The Expression of PD-L1, BRAFV600E, CD68 Protein and the Significance of Tumor Infiltrating Lymphocytes in the Diagnosis of Malignant Melanoma
-
摘要:
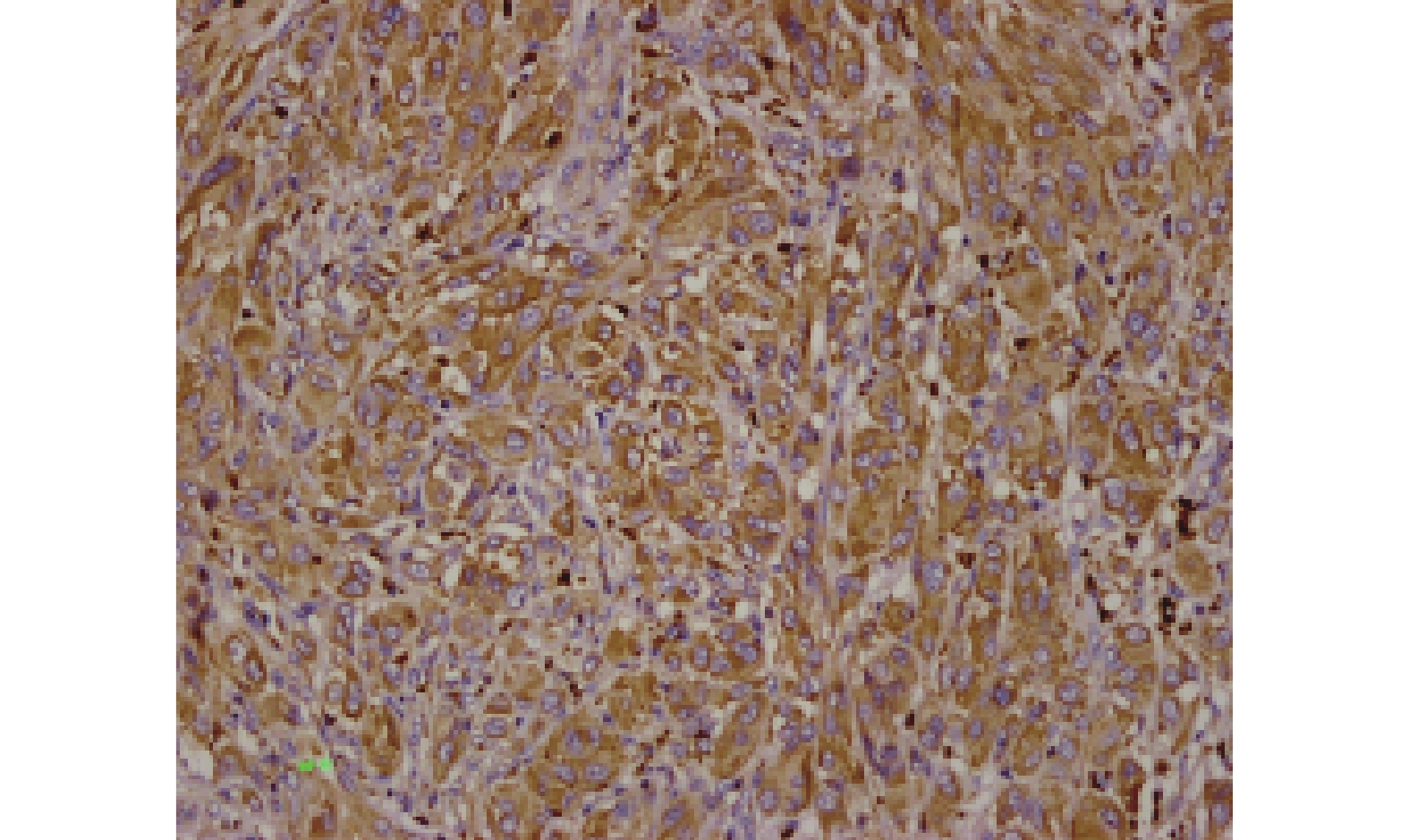
目的 分析PD-L1、BRAFV600E、CD68蛋白和肿瘤浸润淋巴细胞(TIL)在恶性黑色素瘤诊断中的意义。 方法 应用高通量组织芯片技术及免疫组化方法,检测60例原发性恶性黑色素瘤组织中PD-L1、BRAFV600E、CD68蛋白表达;分析PD-L1、BRAFV600E、CD68蛋白以及TIL与患者的临床病理特征及预后关系。 结果 (1)恶性黑色素瘤组织中CD68蛋白表达与肿瘤T分期之间,差异有统计学意义(P = 0.018),而与肿瘤大小、肿瘤浸润深度、淋巴结转移和溃疡形成之间,差异均无统计学意义(P > 0.05);(2)PD-L1、BRAFV600E和TIL与肿瘤T分期、肿瘤大小、肿瘤浸润深度、淋巴结转移和溃疡形成之间,差异均无统计学意义(P > 0.05);(3)皮肤黑色素瘤BRAFV600E突变率约36.67%(22/60),其中,肢端型黑色素瘤BRAFV600E突变率约68.18%(15/22);黏膜黑色素瘤BRAFV600E突变率约23.33%(14/60);(4)Cox回归生存分析结果显示肿瘤淋巴结转移是影响恶性黑色素瘤患者预后的因素。 结论 (1)CD68蛋白表达在判定患者预后方面可能有一定作用;(2)皮肤部位的黑色素瘤建议行BRAFV600E免疫组化检测;(3)患者存在淋巴结转移可作为恶性黑色素瘤预后判断的参考指标。 Abstract:Objective To analyze the significance of PD-L1, BRAFV600E, CD68 protein expressions and tumor infiltrating lymphocytes (TIL) in the diagnosis of malignant melanoma. Methods High-throughput tissue microarray technology and immunohistochemical methods were used to detect the expressions of PD-L1, BRAFV600E and CD68 in 60 primary malignant melanoma tissues. The relationship between PD-L1, BRAFV600E, CD68 expressions, TIL and the clinicopathological characteristics and prognosis of patients was analyzed. Results (1) There was a statistically significant difference between CD68 expression in malignant melanoma tissue and tumor T stage (P = 0.018), but no statistical difference between tumor size, tumor invasion depth, lymph node metastasis and ulceration (P > 0.05). (2) There was no significant difference between PD-L1, BRAFV600E, TIL and tumor T stage, tumor size, tumor invasion depth, lymph node metastasis and ulceration (P > 0.05). (3) The mutation rate of BRAFV600E in cutaneous melanoma was about 36.67% (22/60). The mutation rate of BRAFV600E in cutaneous acral melanoma was about 68.18%. (15/22). The mutation rate of BRAFV600E in mucosal melanoma was about 23.33% (14/60). (4) Cox regression analysis showed that lymph node metastasis was the prognostic factor of malignant melanoma patients. Conclusion (1) The expression of CD68 protein may play a role in determining the prognosis of patients. (2) BRAFV600E immunohistochemical detection is recommended for melanoma in the skin. (3) The presence of lymph node metastasis in patients can be used as a reference index for the prognosis of malignant melanoma. -
Key words:
- Malignant Melanoma /
- PD-L1 /
- BRAFV600E /
- CD68 /
- TIL /
- Immunohistochemistry
-
表 1 多因素 COX比例风险回归模型
Table 1. Multivariate COX proportional hazards regression model
影响因素 β SE Wald P RR 95%CI 转移 0.926 0.451 4.225 0.040 2.524 1.044~6.105 -
[1] Christopher P Wild, Elisabete Weiderpass, Bernard W Stewart. World cancer report-cancer research for cancer prevention[M]. Lyon: World Health Organization, 2020: 374-381. [2] Edge S B, Byrd D R, Compton C C, et al. AJCC cancer staging manual (7th ed) [M]. New York: Springer International Publishing, 2010: 325-344. [3] Liu X,Zheng S P,Peng Y,et al. Construction of the prediction model for locally advanced rectal cancer following neoadjuvant chemoradiotherapy based on pretreatment tumor-infiltrating macrophage-associated biomarkers[J]. OncoTargets and Therapy,2021,14:2599-2610. [4] 刘伟,安杰,侯会池,等. H l F-1 0c及CD68在胃癌组织中的表达及其临床意义[J]. 中国现代普通外科进展,2014,17(7):516-519. [5] Atefi M,Avramis E,Lassen A,et al. Effects of MAPK and PI3K pathways on PD-L1 expression in melanoma[J]. Clinical Cancer Research,2014,20(13):3446-3457. doi: 10.1158/1078-0432.CCR-13-2797 [6] Kim J W, Eder J P. Prospects for targeting PD-1 and PD-L1 in various tumor types [J]. Oncology, 2014, 28 (Suppl 3): 15-28. [7] Park S J,Namkoong H,Doh J,et al. Negative role of inducible PD-1 on survival of activated dendritic cells[J]. J Leukoc Biol,2014,95(4):621-629. doi: 10.1189/jlb.0813443 [8] Merelli B,Massi D,Cattaneo L,et al. Targeting the PD1/PD-L1 axis in melanoma:Biological rationale,clinical challenges and opportunities[J]. Critical Reviews in Oncology/Hematology,2014,89(1):140-165. doi: 10.1016/j.critrevonc.2013.08.002 [9] 林喜娜,李广秋,何萍,等. 非小细胞肺癌中PD-L1表达及其与肺癌相关驱动基因的关系[J]. 临床与实验病理学杂志,2019,35(7):767-771. doi: 10.13315/j.cnki.cjcep.2019.07.003 [10] 黄育刚,王 莉,汤显斌. PD-1/PD-L1免疫抑制剂在肺癌临床治疗和病理检测中的研究进展[J]. 临床与实验病理学杂志,2020,36(6):688-692. [11] Massi D,Brusa D,Merelli B,et al. PD-L1 marks a subset of melanomas with a shorter overall survival and distinct genetic and morphological characteristics[J]. Annals of Oncology,2014,25(12):2433-2442. doi: 10.1093/annonc/mdu452 [12] Gadiot J,Hooijkaas A I,Kaiser A D M,et al. Overall survival and PD-L1 expression in metastasized malignant melanoma[J]. Cancer,2011,117(10):2192-2201. doi: 10.1002/cncr.25747 [13] de Souza Malaspina T S,Gasparoto T H,Costa M R S N,et al. Enhanced programmed death 1 (PD-1) and PD-1 ligand (PD-L1) expression in patients with actinic cheilitis and oral squamous cell carcinoma[J]. Cancer Immunology,Immunotherapy,2011,60(7):965-974. [14] Muenst S,Schaerli A R,Gao F,et al. Expression of programmed death ligand 1 (PD-L1) is associated with poor prognosis in human breast cancer[J]. Breast Cancer Research and Treatment,2014,146(1):15-24. doi: 10.1007/s10549-014-2988-5 [15] 冯昌银,郑巧灵,黄建平. 等 结直肠癌肿瘤原发灶与肝脏转移灶中PD-L1表达的差异性[J]. 临床与实验病理学杂志,2018,34(12):1340-1343. [16] Pinto C A,Liu Xinyue,Li Xiaoyun,et al. Treatment and overall survival among anti-PD-1-exposed advanced melanoma patients with evidence of disease progression[J]. Immunotherapy,2022,14(4):201-214. [17] Flaherty K T,Puzanov I,Kim K B,et al. Inhibition of mutated,activated BRAF in metastatic melanoma[J]. New England Journal of Medicine,2010,363(9):809-819. doi: 10.1056/NEJMoa1002011 [18] 黄志敏,吴一龙. 非小细胞肺癌的BRAF基因突变及其临床意义[J]. 中国肺癌杂志,2012,15(3):183-186. doi: 10.3779/j.issn.1009-3419.2012.03.09 [19] Feller J K,Yang S,Mahalingam M. Immunohistochemistry with a mutation- specific monoclonal antibody as a screening tool for the BRAFV600E mutational status in primary cutaneous malignant melanoma[J]. Mod Pathol,2013,26(3):414-420. doi: 10.1038/modpathol.2012.168 [20] Halapi E. Oligoclonal T cells in human cancer[J]. Med Oncol,1998,15(4):203-211. doi: 10.1007/BF02787202 [21] Rosenberg S A,Restifo N P,Yang J C,et al. Adoptive cell transfer:A clinical path to effective cancer immunotherapy[J]. Nature Reviews Cancer,2008,8(4):299-308. doi: 10.1038/nrc2355 [22] Wang R,Zhang J,Chen S,et al. Tumor-associated macrophages provide a suitable microenvironment for non-small lung cancer invasion and progression[J]. Lung Cancer,2011,74(2):188-196. doi: 10.1016/j.lungcan.2011.04.009 [23] Leek R D,Lewis C E,Whitehouse R,et al. Association of macrophage infiltration with angiogenesis and prognosis in invasive breast carcinoma[J]. Cancer Res,1996,56(20):4625-4629. -






 下载:
下载: