Risk Factors for Hypoparathyroidism after Thyroidectomy
-
摘要:
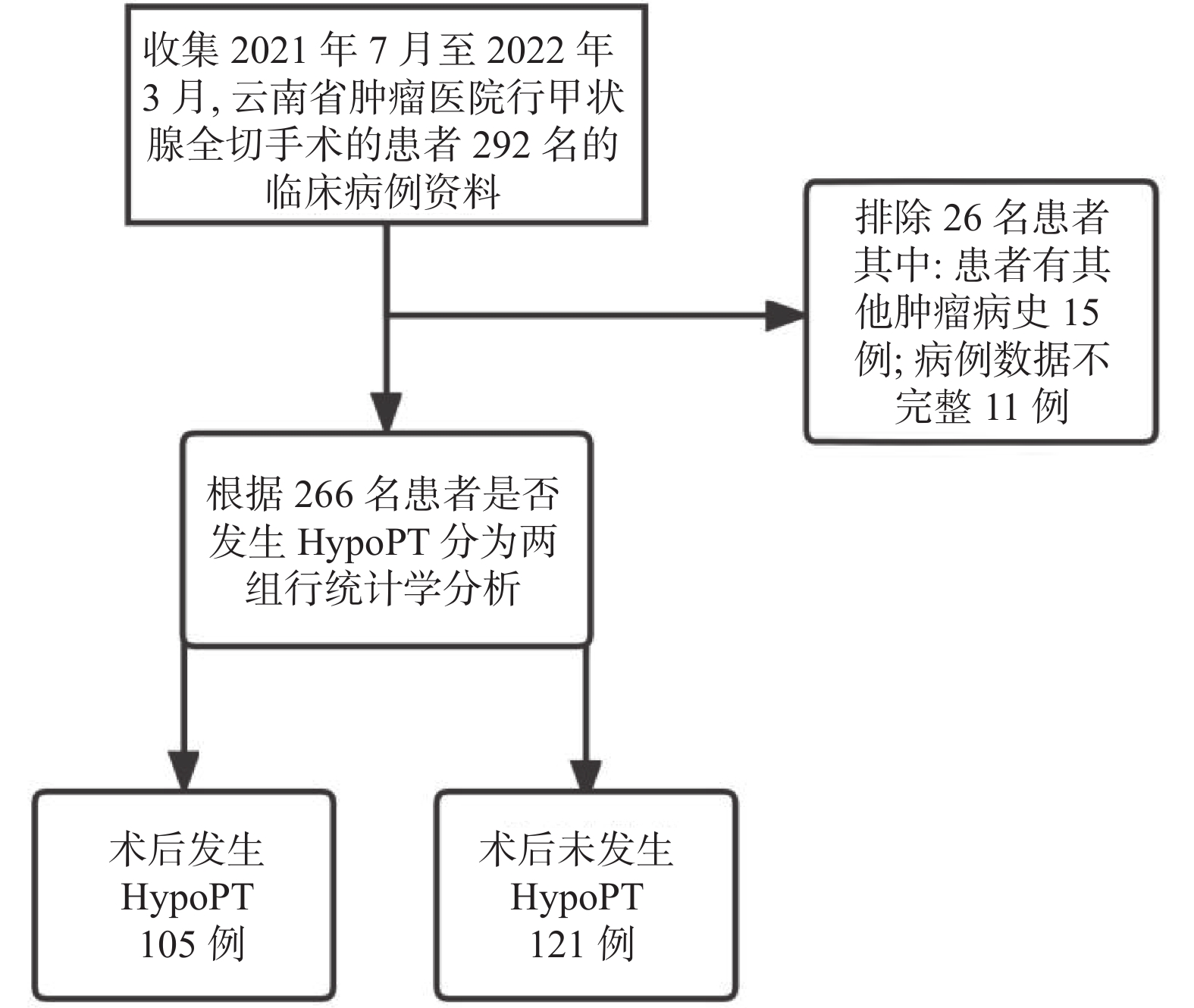
目的 探讨甲状腺切除术后甲状旁腺功能减退(post surgical hypoparathyroidism,HypoPT)的风险因素分析及同时存在风险因素的数量与HypoPT发生率之间的关系,从而指导临床治疗。 方法 回顾性分析2021年7月至2022年3月在云南省肿瘤医院行甲状腺切术后并具备完整病人资料266例,采用单因素分析与多因素Logistic回归分析HypoPT的风险因素分析及同时存在风险因素的数量与HypoPT发生率之间的关系。 结果 (1)单因素分析结果:年龄、体重指数(body mass Index,BMI)、高血压、代谢综合征(metabolicsyndrome,MS)、肿块性质、T分期、VI区淋巴结清扫(central lymph node dissection,CLND)、淋巴结是否转移、周围侵犯、腺叶切除方式(单侧全切、双侧全切)有统计学意义(P < 0.05);(2)Logistic多因素分析结果:MS、CLND、肿块性质、淋巴结是否结转移是HypoPT发生率的独立危险因素( P < 0.05);(3)调整年龄和其他临床因素后,存在风险因素的数量与HypoPT发生率之间的关系之间存在正相关。 结论 (1)年龄、BMI、高血压、MS、肿块性质、T分期、CLND、淋巴结是否转移、周围侵犯、腺叶切除方式会影响HypoPT的发生率;(2) MS、CLND、肿块性质、淋巴结转移是HypoPT的独立危险因素;(3)同时存在风险因素的数量与HypoPT发生率之间存在正相关。 Abstract:Objective To explore the risk factors of hypoparathyroidism (HypoPT) after thyroidec-tomy and analyze the relationship between the number of coexisting risk factors and the incidence of HypoPT, so as to guide the clinical treatment. Methods A total of 266 patients with the complete data after the thyroidectomy in Yunnan Cancer Hospital from July 2021 to March 2022 were retrospectively analyzed. Univariate analysis and multivariate Logistic regression were used to analyze the risk factors of HypoPT and the relationship between the number of co-existing risk factors and the incidence of HypoPT. Results (1) Univariate analysis results: There were statistically significant differences in age, body mass index (BMI), hypertension, metabolic syndrome (MS), mass nature, T stage, central lymph node dissection (CLND) , lymph node metastasis, surrounding invasion, gland lobectomy method (unilateral total resection, bilateral total resection) (P < 0.05); (2) Logistic multivariate analysis results: MS, CLND, tumor nature, Lymph node metastasis were the independent risk factors for the incidence of HypoPT ( P < 0.05); (3) After adjusting for age and other clinical factors, there was a positive correlation between the number of risk factors and the incidence of HypoPT. Conclusion (1) Age, BMI, hypertension, MS, mass nature, T stage, CLND, lymph node metastasis, peripheral invasion, and gland lobectomy method will affect the incidence of HypoPT; (2) MS, CLND, mass nature, lymph node metastasis are independent risk factor for HypoPT; (3) There is a positive correlation between the number of risk factor and the incidence of HypoPT. -
Key words:
- Hypoparathyroidism /
- Metabolic syndrome /
- Risk factors
-
表 1 患者临床病理特征比较情况[n(%)/M(P25,P75)]
Table 1. Comparison of clinicopathological characteristics of patients [n%/M(P25,P75)]
临床病理特征 患者甲状旁腺功能情况 Z/χ2 P 减退(n = 105) 正常(n = 121) 年龄 ≥55岁 28(26.7) 14(11.6) 8.468a 0.004* < 55岁 77(73.3) 107(88.4) 性别 女 102(97.1) 117(96.7) 0.038a 1.000 男 3(2.9) 4(3.3) 绝经 是 36(35.3) 29(24.8) 2.883a 0.09 否 66(64.7) 88(75.2) BMI(kg/m2) ≥25 46(43.8) 36(29.8) 4.805a 0.028* < 25 59(56.2) 85(70.2) 高血压 是 22(21.0) 11(9.1) 6.343a 0.012* 否 83(79.0) 110(90.9) MS 是 21(20.0) 10(8.3) 6.542a 0.011* 否 84(80.0) 111(91.7) CLND 无 6(5.7) 16(13.2) 53.308a < 0.001* 单侧 47(44.8) 97(80.2) 双侧 52(49.5) 8(6.6) 淋巴结转移 N0 65(61.9) 93(76.9) 5.977a 0.014* N+ 40(38.1) 28(23.1) 侵犯外周 是 15(14.3) 4(3.3) 8.802a 0.003* 否 90(85.7) 117(96.7) 肿块性质 恶性 62(59.0) 92(76.0) 23.512a < 0.001* 良性 20(19.0) 27(22.3) 恶性+良性 23(21.9) 2(1.7) T分期 T1 72(83.7) 89(94.7) 8.938a 0.031* T2 1(1.2) 2(2.1) T3 6(7.0) 2(2.1) T4 7(8.1) 1(1.1) 甲状腺全切范围 单侧 32(30.5) 111(91.7) 90.785a < 0.001* 双侧 73(69.5) 10(8.3) 旁腺移植 是 23(21.9) 22(18.2) 0.489a 0.485 否 82(78.1) 99(81.8) 雌激素水平 39.3(17.8,91.9) 43.1(25.7,81.5) 1.043 0.297 *P < 0.05;“a”表示连续校正 χ2。 表 2 术后甲状旁腺功能减退多因素分析
Table 2. Multivariate analysis of postoperative hypoparathyroidism
因素 回归系数 标准误 Wald χ2 OR(95%) P MS 1.061 0.513 4.276 2.89(1.057,7.903) 0.039* 无 30.316 0.00* CLND 单侧 0.087 0.63 0.019 1.091(0.317,3.752) 0.89 双侧 2.518 0.716 12.378 12.4(3.05,50.417) 0.00* 良性 11.042 0.004* 肿块性质 恶性 −0.422 0.486 0.752 0.656(0.253,1.7) 0.386 恶性+良性 2.251 0.901 6.237 9.493(1.623,55.523) 0.013* 年龄 0.75 0.467 2.581 2.117(0.848,5.283) 0.108 侵犯外周 0.474 0.723 0.429 1.606(0.389,6.62) 0.512 淋巴结是否转移 0.757 0.402 3.547 2.132(0.97,4.689) 0.06 注:以“未患有MS、无CLND、肿块性质良性、年龄 < 55岁、外周未侵犯、淋巴结未转移”为对照; *P < 0.05。 表 3 危险因素数量的临床特征[n(%)/M(P25,P75)]
Table 3. Clinical characteristics for the number of risk factors [n(%)/M(P25,P75)]
项目 0 1 2 3 4 总计 人数 6(5.7) 42(40.0) 41(39.0) 11(10.5) 5(4.8) 105(100.0) 年龄 50.0(45.5,54.5) 49.0(42,59) 43.0(34.5,51.5) 40.0(36,51)
52. 0(39,66.5) 48.0(38,55) 性别 女 6(100.0) 41(97.6) 41(100.0) 10(90.9) 4(80.0) 102(97.1) 男 0 1(2.4) 0 1(9.1) 1(20.0) 3(2.9) BMI(kg/m2) 24.9(22.3) 24.2(21.9,25.8) 24.6(22.4,26.7) 25.3(21.8,28.1) 23.8(23.2,25.4) 24.3(22.3,26.7) 绝经 是 1(16.7) 20(48.8) 10(24.4) 3(30.0) 2(50.0) 36(52.3) 否 5(83.3) 21(51.2) 31(75.6) 7(70.0) 2(50.0) 66(64.7) 高血压 是 2(33.3) 13(31.0) 4(9.8) 2(18.2) 1(20.0) 22(21.0) 否 4(66.7) 29(69.0) 37(90.2) 9(81.8) 4(80.0) 83(79.0) MS 是 1(16.7) 29(69.0) 5(12.9) 1(9.0) 1(20.0) 21(20.0) 否 5(83.3) 13(31.0) 36(87.8) 10(91.0) 4(80.0) 84(80.0) CLND 无 6(100.0) 0 0 0 0 6(5.7) 单侧 0 23(54.8) 18(43.9) 4(36.4) 2(40.0) 47(44.8) 双侧 0 19(45.2) 23(56.1) 7(63.6) 3(60.0) 52(49.5) PG移植 是 0 0 12(29.3) 6(54.5) 4(100.0) 23(21.9) 否 6(100.0) 42(100.0) 29(70.7) 5(45.5) 0 82(78.1) 侵犯外周 是 0 0 4(9.8) 6(54.5) 5(100.0) 15(14.3) 否 6(100.0) 42(100.0) 37(90.2) 5(45.5) 0 90(85.7) 肿块性质 良性 5(83.3) 12(28.6) 2(4.9) 1(9.1) 0 20(19.0) 恶性 1(16.7) 22(52.4) 31(75.6) 7(63.6) 1(20.0) 62(59.0) 恶性+良性 0 8(19.0) 8(19.5) 3(27.3) 4(80.0) 23(22.0) 腺叶切除 单侧 4(66.7) 4(33.3) 12(29.3) 2(18.2) 0 32(30.5) 双侧 2(33.3) 28(66.7) 29(70.7) 9(81.8) 5(100.0) 73(69.5) 淋巴结转移 是 0 0 25(61.0) 10(90.9) 5(100.0) 40(38.1) 否 6(100.0) 42(100.0) 16(39.0) 1(9.1) 0 65(61.9) 注:4个主要的危险因素:VI区淋巴结的清扫,淋巴结是否转移,外周是否侵犯,甲状旁腺是否自体移植;*P < 0.05。 表 4 HypoPT与危险因素数量关系多因素分析
Table 4. Multivariate analysis of the relationship between HypoPT and the number of risk factors
危险因素个数 未校正 校正 P OR(95%CI) P OR(95%CI) 0 0.042 参考值 0.019 参考值 1 0.385 1.581(0.562~4.443) 0.508 1.501(0.451~4.992) 2 0.095 2.453(0.857~7.024) 0.035 4.023(1.1~14.711) 3 0.025 5.133(1.234~21.355) 0.025 6.579(1.271~34.059) 4 0.04 11.667(1.112~122.381) 0.235 5.475(0.331~90.623) 注:危险因素个数为0个为参考项;纳入年龄、肿块性质、MS为混杂因素经行校正。 -
[1] 中华人民共和国国家卫生健康委员会 . 甲状腺癌诊疗规范(2018年版)[J]. 中华普通外科学文献(电子版), 2019, 13(1): 1-15. [2] 朱精强,田文,苏安平. 甲状腺围手术期甲状旁腺功能保护指南(2018版)[J]. 中国实用外科杂志,2018,38(10):1108-1113. doi: 10.19538/j.cjps.issn1005-2208.2018.10.03 [3] Imga N N,Atas H,Torgutalp M,et al. Stratifying the risk factors for hypoparathyroidism after total thyroidectomy. A single center’ study[J]. Ann Ital Chir,2019,90(1):21-30. [4] 欧亮,赵志泓,孙振华,等. 甲状腺乳头状癌术后甲状旁腺功能减退发生情况及严重程度的相关风险分析[J]. 江苏医药,2021,47(8):772-776. doi: 10.19460/j.cnki.0253-3685.2021.08.005 [5] Qiu Y,Xing Z,Fei Y,et al. Role of the 2018 American thyroid association statement on postoperative hypoparathyroidism:A 5-year retrospective study[J]. BMC Surg,2021,21(1):334. doi: 10.1186/s12893-021-01333-w [6] D í ez J J,Anda E,Sastre J,et al. Recovery of parathyroid function in patients with thyroid cancer treated by total thyroidectomy:An analysis of 685 patients with hypoparathyroidism at discharge of surgery[J]. Endocrinol Diabetes Nutr (Engl Ed),2021,68(6):398-407. [7] Mencio M,Calcatera N,Ogola G,et al. Factors contributing to unintentional parathyroidectomy during thyroid surgery[J]. Proc (Bayl Univ Med Cent),2019,33(1):19-23. [8] Salem FA,Bergenfelz A,Nordenström E,et al. Central lymph node dissection and permanent hypoparathyroidism after total thyroidectomy for papillary thyroid cancer:Population-based study[J]. Br J Surg,2021,108(6):684-690. [9] Chen Z, Zhao Q, Du J, et al. Risk factors for postoperative hypocalcaemia after thyroidectomy: A systematic review and meta-analysis[J]. J Int Med Res, 2021, 49(3):1-21. [10] Ru Z,Mingliang W,Maofei W,et al. Analysis of risk factors for hypoparathyroidism after total thyroidectomy[J]. Front Surg,2021,8(21):668-672. [11] Su A,Wang B,Gong Y,et al. Risk factors of hypoparathyroidism following total thyroidectomy with central lymph node dissection[J]. Medicine (Baltimore),2017,96(39):e8162. [12] 冯洪雨. 代谢综合征与甲状腺癌的相关性研究[D]. 唐山: 华北理工大学硕士学位论文, 2020. [13] Orloff LA,Wiseman SM,Bernet VJ,et al. American thyroid association statement on postoperative hypoparathyroidism:Diagnosis,prevention,and management in adults[J]. Thyroid,2018,28(7):830-841. doi: 10.1089/thy.2017.0309 [14] 徐国栋,凌煜玮,朱江,等. 甲状腺癌术后迁延性甲状旁腺功能减退风险的列线图预测模型研究[J]. 中国普外基础与临床杂志,2022,29(1):24-31. [15] Fanget F,Demarchi MS,Maillard L,et al. Hypoparathyroidism:Consequences,economic impact,and perspectives. A case series and systematic review[J]. Ann Endocrinol (Paris),2021,82(6):572-581. doi: 10.1016/j.ando.2021.07.085 [16] 田文,张浩. 甲状腺外科能量器械应用专家共识(2017版)[J]. 中国实用外科杂志,2017,37(9):992-997. doi: 10.19538/j.cjps.issn1005-2208.2017.09.14 [17] Sitges-Serra A. Etiology and diagnosis of permanent hypoparathyroidism after total thyroidectomy[J]. J Clin Med,2021,10(3):543. doi: 10.3390/jcm10030543 [18] Tian W,Jiang Y,Gao B,et al. Application of nano-carbon in lymph node dissection for thyroid cancer and protection of parathyroid glands[J]. Med Sci Monit,2014,20(10):1925-1930. [19] Qiu Y,Xing Z,Xiang Q,et al. Duration of parathyroid function recovery in patients with protracted hypoparathyroidism after total thyroidectomy for papillary thyroid carcinoma[J]. Frontiers in Endocrinology,2021,12(4):665-673. [20] Lorente-Poch L,Sancho J J,Ruiz S,et al. Importance of in situ preservation of parathyroid glands during total thyroidectomy[J]. Br J Surg,2015,102(4):359-367. doi: 10.1002/bjs.9676 -






 下载:
下载: