 0.05)。在N分期中,N分期越后,生存率越低。原发灶不明的生存率较低,有临床意义,但差异无统计学意义(P > 0.05)。 结论 原发灶不明的颈部淋巴结转移鳞状细胞癌患者病程较短,以Ⅱ、Ⅲ区淋巴结受累多见,EBV检测、P16等免疫组织化学染色对寻找原发部位有帮助。针对该类患者,应该根据患者病情选择最佳的诊治方案,从而减少肿瘤复发,提高生存质量。 Abstract:Objective To analyze the clinical characteristics of squamous cell carcinoma with cervical lymph node metastasis of unknown primary (CCUP) focus, explore the prognostic factors, and provide the basis for clinical diagnosis and treatment. Methods The clinical data of 23 patients with CCUP who were admitted to our hospital from September 2018 to December 2020 were reviewed. Lymph node metastasis area, tumor stage, P16+, etc. were used as analysis indicators. Univariate analysis was used to establish Cox risk model to analyze prognostic factors. Results As of the end of follow-up, 19 patients survived and 4 died. There was no correlation between the survival prognosis of patients and the gender, course of disease, history of smoking and alcohol, EBV+, lymph node metastasis area, P16+, and whether the primary tumor was clear, and the difference was not statistically significant (all P > 0.05), but it was related to the age of the patient. Correlation (P = 0.024 < 0.05). In the N stage, the later the N stage, the lower the survival rate. The survival rate of patients with unknown primary tumor was lower and clinically significant, but the difference was not statistically significant. Conclusion The patients with CCUP have a short course of disease, and the level Ⅱ, Ⅲ neck lymph nodes are the most involved. EBV detection, P16 and other immunohistochemical staining are helpful for finding the primary site. The best diagnosis and treatment plan should be selected according to the patient’s condition to reduce tumor recurrence and improve the quality of life. -
Key words:
- Unknown primary tumor /
- Neck metastases /
- Squamous cell carcinoma /
- Prognosis
-
表 1 患者基本临床资料[
$ \bar x \pm s $ /n(%)]Table 1. Basic clinical data of patients [
$ \bar x \pm s $ /n(%)]观察项目 数值 性别 男 18 (78.26) 女 5 (21.74) 年龄(岁) 52.74 ± 13.73 病程(月) 3.69 ± 3.66 烟酒史 有 15 (65.22) 无 8 (34.78) EBV病毒 阳性 9 (39.13) 阴性 14 (60.87) 淋巴结分区 Ⅰ区 1 (4.35) Ⅰ~Ⅱ区 4 (17.39) Ⅰ~Ⅲ区 2 (8.70) Ⅱ区 2 (8.70) Ⅱ~Ⅲ区 9 (39.13) Ⅱ~Ⅳ区 1 (4.35) Ⅱ~Ⅴ区 1(4.35) Ⅳ区 3 (13.04) 免疫组化_P16
阳性
阴性
5 (21.74)
18 (78.26)死亡 存活 19 (82.61) 死亡 4 (17.39) 原发灶 鼻咽癌 5 (21.74) 扁桃体癌 3 (13.05) 喉癌 1 (4.35) 膀胱癌 1 (4.35) 鳃裂囊肿癌 1 (4.35) 舌癌 2 (8.70) 食管癌 2 (8.70) 原发灶不明 8 (34.78) T 0 8 (34.78) 1 13 (59.09) 2 2 (9.09) N 1 1 (4.35) 2a 2 (8.70) 2b 13 (56.52) 2c 7 (30.43) 表 2 单因素分析结果[
$ \bar x \pm s $ /n(%)]Table 2. Results of single factor analysis [
$ \bar x \pm s $ /n(%)]项目 总数 (n = 23) 存活 (n = 19) 死亡 (n = 4) t/Fisher P 性别 0.194 男 18 (78.26) 16 (84.21) 2 (50.00) 女 5 (21.74) 3 (15.79) 2 (50.00) 年龄(岁) 52.74 ± 13.73 49.84 ± 11.50 66.50 ± 16.78 −2.443 0.024 病程(月) 3.69 ± 3.66 3.64 ± 3.39 3.92 ± 5.42 −0.133 0.895 烟酒史 0.589 有 15 (65.22) 13 (68.42) 2 (50.00) 无 8 (34.78) 6 (31.58) 2 (50.00) EBV 1.000 阳性 9 (39.13) 7 (36.84) 2 (50.00) 阴性 14 (60.87) 12 (63.16) 2 (50.00) 淋巴结分区 0.660 Ⅰ区 1 (4.35) 1 (5.26) 0 (0.00) Ⅰ~Ⅱ区 4 (17.39) 2 (10.53) 2 (50.00) Ⅰ~Ⅲ区 2 (8.70) 2 (10.53) 0 (0.00) Ⅱ区 2 (8.70) 2 (10.53) 0 (0.00) Ⅱ~Ⅲ区 9 (39.13) 8 (42.11) 1 (25.00) Ⅱ~Ⅳ区 1 (4.35) 1 (5.26) 0 (0.00) Ⅱ~Ⅴ区 1 (4.35) 1 (5.26) 0 (0.00) Ⅳ区 3 (13.04) 2 (10.53) 1 (25.00) 免疫组化P16 0.194 阳性 5 (21.74) 3 (15.79) 2 (50.00) 阴性 18 (78.26) 16 (84.21) 2 (50.00) 原发灶 1.000 不明 8 (34.78) 7 (36.84) 1 (25.00) 明确 15 (65.22) 12 (63.16) 3 (75.00) 表 3 Cox回归分析结果
Table 3. Results of Cox regression analysis
项目 Estimate Se Z Wald P HR (95%CI) 性别 男 ref 女 1.299 1.006 1.291 1.667 0.197 3.666(0.510,26.351) 年龄 0.099 0.053 1.866 3.482 0.062 1.104(0.995,1.224) 病程 0.062 0.139 0.447 0.200 0.655 1.064(0.811,1.396) 烟酒史 有 ref 无 0.648 1.006 0.645 0.416 0.519 1.912(0.266,13.729) EBV 阳性 ref 阴性 −0.029 1.035 −0.028 0.001 0.978 0.972(0.128,7.386) 淋巴结分区 Ⅰ区 ref Ⅰ~Ⅱ区 20.902 49432.740 0.000 0.000 1.000 1195881363.001 (0.000,Inf) Ⅰ~Ⅲ区 0.067 57045.931 0.000 0.000 1.000 1.069(0.000,Inf) Ⅱ区 0.013 62995.075 0.000 0.000 1.000 1.013(0.000,Inf) Ⅱ~Ⅲ区 19.301 49432.740 0.000 0.000 1.000 241229183.935 (0.000,Inf) Ⅱ~Ⅳ区 0.034 80616.865 0.000 0.000 1.000 1.034(0.000,Inf) Ⅱ~Ⅴ区 0.000 69908.442 0.000 0.000 1.000 1.000(0.000,Inf) Ⅳ区 20.523 49432.740 0.000 0.000 1.000 818550438.604 (0.000,Inf) 免疫组化P16 阳性 ref 阴性 −1.904 1.228 −1.551 2.405 0.121 0.149(0.013,1.653) 原发灶 不明 ref 明确 0.216 1.156 0.187 0.035 0.851 1.242(0.129,11.957) -
[1] Civantos F J,Vermorken J B,Shah J P,et al. Metastatic squamous cell carcinoma to the cervical lymph nodes from an unknown primary cancer:Management in the HPV era[J]. Front Oncol,2020,10:593164. doi: 10.3389/fonc.2020.593164 [2] Ye W,Arnaud E H,Langerman A,et al. Diagnostic approaches to carcinoma of unknown primary of the head and neck[J]. Eur J Cancer Care (Engl),2021,30(6):e13459. [3] Ebisumoto K,Sakai A,Maki D,et al. Tumor detection with transoral use of flexible endoscopy for unknown primary head and neck cancer[J]. Laryngoscope Investig Otolaryngol,2021,6(5):1037-1043. doi: 10.1002/lio2.656 [4] Kennel T,Garrel R,Costes V,et al. Head and neck carcinoma of unknown primary[J]. Eur Ann Otorhinolaryngol Head Neck Dis,2019,136(3):185-192. doi: 10.1016/j.anorl.2019.04.002 [5] Golusinski P,Di Maio P,Pehlivan B,et al. Evidence for the approach to the diagnostic evaluation of squamous cell carcinoma occult primary tumors of the head and neck[J]. Oral Oncol,2019,88:145-152. doi: 10.1016/j.oraloncology.2018.11.020 [6] Kawamoto Y,Ikezawa K,Hasegawa S,et al. Ampullary cancer detected upon re-examination in a patient initially diagnosed as cancer of unknown primary[J]. JGH Open,2022,6(3):222-224. doi: 10.1002/jgh3.12710 [7] Park K S,Lim H R,Jeong S H,et al. Treatment outcomes of patients with head and neck squamous cell carcinoma of unknown primary[J]. Chonnam Med J,2021,57(1):58-61. doi: 10.4068/cmj.2021.57.1.58 [8] Li R,Liao K,Wei Z,et al. The prognostic role of radiotherapy and radiotherapy target in cervical lymph node metastatic squamous cell carcinoma with unknown primary:a retrospective study[J]. J Cancer Res Clin Oncol,2022,148(6):1437-1445. doi: 10.1007/s00432-021-03724-1 [9] Qaseem A,Usman N,Jayaraj J S,et al. Cancer of unknown primary:A review on clinical guidelines in the development and targeted management of patients with the unknown primary site[J]. Cureus,2019,11(9):e5552. [10] Barbosa M,Duarte H,Breda E,et al. PET/CT in the management of metastatic cervical lymphadenopathy from unknown primary site:a seven years retrospective study[J]. Rev Laryngol Otol Rhinol (Bord),2013,134(2):89-94. [11] Szymonowicz K A,Chen J. Biological and clinical aspects of HPV-related cancers[J]. Cancer Biol Med,2020,17(4):864-878. doi: 10.20892/j.issn.2095-3941.2020.0370 [12] Jalaly J B,Hosseini S M,Shafique K,et al. Current status of p16 immunohistochemistry and HPV testing in fine needle aspiration specimens of the head and neck[J]. Acta Cytol,2020,64(1-2):30-39. doi: 10.1159/000496158 [13] Shahoumi L A,Yeudall W A. Targeted therapies for non-HPV-related head and neck cancer:challenges and opportunities in the context of predictive,preventive,and personalized medicine[J]. EPMA J,2019,10(3):291-305. doi: 10.1007/s13167-019-00177-y [14] Tsao S W,Tsang C M,Lo K W. Epstein-Barr virus infection and nasopharyngeal carcinoma[J]. Philos Trans R Soc Lond B Biol Sci,2017,372(1732):20160270. [15] Sprave T,Ruhle A,Hees K,et al. Radiotherapeutic management of cervical lymph node metastases from an unknown primary site - experiences from a large cohort treated with modern radiation techniques[J]. Radiat Oncol,2020,15(1):80. doi: 10.1186/s13014-020-01529-z [16] Wang Y,He S S,Bao Y,et al. Cervical lymph node carcinoma metastasis from unknown primary site:a retrospective analysis of 154 patients[J]. Cancer Med,2018,7(5):1852-1859. doi: 10.1002/cam4.1458 -






 下载:
下载: