Prediction of Delivery Mode by Transperineal Ultrasound during the Active Phase of the First Stage Labor
-
摘要:
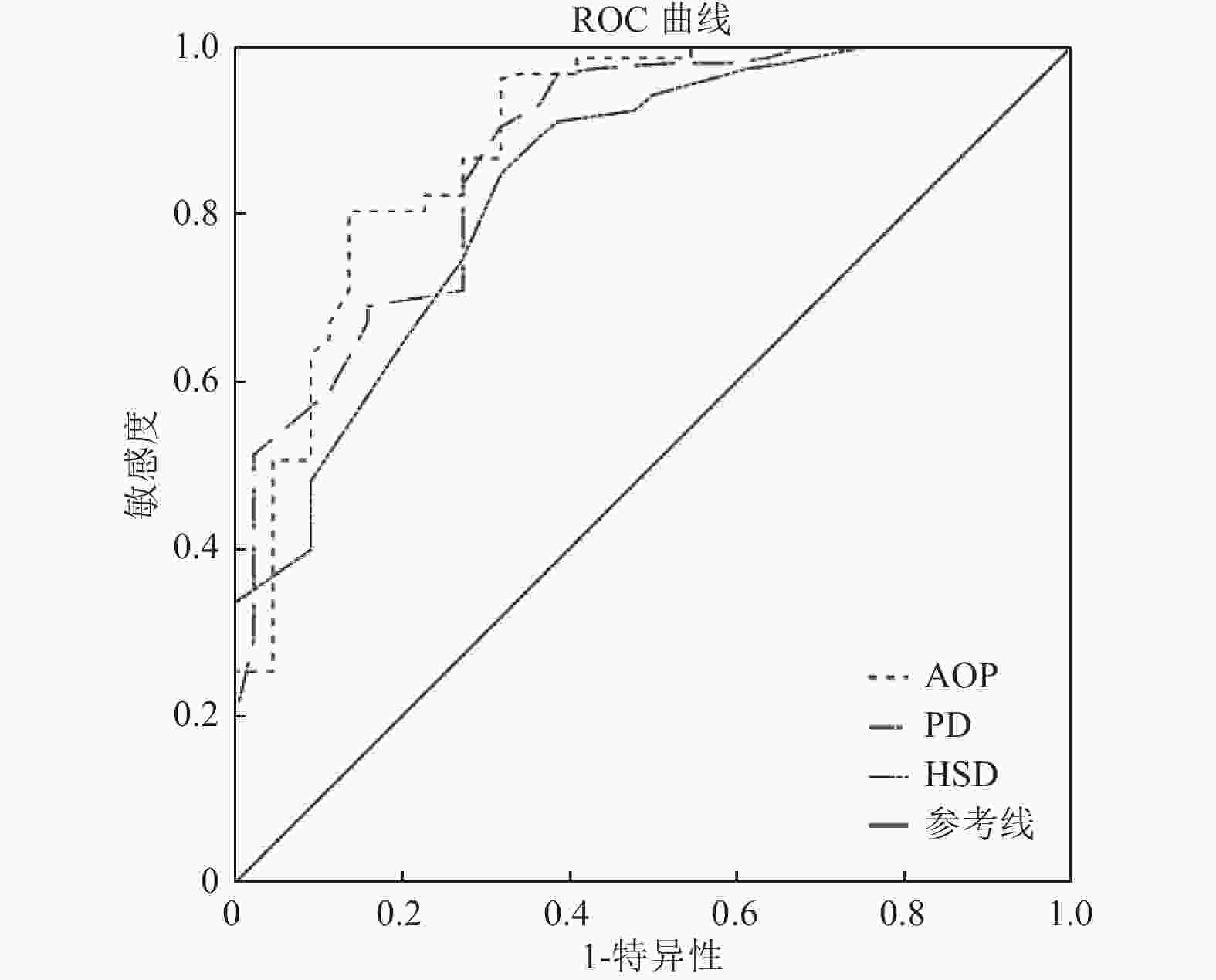
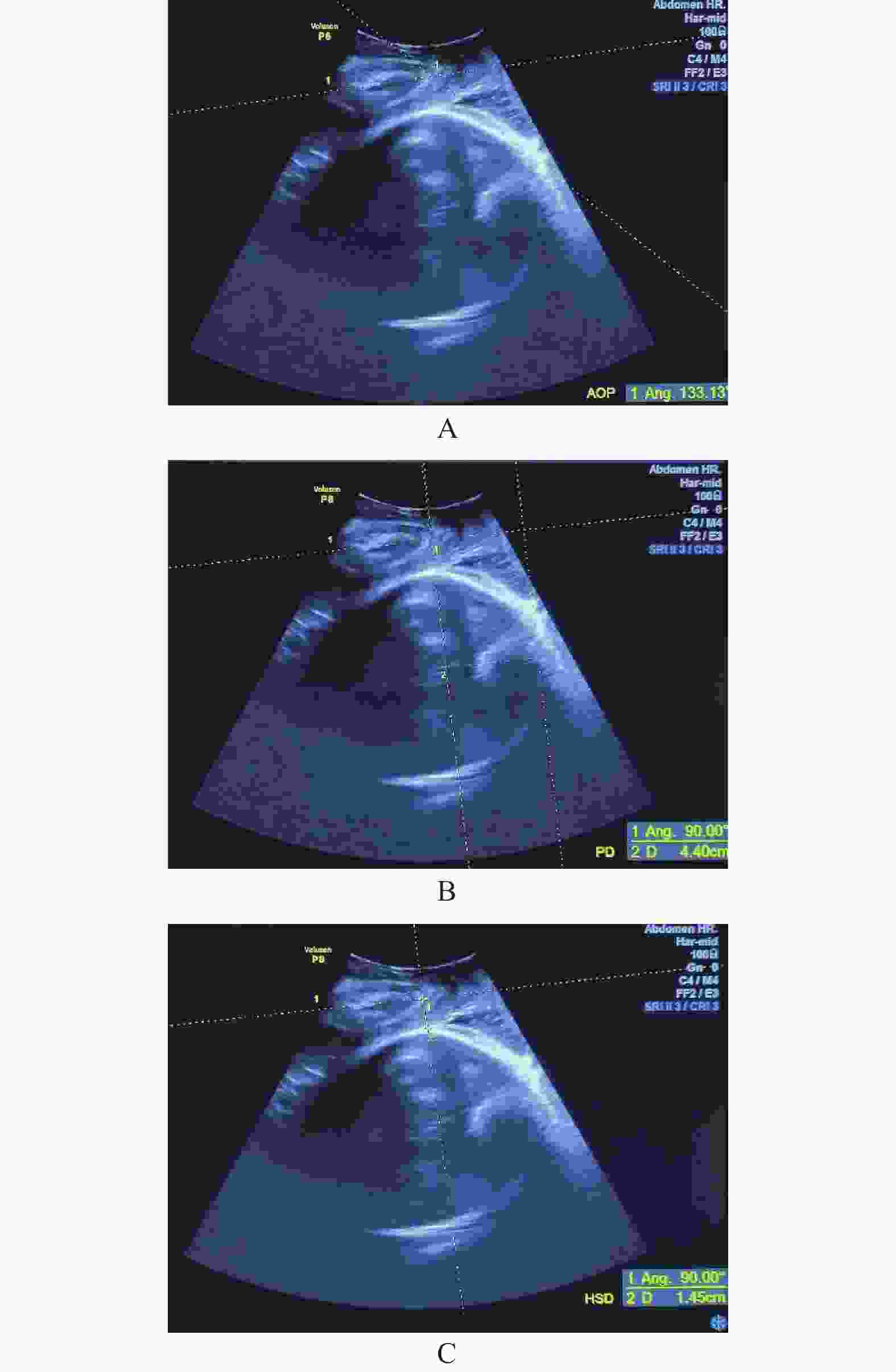
目的 探讨第一产程活跃期时产程进展角(angle of progression,AOP)、胎头下降距离(progression distance,PD)、胎头至耻骨联合距离(head-symphysis distance,HSD)等产程进展参数对分娩方式的预测价值。 方法 选取2020年7月到2021年12月在云南省第一人民医院产科经阴道试产的初产妇作为研究对象,在第一产程活跃期测量其AOP、PD、HSD,比较阴道分娩组与剖宫组之间上述参数的差异,应用ROC曲线分析各产程进展参数对孕妇分娩方式的预测价值。 结果 阴道分娩组孕妇在第一产程活跃期AOP及PD明显大于剖宫产组,[(141.09±9.87)° vs (122.84±10.70)°]、[(4.28±0.48) cm vs (3.18±0.83) cm],而HSD阴道分娩组则明显小于剖宫产组[(1.42±0.40) cm vs( 2.18±0.64) cm],差异均有统计学意义(P < 0.001);ROC曲线分析显示,AOP、PD、HSD预测阴道分娩的曲线下面积分别为0.892、0.875、0.840,差异均有统计学意义(P < 0.001)。 结论 对经阴道试产初产妇,第1产程活跃期AOP、PD及HSD的测量对分娩方式具有预测价值。 Abstract:Objective To investigate the value of angle of progression progression (AOP), fetal head descent distance (PD) and fetal head to pubic symphysis (HSD) in predicting the mode of delivery during the active phase of the first stage of labor. Methods The AOP, PD and HSD were measured at the active phase of the first stage of labor. The difference of these parameters was compared between the vaginal delivery group and the cesarean section group. Results The AOP and PD in vaginal delivery group were significantly higher than those in cesarean delivery group (141.09° ±9.87° vs 122.84° ±10.70° , 4.28 cm ± 0.48 cm vs 3.18 cm ± 0.83 cm), while HSD in vaginal delivery group were significantly lower than that in cesarean delivery group (1.42 cm ± 0.40 cm vs 2.18 cm ± 0.64 cm) (P < 0.001). The AUC of AOP, PD and HSD for predicting vaginal delivery was 0.892, 0.875 and 0.840, respectively, with statistical significance (P < 0.001). Conclusion The measurement of AOP, PD and HSD in the active phase of the first stage of labor has the predictive value for the mode of delivery in nulliparous women. -
Key words:
- Ultrasound /
- Labor /
- Delivery mode /
- AOP /
- PD /
- HSD
-
表 1 阴道分娩组和剖宫产组之间一般情况的比较(
$\bar x \pm s $ )Table 1. The difference of basic characteristics between the vaginal delivery group and the cesarean section group (
$\bar x \pm s $ )临床特征 阴道分娩组 剖宫产组 t P 年龄(岁) 28.67 ± 3.51 28.84 ± 4.12 −0.273 0.785 体重(kg) 67.90 ± 9.24 67.97 ± 6.78 −0.042 0.966 体重指数(kg/m2) 26.36 ± 3.40 26.93 ± 2.65 −1.021 0.309 胎儿头围(cm) 32.60 ± 1.17 33.02 ± 0.93 −2.234 0.027* 出生体重(g) 3232 ± 396 3429 ± 378 −2.945 0.004* * P < 0.05。 表 2 阴道分娩组和剖宫产组之间各产程进展参数的比较(
$\bar x \pm s $ )Table 2. The difference of labor progression parameters between the vaginal delivery group and the cesarean section group (
$\bar x \pm s $ )组别 AOP(°) PD(cm) HSD(cm) 阴道分娩组
(n = 158)141.09 ± 9.87 4.28 ± 0.48 1.42 ± 0.40 剖宫产组
(n = 44)122.84 ± 10.70 3.18 ± 0.83 2.18 ± 0.64 t 10.64 11.25 −9.69 P < 0.001* < 0.001* < 0.001* *P < 0.05。 表 3 产程进展参数对分娩方式(阴道分娩)的预测效能
Table 3. The value of these parameters in predicting the mode of delivery
产程进展参数 AUC 截断值 灵敏度
(%)特异度
(%)P 95%置信区间 下限 上限 AOP 0.892 132.95° 80.4 86.4 < 0.001* 0.833 0.951 PD 0.875 3.65 cm 90.5 68.2 < 0.001* 0.816 0.934 HSD 0.840 1.75 cm 84.8 68.2 < 0.001* 0.773 0.907 *P < 0.05。 -
[1] Dupuis O,Silveira R,Zentner A,et al. Birth simulator:Reliability of transvaginal assessment of fetal head station as defined by the American college of obstetricians and gynecologists classification[J]. Am J Obstet Gynecol,2005,192(3):868-874. doi: 10.1016/j.ajog.2004.09.028 [2] Wiafe Y A,Whitehead B,Venables H,et al. The effectiveness of intrapartum ultrasonography in assessing cervical dilatation,head station and position:A systematic review and Meta-analysis[J]. Ultrasound,2016,24(4):222-232. doi: 10.1177/1742271X16673124 [3] Ghi T,Eggebø T,Lees C,et al. ISUOG Practice guidelines:Intrapartum ultrasound[J]. Ultrasound Obstet Gynecol,2018,52(1):128-139. doi: 10.1002/uog.19072 [4] Barbera A F,Pombar X,Perugino G,et al. A new method to assess fetal head descent in labor with transperineal ultrasound[J]. Ultrasound Obstet Gynecol,2009,33(3):313-319. [5] Bamberg C,Scheuermann S,Slowinski T,et al. Relationship between fetal head station established using an open magnetic resonance imaging scanner and the angle of progression determined by transperineal ultrasound[J]. Ultrasound Obstet Gynecol,2011,37(6):712-716. doi: 10.1002/uog.8944 [6] Kahrs B H,Usman S,Ghi T,et al. Sonographic prediction of outcome of vacuum deliveries:A multicenter,prospective cohort study[J]. Am J Obstet Gynecol,2017,217(1):69.e1-69.e10. doi: 10.1016/j.ajog.2017.03.009 [7] Wiafe Y A,Whitehead B,Venables H,et al. Sonographic parameters for diagnosing fetal head engagement during labour[J]. Ultrasound,2018,26(1):16-21. doi: 10.1177/1742271X18755080 [8] Eggebø T M,Hassan W A,Salvesen K Å,et al. Sonographic prediction of vaginal delivery in prolonged labor:A two- center study[J]. Ultrasound Obstet Gynecol,2014,43(2):195-201. doi: 10.1002/uog.13210 [9] Torkildsen E A,Salvesen K A,Eggebo T M. Prediction of delivery mode with transperineal ultrasound in women with prolonged first stage of labour[J]. Ultrasound Obstet Gynecol,2011,37(6):702-708. doi: 10.1002/uog.8951 [10] Kohls F,Brodowski L,Kuehnle E,et al. Intrapartum translabial ultrasound:A systematic analysis of the fetal head station in the first stage of labor[J]. Z Geburtshilfe Neonatol,2018,222(1):19-24. doi: 10.1055/s-0043-122242 [11] Chor C M,Poon L,Leung T Y. Prediction of labor outcome using serial transperineal ultrasound in the first stage of labor[J]. J Matern Fetal Neonatal Med,2019,32(1):31-37. doi: 10.1080/14767058.2017.1369946 [12] Dall'Asta A,Angeli L,Masturzo B,et al. Prediction of spontaneous vaginal delivery in nulliparous women with a prolonged second stage of labor:The value of intrapartum ultrasound[J]. Am J Obstet Gynecol,2019,221(6):642. [13] Yonetani N,Yamamoto R,Murata M,et al. Prediction of time to delivery by transperineal ultrasound in second stage of labor[J]. Ultrasound Obstet Gynecol,2017,49(2):246-251. doi: 10.1002/uog.15944 [14] Kasbaoui S,Séverac F,Aïssi G,et al. Predicting the difficulty of operative vaginal delivery by ultrasound measurement of fetal head station[J]. Am J Obstet Gynecol,2017,216(5):507. [15] Sainz J A,García-Mejido J A,Aquise A,et al. A simple model to predict the complicated operative vaginal deliveries using vacuum or forceps[J]. Am J Obstet Gynecol,2019,220(2):193.e1-193.e12. doi: 10.1016/j.ajog.2018.10.035 [16] Bibbo C,Rouse C E,Cantonwine D E,et al. Angle of progression on ultrasound in the second stage of labor and spontaneous vaginal delivery[J]. Am J Perinatol,2018,35(4):413-420. [17] Ghi T,Contro E,Farina A,et al. Three-dimensional ultrasound in monitoring progression of labor:A reproducibility study[J]. Ultrasound Obstet Gynecol,2010,36(4):500-506. doi: 10.1002/uog.7752 [18] 田雪叶,韩蓁,全萌,等. 经会阴三维超声监测产程进展各参数的可重复性研究[J]. 西安交通大学学报:医学版,2018,39(6):5. [19] 中华医学会妇产科学分会产科学组. 新产程标准及处理的专家共识(2014)[J]. 中华妇产科杂志,2014,49(7):486. doi: 10.3760/cma.j.issn.0529-567x.2014.07.002 -





 下载:
下载: