Correlation between NLR Value and Prognosis in Patients with Acute Ischemic Stroke before and after Revascularization
-
摘要:
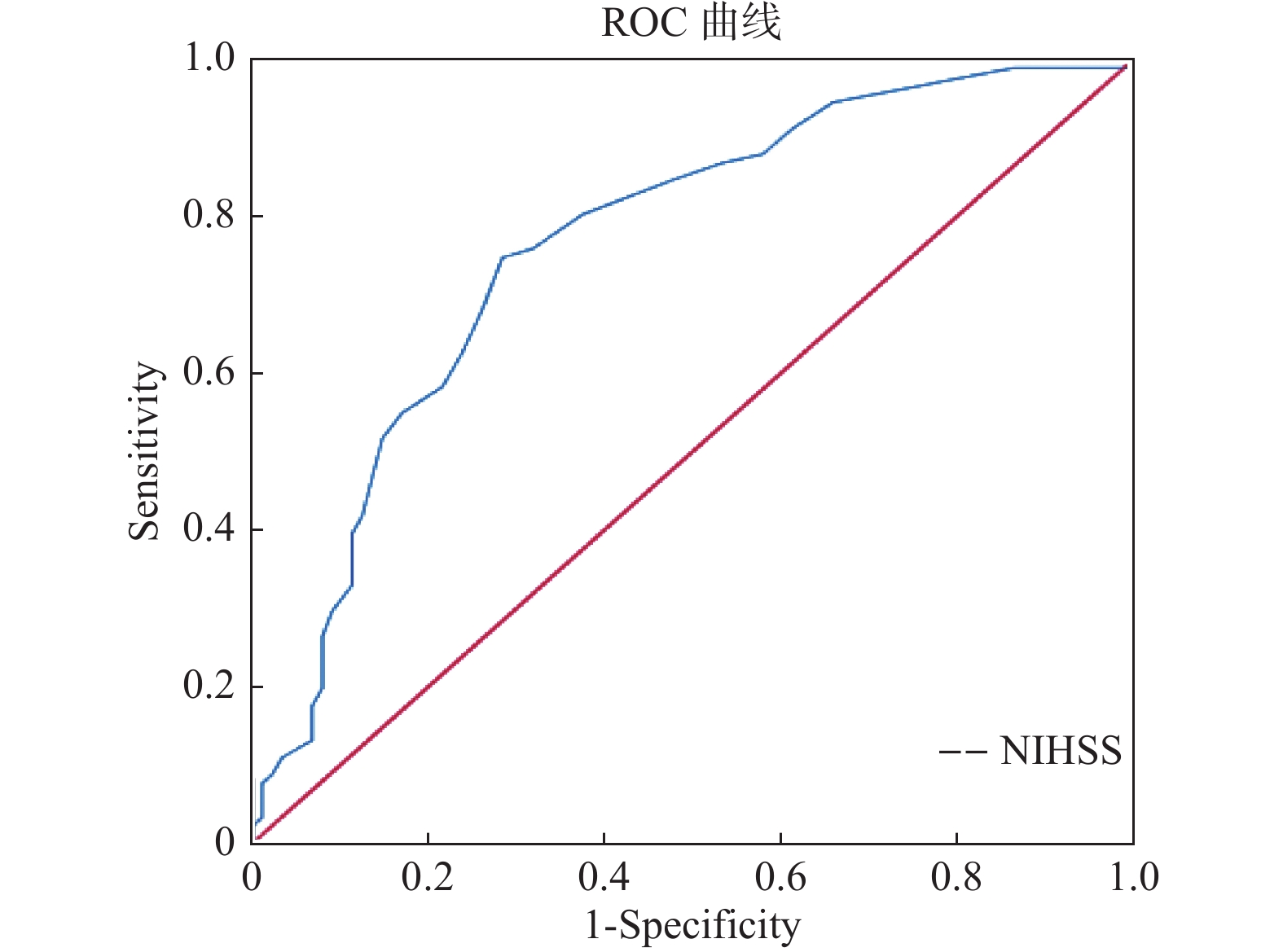
目的 通过研究急性缺血性脑卒中血运重建前后与预后不良有关的影响因素,以期为临床医师预测患者预后提供更多的生物学标志物。 方法 收集2020年12月至2021年10月昆明医科大学附属曲靖医院神经内科及神经介入科收治的急性缺血性脑卒中并接受血运重建治疗(包括静脉溶栓、机械取栓切除术或者2者均行)的患者179例,根据3个月后mRS评分分为预后良好组(mRS < 3分)和预后不良组(mRS≥3分)。比较2组患者的一般资料、临床检验指标、血运重建前后NLR值、NIHSS评分等,并进一步分析预后不良组患者的独立危险因素。 结果 (1)预后良好与预后不良2组患者的甘油三酯、总胆固醇、C反应蛋白、入院的NIHSS评分、中性粒细胞数及百分比、淋巴细胞数及百分比、NLR值及血运重建后8h的白细胞、中性粒细胞数及百分比、淋巴细胞数与百分比、NLR值,差异具有统计学意义(P < 0.05);(2)多因素Logistic回归分析,入院NIHSS评分(OR = 1.123,95% CI 1.065~1.184,P < 0.05)是AIS患者血运重建后3个月预后不良的独立危险因素,临床诊断分界值为11;(3)NLR值比较:预后不良组血运重建前后的NLR值均高于预后良好组,差异有统计学意义(P < 0.05),AIS患者血运重建后NLR值较血运重建前升高,差异有统计学意义(P < 0.05)。 结论 入院时的NIHSS评分是AIS血运重建患者发病3个月不良预后的独立危险因素。AIS患者血运重建前后NLR变化具有上升趋势,预后不良组血运重建前后的NLR高于预后良好组,但并非AIS患者血运重建3个月后不良预后的独立危险因素。 -
关键词:
- 急性缺血性脑卒中 /
- 中性粒细胞与淋巴细胞比值 /
- 血运重建 /
- 预后
Abstract:Objective To study the influencing factors of poor prognosis before and after revascularization of acute ischemic stroke, so as to provide more biomarkers for prognosis prediction. Methods A total of 179 patients with acute ischemic stroke who received revascularization therapy (including intravenous thrombolysis, mechanical thrombectomy, or both) admitted to the Department of Neurology and The Department of Neurointervention of Qujing Hospital Affiliated to Kunming Medical University from December 2020 to October 2021 were collected. According to mRS score after 3 months, the patients were divided into good prognosis group (mRS < 3) and poor prognosis group (mRS≥3). General data, clinical test indicators, NLR value and NIHSS score before and after revascularization were compared between the two groups, and independent risk factors of patients with poor prognosis were further analyzed. Results There are siginificant differences in triglyceride, total cholesterol, c-reactive protein, NIHSS score, the number of neutrophils and percentage of the hospital, lymphocyte count and percentage, NLR value and reascularization 8 hours after the number of white blood cells, neutrophils and percentage, lymphocyte count and percentage, NLR value between the two groups (P < 0.05). Multivariate Logistic regression analysis showed that admission NIHSS score (OR=1.123, 95%CI 1.065-1.184, P < 0.05) was an independent risk factor for poor prognosis 3 months after revascularization in AIS patients, with a clinical diagnostic cut-off value of 11. The NLR values of the poor prognosis group before and after revascularization were higher than those of the good prognosis group, the difference was statistically significant (P < 0.05). The NLR values of AIS patients after revascularization were higher than those before revascularization, the difference was statistically significant (P < 0.05). Conclusion NIHSS score at admission is an independent risk factor for poor prognosis at 3 months in patients with AIS revascularization. Changes in NLR in AIS patients before and after revascularization showed an upward trend, and NLR in the poor prognosis group was higher than that in the good prognosis group before and after revascularization, but it was not an independent risk factor for poor prognosis in AIS patients 3 months after revascularization. -
表 1 预后良好组与预后不良组一般信息、实验室检查结果比较[(
$ \bar x \pm s $ )/n(%)/M(P25,P75)]Table 1. Comparison of general information,laboratory examination results between two groups[(
$ \bar x \pm s $ )n(%)/M(P25,P75)]变量 预后良好(n = 88) 预后不良(n = 91) t/Z P 男性 57(64.77 ) 57(62.64 ) −0.296 0.767 年龄(岁) 66(57,74) 66(56,75) −0.202 0.840 高血压病 49(55.68) 55(60.44) −0.643 0.520 糖尿病 15(17.05) 20(21.98) −0.830 0.407 心房颤动 11(12.50) 16(17.58) −0.947 0.344 冠心病 8(9.09) 7(7.69) −0.360 0.719 同型半胱氨酸(μmol/L) 14(11.25,18.00) 13(11,18) −0.578 0.564 高密度脂蛋白(mmol/L) 1.13(0.96,1.28) 1.17(1.03,1.42) −1.926 0.054 低密度脂蛋白(mmol/L) 2.87(2.50,3.40) 2.78(2.33,3.31) −0.831 0.406 总胆固醇(mmol/L) 4.45(3.83,5.12) 4.46(3.89,5.01) −0.400 0.689 甘油三酯(mmol/L) 1.35(1.01,1.99) 1.16(0.95,1.53) −2.303 0.021* 总胆红素(µmol/L) 12.75(9.33,16.67) 15.3(9.7,24.00) −2.992 0.003* C-反应蛋白(mg/L) 2.3(1.12,6.22) 6.9(2.71,17.7) −4.802 0.000* 脂蛋白(mg/L) 132(63,216) 132(65,290) −0.573 0.567 入院时NIHSS评分 8(4,13) 17(11,22) −6.127 0.000* *P < 0.05 。 表 2 预后良好组与预后不良组相关血常规指标的比较[M(P25,P75)]
Table 2. Comparison of blood routine indexes between the two groups [M(P25,P75)]
变量 预后良好(n = 88) 预后不良(n = 91) t/Z P 血运重建前 中性粒百分比 69.6(60.05,80.37) 77(62.58,83.71) −2.642 0.008* 淋巴百分比 22.7(13.32,31.55) 16.7(10.8,27.00) −2.422 0.015* 白细胞(×109/L) 8.3(6.12,10.25) 8.7(6.61,11.12) −1.301 0.193 中性粒值(×109/L) 5.83(3.71,8.11) 6.52(4.41,8.82) −1.613 0.107* 淋巴细胞值(×109/L) 1.74(1.32,2.22) 1.42(1.04,2.01) −2.437 0.015* NLR 2.99(1.97,6.08) 4.55(2.35,7.91) −2.292 0.022* 血运重建后8 h 中性粒百分百比 72.4(62.1,81.48) 78.4(72,85.9) −3.892 0.000* 淋巴百分比 17.85(11.65,27.88) 14.6(7.71,19.63) −3.819 0.000* 白细胞(×109/L) 7.55(6.35,10.20) 8.95(7.10,11.62) −2.706 0.007* 中性粒值(×109/L) 5.61(3.59,7.86) 7.27(5.28,9.27) −3.356 0.001* 淋巴值(×109/L) 1.42(1.02,1.91) 1.22(0.83,1.57) −2.761 0.006* NLR 4.07(2.23,6.79) 5.39(3.74,10.78) −3.822 0.000* *P < 0.05。 表 3 AIS患者预后的多因素Logistic回归分析
Table 3. Multivariate Logistic regression analysis of prognosis in AIS patients
检验变量 B Wals OR值(95%CI) P NIHSS 0.116 18.376 1.123(1.065~1.184) 0.000* C反应蛋白 0.012 1.695 1.012(0.994~1.030) 0.193 甘油三脂 0.414 3.072 0.661(0.416~1.035) 0.080 总胆固醇 0.042 0.034 1.043(0.669~1.624) 0.854 血运重建前 中性粒值(×109/L) −5.385 2.842 0.005(0.001~2.399) 0.092 中性粒百分比 0.427 2.166 1.532(0.868~2.705) 0.141 淋巴值(×109/L) −6.640 2.922 0.001(0.000~2.646) 0.087 淋巴百分比 0.528 2.345 1.696(0.892~3.336) 0.126 NLR值 −0.040 0.196 0.961(0.805~1.147) 0.658 血运重建后8 h NLR值 0.136 2.353 1.145(0.963~1.362) 0.125 白细胞数(×109/L) 0.352 0.011 1.421(0.002~11.70) 0.918 中性粒值(×109/L) −0.729 0.041 0.026(0.001~11.162) 0.239 中性粒百分比 0.314 1.199 1.369(0.780~2.404) 0.274 淋巴值(×109/L) −2.171 0.350 0.114(0.001~10.944) 0.555 淋巴百分比 0.026 0.005 1.027(0.486~2.168) 0.945 *P < 0.05。 表 4 AIS患者血运重建前后血常规相关指标的变化[(n = 179),M(P25,P75)]
Table 4. Changes of blood routine indexes in AIS patients before and after revascularization [(n = 179),M(P25,P75)]
检验值 治疗前 治疗后8 h Z P NLR值 3.56(2.11,6.37) 4.94(2.85,8.26) −4.054 0.000* 白细胞(×109/L) 8.50(6.40,10.90) 8.55(6.70,10.90) −0.067 0.947 中性粒值(×109/L) 6.10(3.91,8.38) 6.51(4.74,8.53) −1.320 0.187 淋巴值(×109/L) 1.57(1.15,2.05) 1.31(0.97,1.76) −5.911 0.000* 中性粒细胞(%) 73.3(62.7,81.2) 76.4(67.6,83.7) −3.451 0.001* 淋巴细胞(%) 19.5(12.7,29.0) 15.5(10.1,23.3) −5.027 0.000* *P < 0.05。 -
[1] Liu J,Shi Z,Bai R,et al. Temporal,geographical and demographic trends of stroke prevalence in China:A systematic review and meta-analysis[J]. Ann Transl Med,2020,8(21):1432. doi: 10.21037/atm-19-4342 [2] M ü ller S,Kufner A,Dell’Orco A,et al. Evolution of bood-brain barrier permeability in subacute ischemic stroke and associations with serum biomarkers and functional outcome[J]. Front Neurol,2021,12(6):730923. [3] 中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2018[J]. 中华神经科杂志,2018,51(9):666-682. doi: 10.3760/cma.j.issn.1006-7876.2018.09.004 [4] Yu A Y,Hill M D,Coutts S B. Should minor stroke patients be thrombolyzed? A focused review and future directions[J]. Int J Stroke,2015,10(3):292-297. doi: 10.1111/ijs.12426 [5] Zhang J,Yuan C,Deng X,et al. Efficacy and safety of endovascular treatment with or without intravenous alteplase in acute anterior circulation large vessel occlusion stroke:A meta-analysis of randomized controlled trials[J]. Neurol Sci,2022,22(9):207. [6] Świtońska M,Piekuś-Słomka N,Słomka A,et al. Neutrophil-to-lymphocyte ratio and symptomatic hemorrhagic transformation in ischemic stroke patients undergoing revascularization[J]. Brain Sci,2020,10(11):771. doi: 10.3390/brainsci10110771 [7] 徐慈航,李敬伟,朱晓蕾,等. 急性缺血性卒中出血转化的研究进展[J]. 中国卒中杂志,2020,15(4):446-451. doi: 10.3969/j.issn.1673-5765.2020.04.020 [8] Lee Y B,Yoon W,Lee Y Y,et al. Predictors and impact of hemorrhagic transformations after endovascular thrombectomy in patients with acute large vessel occlusions[J]. J Neurointerv Surg,2019,11(5):469-473. doi: 10.1136/neurintsurg-2018-014080 [9] Zhang W B,Zeng Y Y,Wang F,et al. A high neutrophil-to-lymphocyte ratio predicts hemorrhagic transformation of large atherosclerotic infarction in patients with acute ischemic stroke[J]. Aging (Albany NY),2020,12(3):2428-2439. doi: 10.18632/aging.102752 [10] Weng Y,Zeng T,Huang H,et al. Systemic immune-inflammation index predicts 3-month functional outcome in acute ischemic stroke patients treated with intravenous thrombolysis[J]. Clin Interv Aging,2021,16(1):877-886. [11] Khatri R, McKinney A M, Swenson B, Janardhan V. Blood-brain barrier, reperfusion injury, and hemorrhagic transformation in acute ischemic stroke[J]. Neurology, 2012 , 79(13 Suppl 1): 52–57. [12] Maestrini I,Strbian D,Gautier S,et al. Higher neutrophil counts before thrombolysis for cerebral ischemia predict worse outcomes[J]. Neurology,2015,85(16):1408-1416. doi: 10.1212/WNL.0000000000002029 [13] Liu Y L,Lu J K,Yin H P,et al. High Neutrophil-to-lymphocyte ratio predicts hemorrhagic transformation in acute ischemic stroke patients treated with intravenous thrombolysis[J]. Int J Hypertens,2020,2020(3):5980261. [14] Semerano A,Laredo C,Zhao Y,et al. Leukocytes,collateral circulation,and reperfusion in ischemic stroke patients treated with mechanical thrombectomy[J]. Stroke,2019,50(12):3456-3464. doi: 10.1161/STROKEAHA.119.026743 [15] 刘畅,董萌,刘继红,等. 急性脑梗死患者静脉溶栓前中性粒细胞百分比与溶栓后临床结局的关系[J]. 中国当代医药,2020,27(19):77-80. doi: 10.3969/j.issn.1674-4721.2020.19.022 [16] Köm ü rc ü H F,Gözke E,Doğan Ak P,et al. Changes in neutrophil,lymphocyte,platelet ratios and their relationship with NIHSS after rtPA and/or thrombectomy in ischemic stroke[J]. J Stroke Cerebrovasc Dis,2020,29(8):105004. doi: 10.1016/j.jstrokecerebrovasdis.2020.105004 -






 下载:
下载: