Comparison of Frailty Assessment Methods for Predicting Postoperative Complications in Hospitalized Elderly Patients
-
摘要:
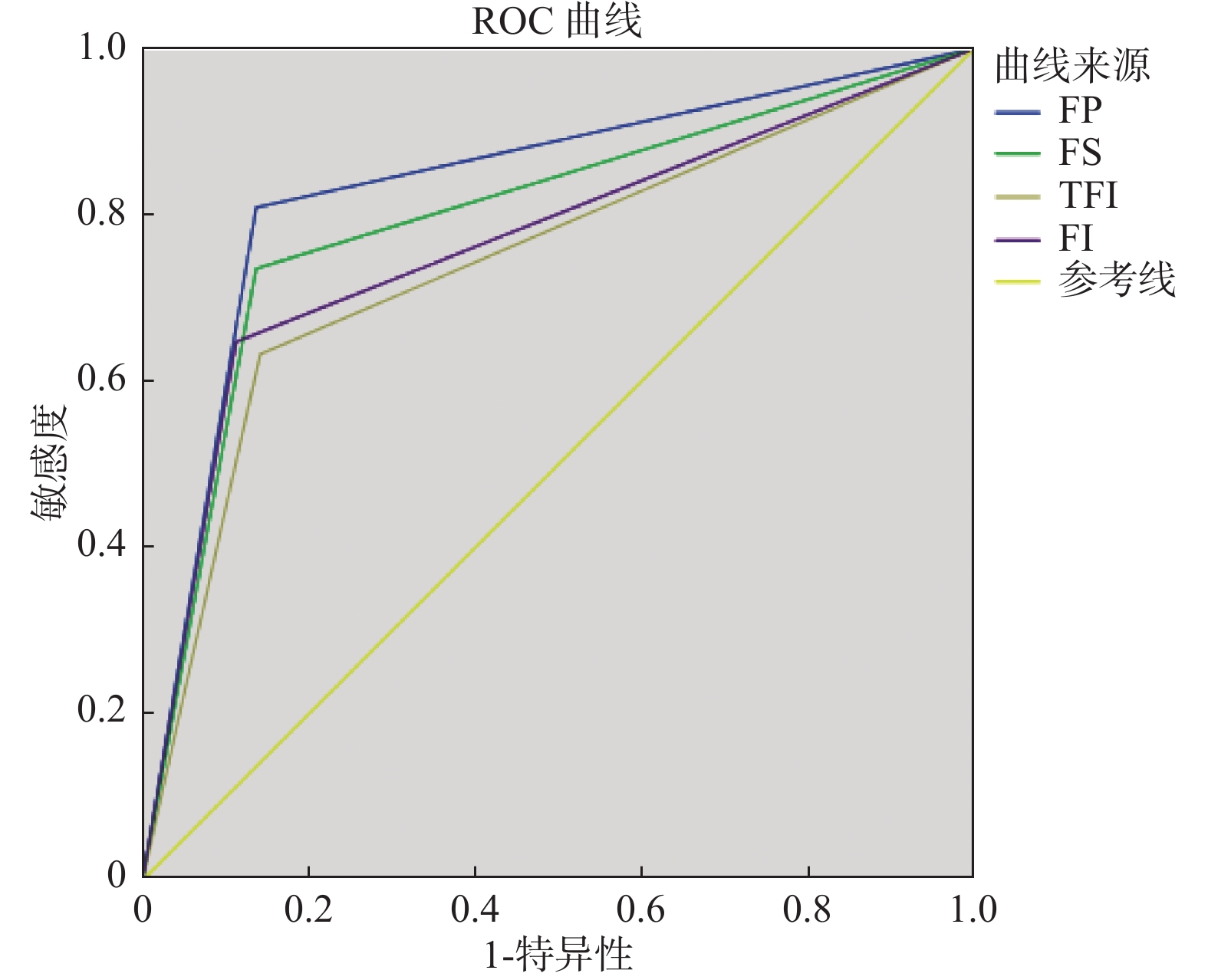
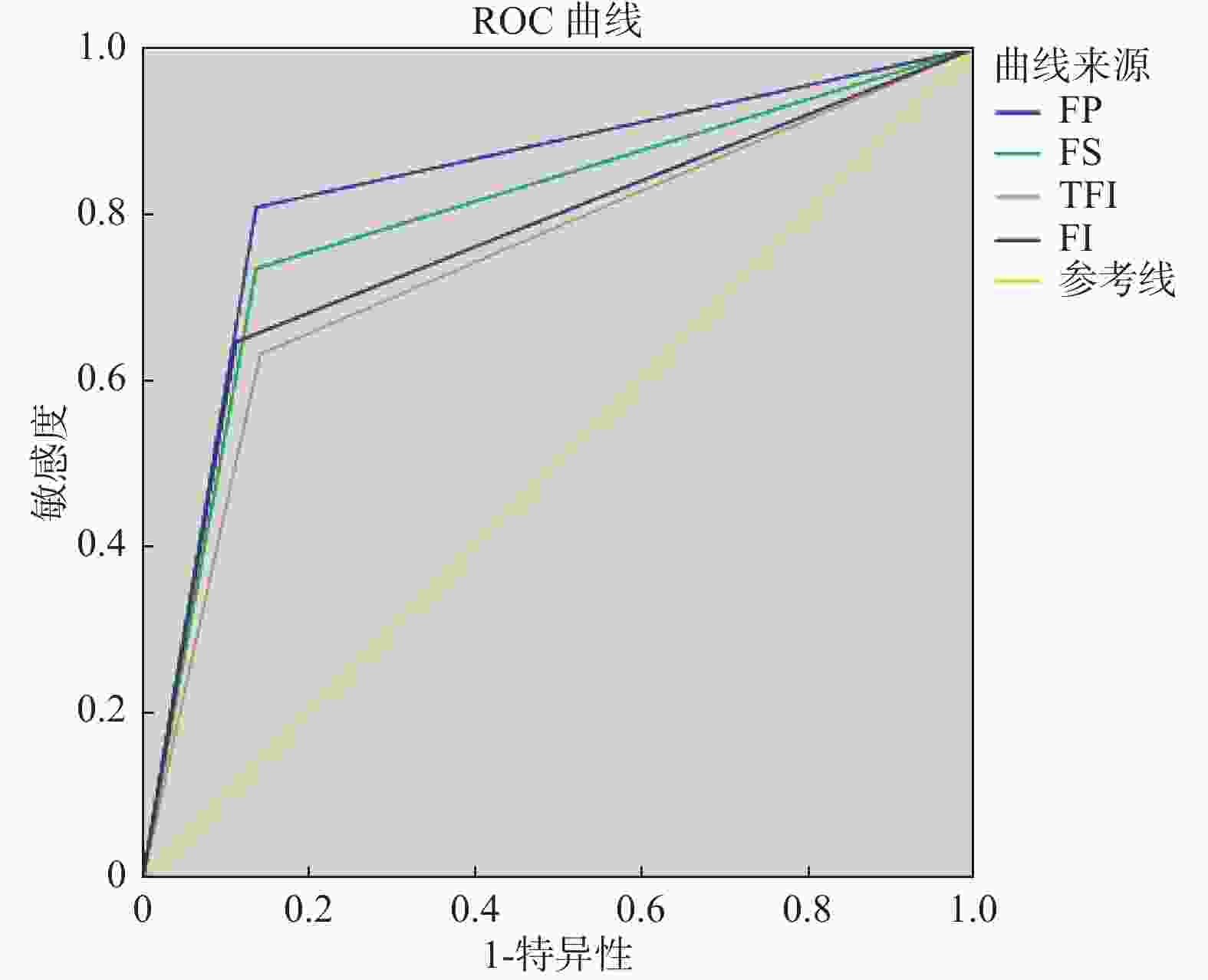
目的 应用FP(frailty phenotype,FP)、FI-CD(frailty index of accumulative deficits,FI-CD)、Frail Scale、TFI(tilburg frailty indicator,TFI) 4种衰弱评估方法对胃肠外科住院老年患者进行衰弱评估,并对其预测术后并发症的能力进行比较。 方法 采用队列研究方法,选取广州市某医院2个院区胃肠外科手术老年患者进行资料收集,包括一般资料、FP、FI-CD、Frail Scale、TFI 、手术时间、出血量、住院期间发生的并发症以及出院30 d内发生的并发症资料等。计算受试者工作特征曲线(receiver operating characteristic,ROC)和曲线下面积(area under the roc curve,AUC), 比较FP、FI-CD、Frail Scale、TFI 4种衰弱评估量表预测术后并发症的能力。 结果 共纳入294位患者资料,21例失访,最终收集到完整资料273例,年龄为60~88(69.49 ± 6.90)岁。采用FP、FI-CD、Frail Scale、TFI 评估检出衰弱的比例分别为30.4 %、24.5%、28.6%、26.4%。经卡方检验,FP、FI-CD 与 Frail Scale(FS)、TFI 评估结果两两比较kappa值分别为0.52、0.60、0.47、0.65、0.54、0.58(P < 0.001),一致性较弱。FP、FI-CD、Frail Scale、TFI 预测术后并发症的AUC分别为0.896[95%CI(0.784,0.929)]、0.767[95%CI(0.706,0.829)]、0.799[95%CI(0.742,0.857)]、0.745[95%CI(0.683,0.808)],(均P < 0.001)。 结论 不同衰弱评估工具对衰弱的检出率差异较大,在临床工作中选取衰弱评估量表时需要慎重。FP、FI-CD、FS、TFI对术后并发症的AUC分别为0.836、0.767、0.799、0.745,FP预测术后并发症的能力强于其他3种衰弱评估工具。 Abstract:Objective To evaluate frailty of surgical elderly hospitalized patients by four kinds of frailty assessment tools, FP (frailty phenotype, FP), FI-CD (frailty index of accumulative deficits, FI-CD), Frail Scale, and TFI (tilburg frailty indicator, TFI), and to compare their ability to predict postoperative complications. Methods A cohort study method was used to select elderly patients undergoing surgical operations in Guangzhou hospitals for data collection, including general information, FP, FI-CD, Frail Scale, TFI, operation time, blood loss, complications during hospitalization, and those occurring within 30 days of discharge Complication information, etc. We calculated the receiver operating characteristic curve (ROC) and area under the ROC curve (AUC), and compared the ability of FP, FI-CD, Frail Scale, and TFI to predict postoperative complications. Results A total of 294 patients were included, 21 cases were lost to follow-up, and 273 patients with complete data were finally collected, aged 60-88 (69.49 ± 6.90) years old. The percentages of frailty detected by FP, FI-CD, Frail Scale, and TFI were 30.4%, 24.5%, 28.6%, and 26.4%, respectively. After chi-square test, the kappa values of FP, FI-CD and Frail Scale (FS) and TFI evaluation results were 0.52, 0.60, 0.47, 0.65, 0.54, 0.58, respectively (P < 0.001), and the consistency was weak. The AUC of FP, FI-CD, Frail Scale, and TFI predicting postoperative complications were 0.896 [95% CI (0.784, 0.929)], 0.767 [95% CI (0.706, 0.829)], 0.799 [95% CI (0.742), respectively , 0.857)], 0.745 [95%CI (0.683, 0.808)], (all P < 0.05). Conclusions Different frailty assessment tools have great differences in the detection rate of frailty, and caution should be exercised when selecting frailty assessment methods in clinical work. AUC for FP, FI-CD, FS, and TFI for postoperative complications are 0.836, 0.767, 0.799, and 0.745, respectively. The ability of FP to predict postoperative complications is better than the other three assessment tools. -
Key words:
- Elderly /
- Frailty assessment /
- Complication /
- Frailty
-
表 1 研究对象的人口统计学基本情况(n = 273)
Table 1. Basic demographics of the study subjects (n = 273)
变量 n 百分比(%) 年龄(岁) 60~69 152 55.7 70~79 95 34.8 ≥80 26 9.5 性别 男 142 52.0 女 131 48.0 文化程度 文盲 52 19.0 初小 151 55.3 中学 46 16.8 大专及以上 24 8.8 医疗费支付形式 公费医疗 15 5.5 城镇居民/居民医疗保险 129 47.3 新农合 123 45.1 自费 6 2.2 已确诊慢性病的种类 没有 25 9.2 1种 83 30.4 2种 63 23.1 3种 36 13.2 4种及以上 66 24.2 高血压 无 214 78.4 有 59 21.6 糖尿病 无 216 79.1 有 57 20.9 表 2 患者实验室检查及应用FP、FI-CD、FS、TFI评估衰弱情况[(
$ \bar{x} \pm s $ )/n(%)]Table 2. Laboratory examination of patients and assessment of frailty with FP,FI-CD,FS,and TFI [(
$ \bar{x} \pm s $ )/n(%)]项目 检出率
(%)年龄
(岁)共病数量 血红蛋白
(g/L)白蛋白
(g/L)手术时间
(h)出血量
(mL)住院时间
(d)住院费用
(万元)并发症发生
例数FP 无衰弱(n = 190) 69.6 67.9 ± 5.9 3.1 ± 1.3 121.7 ± 8.8 38.2 ± 3.1 4.4 ± 0.3 22.6 ± 8.0 17.9 ± 1.9 7.3 ± 0.5 13(6.8) 衰弱(n = 83) 30.4 73.1 ± 7.7 3.1 ± 1.4 114.1 ± 12.8 34.0 ± 4.6 4.9 ± 0.3 36.9 ± 9.1 20.1 ± 2.6 8.0 ± 0.8 55(66.3) t 4.885 −1.413 −3.911 −5.944 8.299 9.302 8.144 5.831 P < 0.001* 0.163 < 0.001* < 0.001* < 0.001* < 0.001* 0.007* 0.001* FI-CD 无衰弱(n = 206) 75.5 68.3 ± 6.1 3.1 ± 1.3 122.2 ± 8.4 38.3 ± 3.2 4.4 ± 0.3 22.4 ± 8.1 17.7 ± 1.7 7.2 ± 0.5 24(11.7) 衰弱(n = 67) 24.5 73.4 ± 7.3 3.1 ± 1.3 111.2 ± 12.7 33.0 ± 3.8 5.0 ± 0.3 39.2 ± 7.8 21.6 ± 2.4 8.1 ± 0.8 44(65.7) t 4.434 −1.085 −5.236 −5.325 10.655 11.088 11.552 7.790 P < 0.001* 0.182 0.004* < 0.001* < 0.001* < 0.001* 0.001* < 0.001* FS 无衰弱(n = 195) 71.4 68.1 ± 6.0 3.1 ± 1.3 122.2 ± 8.6 38.1 ± 3.4 4.4 ± 0.3 22.8 ± 8.2 17.8 ± 1.7 7.3 ± 0.5 18(9.2) 衰弱(n = 78) 28.6 72.9 ± 7.9 3.1 ± 1.4 112.3 ± 12.4 33.9 ± 4.3 5.0 ± 0.3 37.4 ± 8.6 21.2 ± 2.4 8.0 ± 0.8 50(64.1) t 5.516 −0.153 −5.574 −5.902 10.956 10.122 11.281 7.256 P < 0.001* 0.076 < 0.001* < 0.001* 0.008* < 0.001* < 0.001* < 0.001* TFI 无衰弱(n = 201) 73.6 68.7 ± 6.3 3.1 ± 1.3 121.8 ± 9.0 38.0 ± 3.5 4.4 ± 0.3 23.1 ± 8.5 17.8 ± 1.8 7.3 ± 0.5 25(12.4) 衰弱(n = 72) 26.4 71.8 ± 7.9 3.1 ± 1.3 112.5 ± 12.1 33.9 ± 4.1 5.0 ± 0.4 37.6 ± 8.6 21.3 ± 2.5 8.1 ± 0.8 43(59.7) t 2.540 −0.490 −4.756 −3.980 9.204 9.619 10.032 6.542 P 0.003* 0.227 0.005* < 0.001* < 0.001* < 0.001* < 0.001* 0.005* *P < 0.05。 表 3 FP、FI-CD、FS、TFI 4种衰弱评估方法评估衰弱的一致性比较
Table 3. Consistency comparison of frailty assessment by FP,FI-CD,FS,TFI four frailty assessment tools
项目FP FS TFI FI FP TFI 非衰弱 衰弱 非衰弱 衰弱 非衰弱 衰弱 非衰弱 衰弱 非衰弱 衰弱 非衰弱 衰弱 FI TFI FI FS FS FP 非衰弱 172 34 非衰弱 175 26 非衰弱 180 26 非衰弱 182 13 非衰弱 170 25 非衰弱 166 24 衰弱 18 49 衰弱 20 52 衰弱 21 46 衰弱 24 54 衰弱 20 58 衰弱 35 48 Kappa值 0.52 0.58 0.54 0.65 0.60 0.47 表 4 FP、FI-CD、FS、TFI对术后并发症的预测效能比较
Table 4. Comparison of the predictive power of FP,FI-CD,FS,and TFI for postoperative complications
项目 截断值 AUC 敏感度Se 特异度Sp 准确度Ac 阳性预测值PPV 阴性预测值NPV 诊断比值比DOR FP 2.5 0.896 0.809 0.863 0.850 0.663 0.932 26.745 FI-CD 0.40 0.767 0.648 0.889 0.828 0.658 0.884 14.507 FS 3.0 0.799 0.735 0.863 0.832 0.641 0.908 17.560 TFI 4.5 0.745 0.632 0.859 0.802 0.597 0.876 10.439 -
[1] 马彩莉,张孟喜. 老年糖尿病合并衰弱的研究进展[J]. 中华现代护理杂志,2019,25(10):1209-1211. doi: 10.3760/cma.j.issn.1674-2907.2019.10.005 [2] Rodrguez-Mañas L,Féart C,Mann G,et al,on behalf of the FOD-CC group. Searching for an operational definition of frailty:A Delphi method based consensus statement. The Frailty Operative Definition-Consensus Conference Project[J]. J Gerontol A BiolSci Med Sci,2013,68(1):62-67. doi: 10.1093/gerona/gls119 [3] Nicoleta Stoicea1,Ramya Baddigam,Jennifer Wajahn,et al. The gap between clinical research and standard of care:a review of frailty assessment scales in perioperative surgical settings[J]. Frontiers In Public Health,2016,150(4):1-7. [4] Kulmala J,Nykänen I,Hartikainen S. Frailty as apredictor of all-cause mortality in older men and women[J]. Geriatr Gerontol Int,2014,14(4):899-905. doi: 10.1111/ggi.12190 [5] Ana,Izabel,Lopes,et al. Frailty as a predictor of adverse outcomes in hospitalized older adults:A systematic review and meta-analysis[J]. Ageing Research Reviews,2019,56:100960-101018. doi: 10.1016/j.arr.2019.00960 [6] 奚兴,郭桂芳,孙静. 老年人衰弱评估工具及其应用研究进展[J]. 中国老年学杂志,2015,35(20):5993-5996. doi: 10.3969/j.issn.1005-9202.2015.20.153 [7] Avila-Funes J A, Aguilar-Navarro S, Melano-Carranza E. Frailty, an enigmatic and controversial concept in geriatrics. The biological perspective[J]. Gac M é d De M é xico, 2008, 144(3): 255-262. [8] Wou F, Gladman J F R, Bradshaw L, et al, Conroy SP: The predictive properties of frailt–rating scales in the acute medical unit [J]. Age ageing, 2013, 42: 776 - 781. [9] Coelho T,Paul C,Gobbens R J,et al. Frailty as a predictor of shortterm advese outcomes[J]. Peer J,2015,3(30):e1121. [10] 中华医学会老年医学分会. 老年患者衰弱评估与干预中国专家共识[J]. 中华老年医学杂志,2017,36(3):251-256. doi: 10.3760/cma.j.issn.0254-9026.2017.03.007 [11] Zhao Y,Lu Y,Zhao W,et al. Long sleep duration is associated with cognitive frailty among older community-dwelling adults:results from West China Health and Aging Trend Study[J]. BMC Geriatr,2021,21(1):608. doi: 10.1186/s12877-021-02455-9 [12] 杨帆,陈庆伟. 老年住院患者衰弱状态及其影响因素分析研究[J]. 中国全科医学,2018,21(2):173-179. [13] Fried L P,Tangen C M,Walston J,et al. Frailty in older adults:evidence for a phenotype[J]. J Gerontol A BiolSci Med Sci,2001,56(3):146-156. doi: 10.1093/gerona/56.3.M146 [14] Mitnitski A B,Mogilner A J,Rockwood K. Accumulation of deficits as a proxy measure of aging[J]. Scientific World Journal,2001,1(8):323-336. [15] Saum K U,Dieffenbach A K,Müller H. Frailty prevalence and 10-year survival in community-dwelling older adults:results from the E STHER cohort study[J]. Eur J Epidemiol,2014,29(3):171-179. doi: 10.1007/s10654-014-9891-6 [16] Abellan van Kan G,Rolland Y,Bergman H,et al. The I. A. N. A task force on frailty assessment of older people in clinical practice[J]. J Nutr Health Aging,2008,12(1):29-37. [17] Gobbens R J,Van Assen M A,Luijkx K G,et al. The tilburg frailty indicator:Psychometric properties[J]. J Am Med Dir Assoc,2010,11(50):344-355. [18] 奚兴,郭桂芳,孙静. 中文版Tilburg 衰弱评估量表的信效度研究[J]. 护理学报,2013,20(8B):1-5. [19] Dong L,Liu N,Tian X,et al. Reliability and validity of the Tilburg Frailty Indicator (TFI) among Chinese community-dwelling older people[J]. Archives of gerontology and geriatrics,2017,73:21-28. doi: 10.1016/j.archger.2017.07.001 [20] 韩斌如,李秋萍. 老年患者手术风险评估工具的应用进展[J]. 护理学报,2017,24(331):36-39. doi: 10.16460/j.issn1008-9969.2017.24.031 [21] Tepas J J. Simple frailty score predicts postoperative complications across surgical specialties[J]. Am J Surg,2013,206(5):818. [22] Hewitt J,Moug S J,Middleton M,et al. Prevalence of frailty and its association with mortality in general surgery[J]. Am J Surg,2015,209(2):254-259. [23] Oakland K,Nadler R,Cresswell L,et al. Systematic re-view and Meta-analysis of the association between frailty and outcome in surgical patients[J]. Ann R Coll Surg En-gl,2016,98(2):80-85. doi: 10.1308/rcsann.2016.0048 [24] Chow W B,Rosenthal R A,Merkow R P,et a1. Optimal preoperative assessment of the geriatric surgical patient:a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society[J]. J Am Coil Surg,2012,215(4):453-466. doi: 10.1016/j.jamcollsurg.2012.06.017 [25] 中华医学会老年医学分会,解放军总医院老年医学教研室,中华老年心脑血管病杂志编辑委员会. 老年患者术前评估中国专家建议(精简版)[J]. 中华老年心脑血管病杂志,2016,18(1):19-24. doi: 10.3969/j.issn.1009-0126.2016.01.006 [26] Tegels J J,J H Stoot. Way forward:Geriatric frailty assessment as risk predictor in gastric cancer surgery[J]. World J Gastrointestinal Surg,2015,7(10):223. doi: 10.4240/wjgs.v7.i10.223 [27] Decoster L,Van Puyvelde K,Mohile S,et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients:an update on SIOG recommendations[J]. Ann Oncol,2015,26(2):288-300. doi: 10.1093/annonc/mdu210 [28] 符琳琳,王青,张少景,等. 四种衰弱评估工具对老年住院患者出院后全因死亡预测效果比较[J]. 中华老年多器官疾病杂志,2020,19(9):651-655. doi: 10.11915/j.issn.1671-5403.2020.09.152 [29] 孟丽,石婧,邹晨双,等. 老年人衰弱程度与肌肉相关指标关系的初步研究[J]. 中华老年医学杂志,2017,36(12):1313-1317. doi: 10.3760/cma.j.issn.0254-9026.2017.12.009 [30] Lin H S,Watts J N,Peel N M,et al. Frailty and post-operative outcomes in older surgical patients: a systematic review[J]. Bmc Geriatrics,2016,16(1):157. [31] Shamliyan T,Talley K M,Ramakrishnan R,et a1. Association of frailty with survival:A systematic literature review[J]. Ageing Res Rev,2013,12(2):719-736. doi: 10.1016/j.arr.2012.03.001 [32] Chong E,Ho E,Baldevarona-Llego J,et al. Frailty in hospitalized older adults:Comparing different frailty measures in predicting short- and long-term patient outcomes[J]. J Am Med Dir Assoc,2018,19(5):450-457. [33] Dent E,Lien C,Lim W S,et al. The Asia-Pacific clinical practice guidelines for the management of frailty[J]. Journal of the American Medical Directors Association,2017,18(7):564-575. [34] 杨丽峰,杨洋,张春梅,等. 老年人衰弱评估量表的编制及信效度检验[J]. 中华护理杂志,2017,52(1):49-53. -





 下载:
下载: