Influence of Different Thyroid Surgery Methods on the Function of Parathyroid Glands
-
摘要:
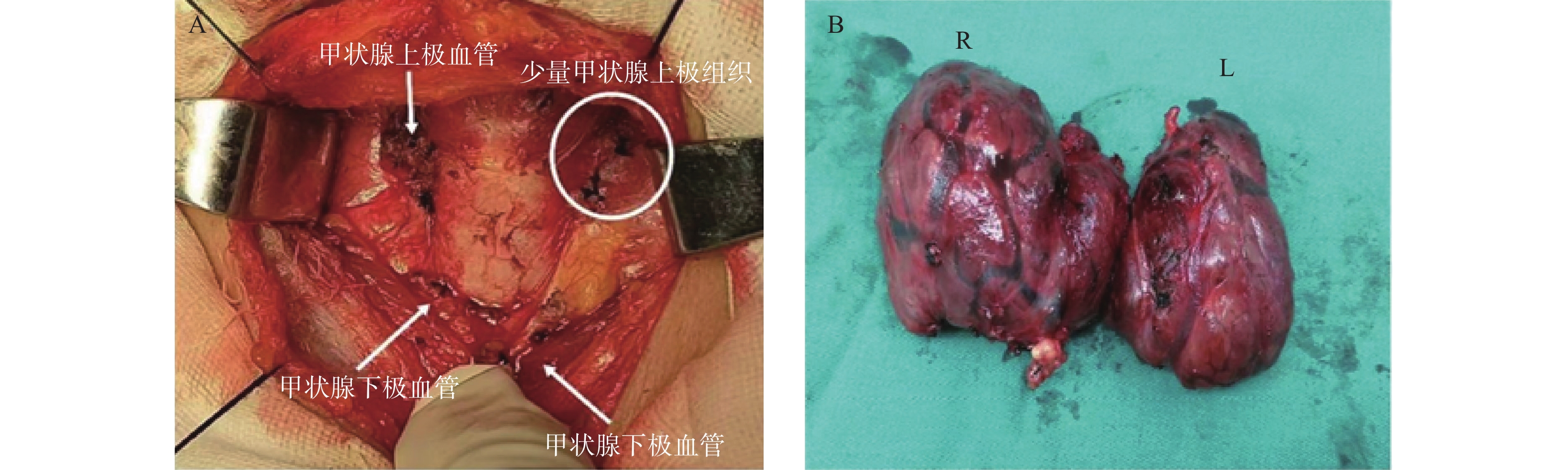
目的 探讨不同甲状腺手术方式对甲状旁腺功能的影响。 方法 分析60例甲状腺手术患者临床资料,行甲状腺次全切除组30例,行甲状腺全切组30例,比较2组患者术前PTH、术后1周PTH水平及PTH下降程度,以及术前血钙含量、术后1周血钙含量及血钙含量下降程度。 结果 2组患者临床资料差异无统计学意义(P > 0.05)。术前2组患者PTH[(46.71±11.52)ng/L比(46.23±11.74)ng/L,P > 0.05]及血钙水平[(1.85±0.47) mmol/L比(1.88±0.39) mmol/L,P > 0.05]比较差异无统计学意义。术后1周,2组患者的PTH及血钙均低于术前,其中全切组PTH[(23.35±6.42)ng/L比(32.18±9.51)ng/L,P < 0.05]及血钙水平[(1.42±0.31)mmol/L比(1.75±0.21)mmol/L,P < 0.05]明显低于次全切除组,PTH[(49.5±5.1%)比(31.1±3.5%),P < 0.05]及血钙水平[(24.5±2.31%)比(5.4±0.5%),P < 0.05]下降程度明显高于次全切除组,术后全切除组患者甲状旁腺病检检出率明显高于次全切组(26.67%比3.33%,P < 0.05)。 结论 不同甲状腺手术方式将导致术后不同程度的甲状旁腺功能减退,甲状腺全切术较甲状腺次全切除术影响显著。 Abstract:Objective To explore the influence of different thyroid surgery methods on the function of parathyroid glands. Methods We analyzed the clinical data of 60 patients undergoing thyroid surgery, including 30 cases in the subtotal thyroidectomy group and 30 cases in the total thyroidectomy group. Then we compared the preoperative PTH, the level of PTH and the degree of decrease in PTH in one week after the operation, as well as the preoperative blood calcium content, the level of blood calcium content and the decrease in blood calcium content one week after the operation. Results No difference was found in preoperative clinical data between the two groups (P > 0.05). There was no significant difference in PTH [(46.71±11.52) ng/L vs(46.23±11.74) ng/L, P > 0.05] and blood calcium levels [(1.85±0.47) mmol/L vs(1.88±0.39) mmol/L, P > 0.05] between the two groups before surgery. One week after the operation, the PTH and blood calcium of the two groups were lower than before the operation. The PTH [(23.35±6.42) ng/L vs (32.18±9.51) ng/L, P < 0.05] and blood calcium levels [(1.42±0.31) mmol/L vs (1.75±0.21)mmol/L, P < 0.05] in the total thyroidectomy group were significantly lower than those in the subtotal thyroidectomy group. The degree of decrease in PTH [(49.5±5.1%) vs (31.1±3.5%), P < 0.05] and blood calcium levels [(24.5±2.31%) vs (5.4±0.5%), P < 0.05] were significantly higher than the subtotal thyroidectomy group. Total thyroidectomy group parathyroid detection rate was significantly higher than the subtotal thyroidectomy group (26.67%比3.33%, P < 0.05). Conclusion Different thyroid surgery methods will lead to different degrees of postoperative hypoparathyroidism, and total thyroidectomy has a more significant impact than subtotal thyroidectomy. -
Key words:
- Thyroid surgery /
- Hypoparathyroidism /
- Hypocalcemia
-
表 1 次全切除组和全切组患者甲状旁腺功能比较(
$\bar x \pm s$ )Table 1. Comparison of the parathyroid function between subtotal thyroidectomy group parathyroid function and total thyroidectomy group (
$\bar x \pm s$ )PTH及血钙 次全切除组(n = 30) 全切组(n = 30) t P 术前PTH(ng/L) 46.71 ± 11.52 46.23 ± 11.74 0.541 0.575 术后PTH(ng/L) 32.18 ± 9.51 23.35 ± 6.42 8.365 0.013* PTH下降程度(%) 31.1 ± 3.5 49.5 ± 5.1 4.651 0.021* 术前血钙(mmol/L) 1.85 ± 0.47 1.88 ± 0.39 0.932 0.353 术后血钙(mmol/L) 1.75 ± 0.21 1.42 ± 0.31 3.832 0.032* 血钙下降程度(%) 5.4 ± 0.5 24.5 ± 2.3 5.735 0.019* *P < 0.05。 表 2 次全切除组和全切组患者甲状旁腺检出率比较[n(%)]
Table 2. Comparison of the parathyroid detection rate between subtotal thyroidectomy group parathyroid detection rate and total thyroidectomy group [n(%)]
组别 n 甲状旁腺检出率 次全切除组 30 1( 3.33) 全切组 30 8(26.67) χ2 57.44 P 0.011* *P < 0.05。 -
[1] Kakava K,Tournis S,Makris K,et al. Identification of patients at high risk for postsurgical hypoparathyroidism[J]. In Vivo,2020,34(5):2973-2980. doi: 10.21873/invivo.12128 [2] Paladino N C,Gu é rin C,Graziani J,et al. Predicting risk factors of postoperative hypocalcemia after total thyroidectomy:is safe discharge without supplementation possible? A large cohort study[J]. Langenbeck Arch Surg,2021,406(7):2425-2431. doi: 10.1007/s00423-021-02237-2 [3] Godlewska P,Benke M,Stachlewska-Nasfeter E,et al. Risk factors of permanent hypoparathyroidism after total thyroidectomy and central neck dissection for papillary thyroid cancer:a prospective study[J]. Endokrynol Pol,2020,71(2):126-133. doi: 10.5603/EP.a2020.0006 [4] 邓汇典. 不同甲状腺手术方式对甲状旁腺功能损伤的影响比较[J]. 当代医学,2020,26(33):179-180. doi: 10.3969/j.issn.1009-4393.2020.33.079 [5] 杨建新. 分析不同手术方式治疗甲状腺癌对甲状旁腺功能的影响[J]. 现代诊断与治疗, 2019, 30(21): 3806-3808. [6] Mehrabi B M,Jangjoo A,Afzal A M,et al. Transient and permanent hypoparathyroidism following thyroidectomy[J]. Minerva Chir,2012,67(5):433-438. [7] Ozbas S,Kocak S,Aydintug S,et al. Comparison of the complications of subtotal, near total and total thyroidectomy in the surgical management of multinodular goitre[J]. Endocr J,2005,52(2):199-205. [8] Yazıcıoğlu M Ö,Yılmaz A,Kocaöz S,Parlak,et al. Risks and prediction of postoperative hypoparathyroidism due to thyroid surgery[J]. Sci Rep,2021,11(1):11876. doi: 10.1038/s41598-021-91277-1 [9] Chahardahmasumi E,Salehidoost R,Amini M,et al. Assessment of the Early and Late Complication after Thyroidectomy[J]. Adv Biomed Res,2019,8:14. doi: 10.4103/abr.abr_3_19 [10] Nawrot I,Woźniewicz B,Tołłoczko T,et al. Allotransplantation of cultured parathyroid progenitor cells withoutimmunosuppression:clinical results[J]. Transplantation,2007,83(6):734-740. doi: 10.1097/01.tp.0000258601.17505.9d [11] 朱精强. 甲状腺手术中甲状旁腺保护专家共识[J]. 中国实用外科杂志,2015,35(7):731-736. [12] 夏恒,刘钊,黄河,等. 甲状腺癌手术中不同手术入路方式对甲状旁腺辨识及功能保护的影响[J]. 全科医学临床与教育,2022,20(3):267-269. [13] 朱国华,邹贤,宋智明,等. 甲状腺不同手术方式对甲状旁腺功能的影响[J]. 中国现代普通外科进展,2014,17(5):342-345. [14] 罗登榜. 甲状旁腺保护技术在甲状腺癌手术中的应用[J]. 医学伦理与实践,2021,34(21):3740-3742. [15] 王登欢,任艳鑫,冯恩梓,等. 经口腔入路甲状腺腔镜手术在治疗甲状腺微小癌的应用价值及美容性效果[J]. 昆明医科大学学报,2020,41(10):119-123. -






 下载:
下载: