Risk Factors of Readmission in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease and Establishment of Risk Prediction Model
-
摘要:
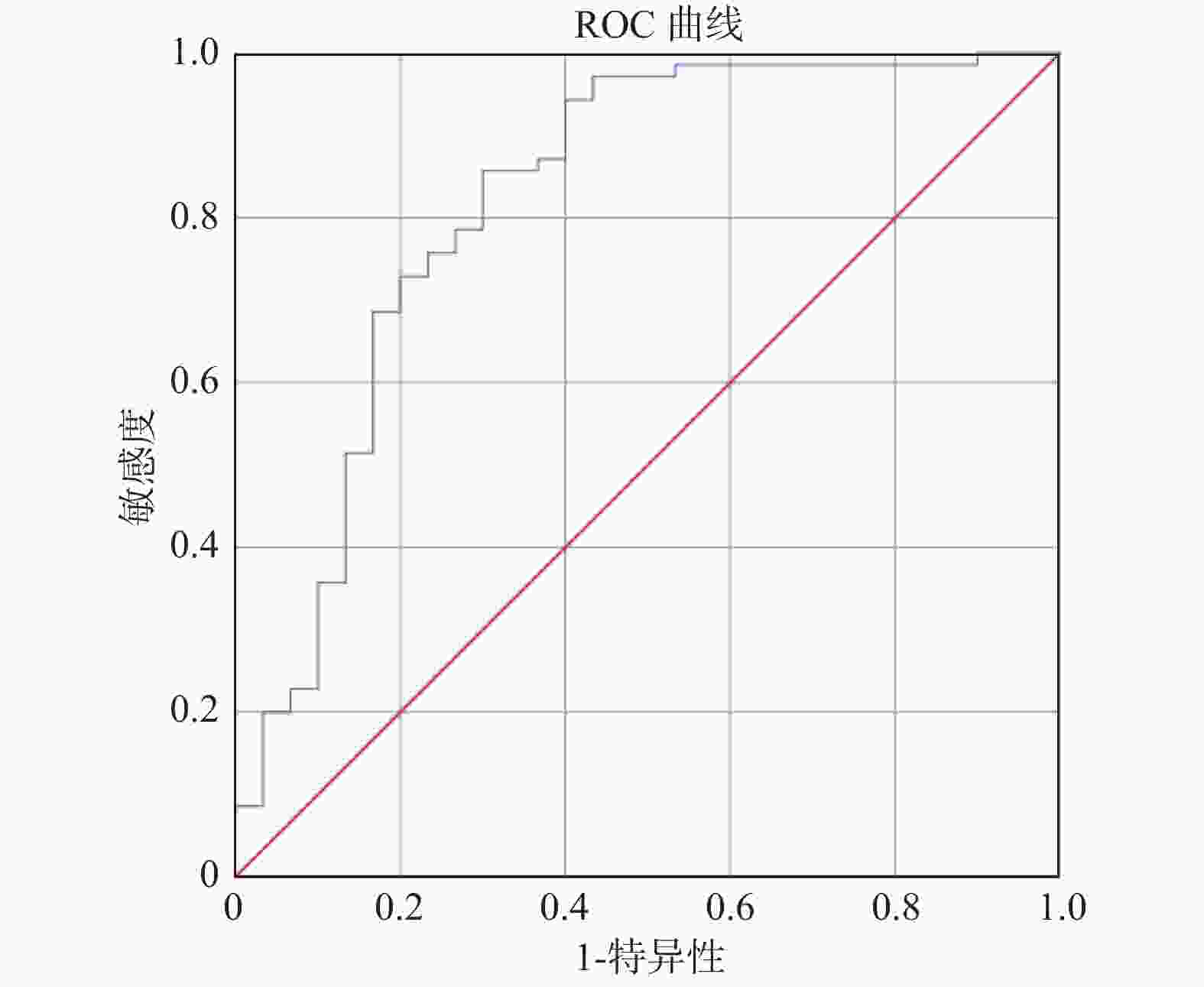
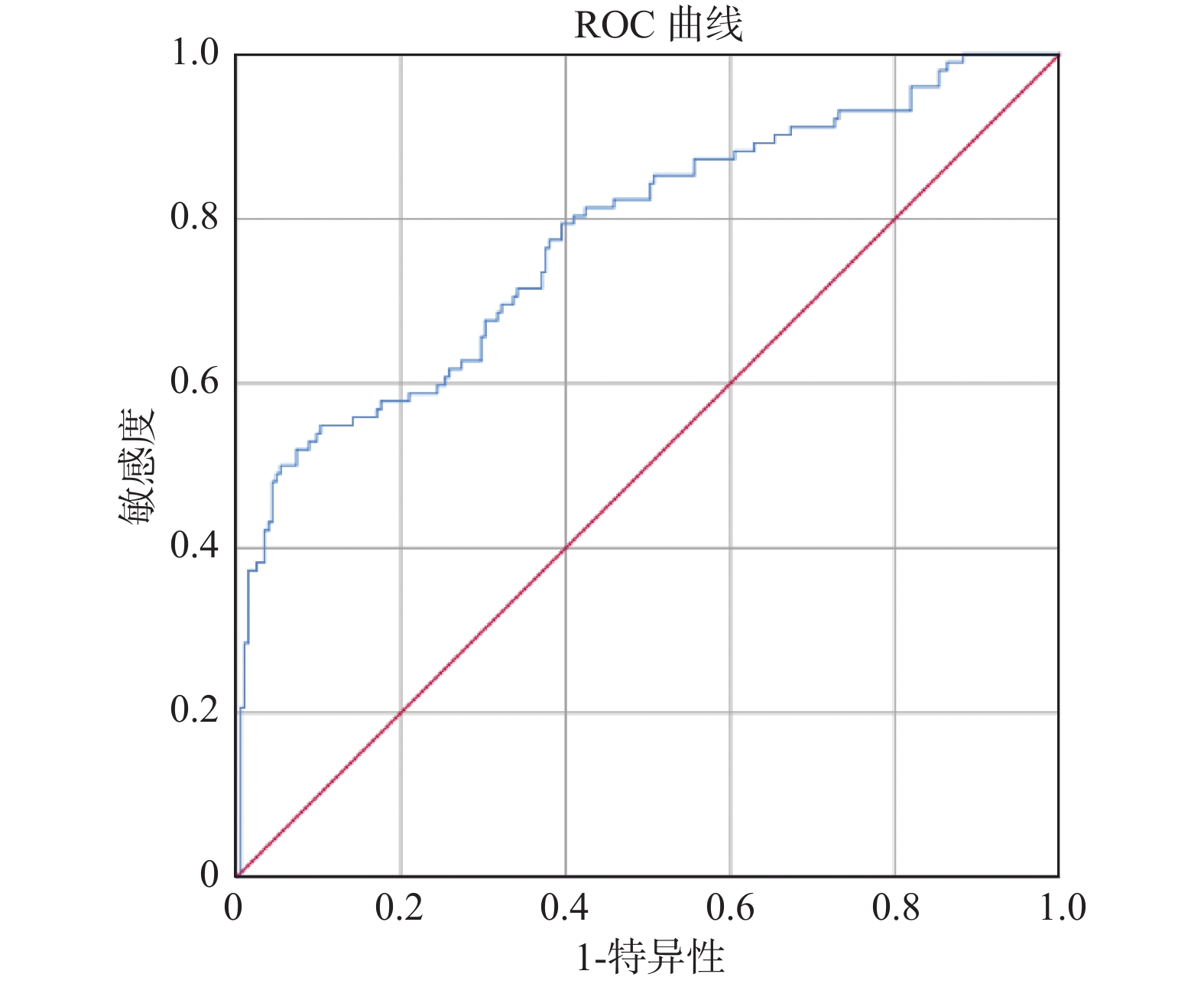
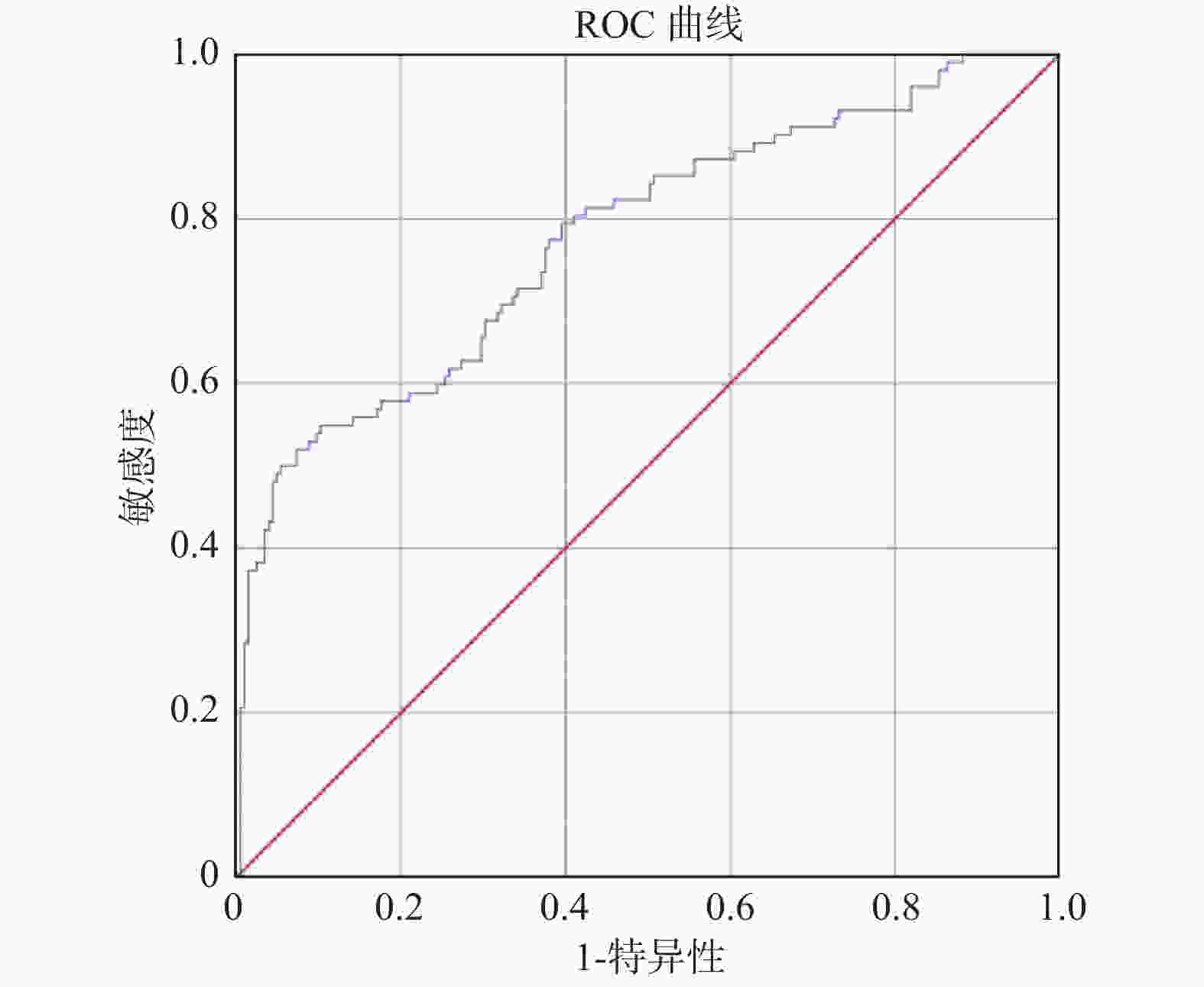
目的 探讨慢性阻塞性肺疾病急性加重期(acute exacerbation of chronic obstructive pulmonary disease,AECOPD)患者发生再入院的危险因素并构建疾病风险预测模型,旨在为早期识别并筛选AECOPD再次入院的高风险患者提供评估工具。 方法 选取云南省某三甲医院2016年1月1日至2021年1月1日诊断为AECOPD且符合纳入、排除标准的414例患者为研究对象。将其中70%(307例)的患者作为建模组,剩余30%(107例)患者作为验证组。根据患者是否发生再入院作为结局指标,分析 AECOPD患者发生再入院的危险因素并构建疾病风险预测模型。 结果 最终纳入年龄(OR = 0.958)、雾化吸入激素种类(OR = 1.893)、FEF75预计值(OR = 0.583)、FEV1实际值(OR = 1.947)、合并呼吸衰竭(OR = 0.501)5个预测因子。预测模型公式:P = 1/{1+exp[−(3.361+(−0.043)× 年龄+0.638 ×吸入雾化激素种类+(−0.539)×FEF75预计值+0.666 ×FEV1实际值+(−0.691)×合并呼吸衰竭)]},建模组受试者特征工作曲线下面积(AUC)为0.777,其灵敏度和特异度分别为0.898和0.549。验证组受试者特征工作曲线下面积(AUC)为0.821,灵敏度和特异度分别为0.857和0.7。 结论 研究所构建的AECOPD患者再入院风险预测模型具有良好的预测效能,为早期识别并筛选AECOPD再次入院的高风险患者提供了评估工具,为医护人员调整高风险患者的治疗和护理提供参考依据,为减轻患者痛苦,减少家庭及社会负担,提高护理服务质量提供科学依据。 Abstract:Objective To explore the risk factors of readmission in patients with AECOPD and develop a disease risk prediction model, aiming to provide an evaluation tool for early identification and screening of patients at high risk of readmission with AECOPD. Methods A total of 414 patients diagnosed with AECOPD in a tertiary hospital in Yunnan Province from January 1, 2016 to January 1, 2021 and met the criteria for inclusion and exclusion were selected as the study subjects. 70% (307) of these patients were included as the modeling group and the remaining 30% (107) patients were included as the validation group. According to whether patients have readmission as an outcome indicator, the risk factors for readmission of patients with AECOPD are analyzed and a disease risk prediction model is constructed. Results Age (OR = 0.958), nebulized inhaled hormone (OR = 1.893), predicted value of FEF75 (OR = 0.583), actual value of FEV1 (OR = 1.947) and combined respiratory failure (OR = 0.501) were included. Prediction model formula: P = 1/{1 + exp [− (3.361 + (−0.043)×age + 0.638×type of inhaled nebulized hormone + (−0.539)×predicted value of FEF75 + 0.666 × actual value of FEV1 + (−0.691)×respiratory failure)]}. The area under ROC curve (AUC) of the modeling group was 0.777, and the sensitivity and specificity were 0.898 and 0.549, respectively. The area under ROC curve (AUC) of the verification group was 0.821, and the sensitivity and specificity were 0.857 and 0.7, respectively. Conclusion The risk prediction model for readmission of AECOPD patients established in this study has good predictive efficacy, providing an evaluation tool for early identification and screening of high-risk patients with AECOPD readmission, and provides a reference for medical staff to adjust the treatment and care of high-risk patients. -
Key words:
- AECOPD /
- Readmission /
- Influencing factors /
- Prediction model /
- Nursing care
-
表 1 AECOPD患者再入院单因素分析( $ \bar x \pm s $)
Table 1. Single Factor analysis of patient readmission in AECOPD ( $ \bar x \pm s $)
变量 均数 ± 标准差
χ2/t P 变量 分组 再入院组
(n = 102)非再入院组
(n = 205)χ2/t P 年龄(岁) 68.48 ± 9.553 2.877 0.004* 体力劳动 是 24 78 5.314 0.021* FEV1/FVC
预计值(%)75.45 ± 5.00 −2.227 0.027* 否 75 130 吸入雾化
激素种类(种)1.07 ± 0.54 −2.909 0.004* 鼻导管吸氧 是 82 20 11.17 0.001* 戒烟时长(a) 1.42 ± 5.044 9406 0.025* 否 126 79 鼻导管吸入
氧浓度(L/min)1.66 ± 1.251 8232.5 0.001* 呼吸衰竭 是 61 41 13.618 < 0.001 * COPD病程(a) 9.50 ± 8.66 7950 0.001* − 否 77 128 并发症个数(个) 1.18 ± 1.061 8526 0.006* 肺心病 是 37 65 6.105 0.013* 入院时二氧化碳
分压(mmHg)41.34 ± 19.94 8807 0.024* 否 47 158 FEF25预计值(L/min) 5.81 ± 1.81 13383.5 < 0.001 * 文化程度 文盲 13 27 17.37 0.002* FEF75预计值(L/min) 1.73 ± 1.83 7716 < 0.001 * 小学 16 67 FEV1实际值(L/min) 1.38 ± 0.64 13146 < 0.001 * 初中 39 53 FEV1/FVC实际值(%) 52.9 ± 21.2 12051 0.029* 高中 10 32 FEF25实际值(L/min) 1.79 ± 1.55 14665 < 0.001 * 大专及以上 24 26 FEF50实际值(L/min) 0.82 ± 0.62 12796 0.001* − − − − − − MMEF75/25实际值(L/min) 0.63 ± 0.57 13498 < 0.001 * − − − − − − *P < 0.05。 表 2 AECOPD患者再入院Logistic回归分析
Table 2. Logistic regression analysis of patient readmissions in AECOPD
变量 B值 标准误 Wald χ2 P OR 95% CI 常数 3.361 1.325 6.434 0.011* 28.83 − 年龄 −0.043 0.016 6.721 0.01* 0.958 0.928~0.99 吸入雾化激素种类 0.638 0.282 5.111 0.024* 1.893 1.089~3.291 FEF75预计值 −0.539 0.116 21.439 < 0.001 * 0.583 0.464~0.733 FEV1实际值 0.666 0.267 6.229 0.013* 1.947 1.154~3.285 是否伴有呼吸衰竭 −0.691 0.294 5.519 0.019* 0.501 0.282~0.892 *P < 0.05。 -
[1] 张丽,范忠杰,周凡. 慢性阻塞性肺疾病急性加重期肺部感染患者的病原菌分布、耐药性及危险因素分析[J]. 中国病原生物学杂志,2019,14(12):1456-1459. doi: 10.13350/j.cjpb.191219 [2] Landrum L,Weinrich S. Readmission data for outcomes measurement:Identifying and strengthening the empirical base[J]. Qual Manag Health Care,2006,15(2):83-95. doi: 10.1097/00019514-200604000-00003 [3] Hartl S,Lopez-Campos J L,Pozo-Rodriguez F,et al. Risk of death and readmission of hospital-admitted COPD exacerbations:European COPD audit[J]. Eur Respir,2016,47(1):113-121. doi: 10.1183/13993003.01391-2014 [4] Jacobs D M,Noyes K,Zhao J,et al. Early hospital readmissions after an acute exacerbation of chronic obstructive pulmonary disease in the nationwide readmissions database[J]. Ann Am Thorac Soc,2018,15(7):837-845. doi: 10.1513/AnnalsATS.201712-913OC [5] Vogelmeier C F,Criner G J,Martinez F J,et al. Global strategy for the diagnosis,management,and prevention of chronic obstructive lung disease 2017 report:Gold executive summary[J]. Am J Respir Crit Care Med,2017,195(5):557-582. doi: 10.1164/rccm.201701-0218PP [6] Capistrano S J,et al. Evidence of Biomass Smoke Exposure as a causative factor for the development of COPD[J]. Toxics,2017,5(4):36. doi: 10.3390/toxics5040036 [7] O’Brien R. A caution regarding rules of thumb for variance inflation factor[J]. Qual Quant,2007,41(5):673-690. doi: 10.1007/s11135-006-9018-6 [8] Lau,C S,Siracuse,B L,Chamberlain,R S. Readmission after COPD exacerbation scale:determining 30-day readmission risk for COPD patients[J]. Int J Chron Obstruct Pulmon Dis,2017,12(6):1891-1902. [9] Hakim M A,Garden F L,Jennings M D,et al. Performance of the LACE index to predict 30-day hospital readmissions in patients with chronic obstructive pulmonary disease[J]. Clin Epidemiol,2018,10(12):51-59. [10] Shu C C,Lin Y F,Hsu N C,et al. Risk factors for 30-day readmission in general medical patients admitted from the emergency department:A single centre study[J]. Intern Med J.,2012,42(6):677-682. doi: 10.1111/j.1445-5994.2011.02562.x [11] Harries T H,Thornton H,Crichton S,et al. Hospital readmissions for COPD:A retrospective longitudinal study[J]. NPJ Prim Care Respir Med,2017,27(1):31. doi: 10.1038/s41533-017-0028-8 [12] 张瑞,吴珍珍,常艳,等. 老年慢性阻塞性肺疾病患者30天内急性加重再入院风险预测模型的构建与验证[J]. 中国呼吸与危重监护杂志,2021,20(7):457-464. [13] 蔡柏蔷,陈荣昌. 慢性阻塞性肺疾病急性加重(AECOPD)诊治中国专家共识(2017 年更新版)[J]. 国际呼吸杂志,2017,37(14):1041-1057. doi: 10.3760/cma.j.issn.1673-436X.2017.14.001 [14] 王明航,蔡坤坤,施丁莉,等. 基于回归分析法建立慢性阻塞性肺疾病急性加重风险预测模型与验证[J]. 中华危重病急救医学,2021,33(01):64-68. doi: 10.3760/cma.j.cn121430-20200720-00534 [15] 潘东霞,钱一建,王春梅,等. 吸烟与室内空气污染的交互作用对慢性阻塞性肺部疾病影响的分析[J]. 中华流行病学杂志,2016,37(11):1444-1449. doi: 10.3760/cma.j.issn.0254-6450.2016.11.002 [16] 黄亚玲,毛兵,闵婕,等. 慢性阻塞性肺疾病稳定期患者共患疾病与一年急性加重风险的关系研究[J]. 中华结核和呼吸杂志,2018,41(5):349-354. doi: 10.3760/cma.j.issn.1001-0939.2018.05.009 [17] 慢性阻塞性肺疾病糖皮质激素规范管理撰写组. 慢性阻塞性肺疾病糖皮质激素规范管理专家共识(2021版)[J]. 中华结核和呼吸杂志,2021,44(12):1054-1063. doi: 10.3760/cma.j.cn112147-20210802-00543 [18] 张维慧,刘颖,李彤彤,等. 雾化吸入和全身用糖皮质激素治疗老年慢性阻塞性肺疾病急性加重期的疗效[J]. 中国老年学杂志,2018,38(16):3902-3904. doi: 10.3969/j.issn.1005-9202.2018.16.026 [19] Mirici A,Meral M,Akgun M. Comparison of efficacy of nebulished budesonide with parenteral corticosteroids in the treatment of acute exacerbations of chronic obstructive pulmonary disease[J]. Clin Drug Invest,2003,23(1):55-62. doi: 10.2165/00044011-200323010-00007 [20] 党瑞志,刘羽. 胸腺肽联合异丙托溴铵雾化吸入对老年COPD合并肺部感染患者肺功能及免疫功能的影响[J]. 中国老年学杂志,2020,40(22):4760-4762. doi: 10.3969/j.issn.1005-9202.2020.22.019 [21] Maltais F,Ostinelli J,Bourbeau J,et al. Comparison of nebulized budesonide and oral prednisolone with placebo in the treatment of acute exacerbations of chronic obstructive pulmonary disease:A randomized controlled trial[J]. Am J Respir Crit Care Med,2002,165(5):698-703. doi: 10.1164/ajrccm.165.5.2109093 [22] Rochwerg B,Brochard L,Elliott M W,et al. Official ERS/ATS clinical practice guidelines:Noninvasive ventilation for acute respiratory failure[J]. Eur Respir J,2017,50(2):1602426. doi: 10.1183/13993003.02426-2016 [23] Peter J V,Moran J L. Noninvasive ventilation in exacerbations of chronic obstructive pulmonary disease:Implications of different meta-analytic strategies[J]. Ann Intern Med,2004,141(5):78-79. doi: 10.7326/0003-4819-141-5-200409070-00031-w1 [24] Lightowler J V,Wedzicha J A,et al. Non-invasive positive pressure ventilation to treat respiratoryfailure resulting from exacerbations of chronic obstructive pulmonary disease:Cochrane systematic review and meta-analysis[J]. BMJ,2003,326(7382):185. doi: 10.1136/bmj.326.7382.185 [25] Shah T,Press V G,et al. COPD Readmissions:Addressing COPD in the Era of Value-based Health Care[J]. Chest,2016,150(4):916-926. doi: 10.1016/j.chest.2016.05.002 [26] Wu Y K,Lan C C,Tzeng I S,et al. The COPD-readmission (CORE) score:A novel prediction model for one-year chronic obstructive pulmonary disease readmissions[J]. J Formos Med Assoc,2021,120(3):1005-1013. doi: 10.1016/j.jfma.2020.08.043 [27] 邓琳,郑劲平. 肺功能检查临床应用研究进展(2018-2019年度)[J]. 中国实用内科杂志,2020,40(9):777-781. doi: 10.19538/j.nk2020090116 [28] Rabe K F,Hurd,S,Anzueto A,et al. Global strategy for the diagnosis,management,and prevention of chronic obstructive pulmonary disease:GOLD executive summary[J]. Am J Respir Crit Care Med,2007,176(6):532-555. doi: 10.1164/rccm.200703-456SO [29] Cen J,Ma H,Chen Z,et al. Monitoring peak expiratory flow could predict COPD exacerbations:A prospective observational study[J]. Respir Med,2019,148:43-48. doi: 10.1016/j.rmed.2019.01.010 [30] Hong W,Earnest A,Sultana P,Koh Z,et al. How accurate are vital signs in predicting clinical outcomes in critically ill emergency department patients[J]. Eur J Emerg Med,2013,20(1):27-32. doi: 10.1097/MEJ.0b013e32834fdcf3 -





 下载:
下载: