Study on the Correlation between Late-onset Breast Milk Jaundice and Defecation Frequency in Infants
-
摘要:
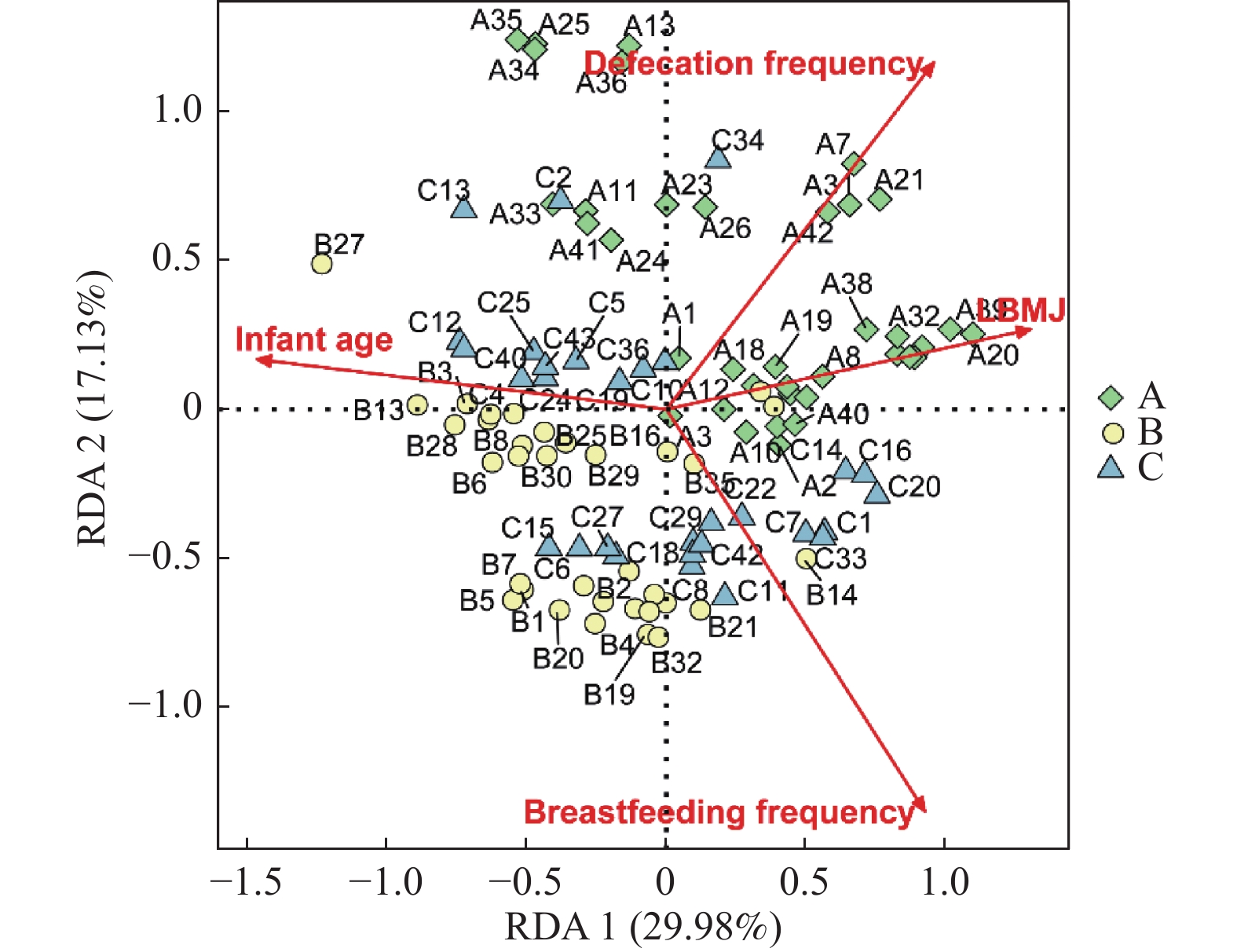
目的 研究迟发型母乳性黄疸(LBMJ)的相关性因素,为LBMJ病因研究提供参考依据。 方法 选取昆明医科大学第一临床学院0~6月龄纯母乳喂养足月儿102例,根据不同排便频次分为排便频次增多组,即排便 > 3次/d(A组,n = 37);排便频次减少组,即超过4 d排便1次(B组,n = 34);排便频次正常组,即3d以内排便1次或排便≤3次/d(C组,n = 31);选取的黄疸患儿均为LBMJ,分析LBMJ婴儿和其排便频次及日龄、喂养频次之间的相关性。 结果 (1)纯母乳喂养婴儿的日龄与其不同排便频次差异有统计学意义(Hc = 7.8007,P = 0.0202);排便频次改变与有无LBMJ差异无统计学意义(χ2 = 5.8649,P = 0.0533),但经趋势性卡方检验发现LBMJ的发生率随着排便次数的增多而增高(χ2 = 5.7593,P = 0.0164);(2)LBMJ与婴儿排便频次和喂养频率呈正相关,并且以上因素均与婴儿日龄呈负相关。 结论 0~6月龄婴儿日龄越小,母乳喂养的频次越多,排便频次也越多,LBMJ发生率越高;另外,LBMJ的胆红素肠肝循环途径增强与婴儿的排便频次增多相关性较小。 Abstract:Objective To analyze the correlation factors of late-onset breast-feeding jaundice (LBMJ), and provide the reference for the study of LBMJ etiology. Methods 102 full-term breast-fed infants aged 0-6 months from the First Affiliated Hospital of Kunming Medical University were selected as the participants of this study and according to their defecation frequency they were divided respectively into defecation frequency increased group or group A, i.e. defecation > 3 times / D ( n = 37), decreased defecation frequency group or group B, i.e. one defecation in more than 4 days (n = 34) and the normal group or group C, i.e. defecating once within 3 days or 3 times a day (n = 31). All the infants with jaundice were LBMJ and the correlation between LBMJ and defecation frequency, age and feeding frequency was analyzed. Results 1. There was a statistical difference between the age of exclusively breast-fed infants and their different defecation frequency (Hc =7.8007, P = 0.0202). There was no significant difference between the change of defecation frequency and the absence of LBMJ (χ2 = 5.8649, P = 0.0533), but the incidence of LBMJ increased with the increase of defecation frequency (χ2 =5.7593, P = 0.0164). 2. LBMJ was positively correlated with the defecation frequency and feeding frequency in infants, and the above factors were negatively correlated with the age of infants. Conclusion The younger the infants aged from 0 to 6 months, the more frequent the breastfeeding, the more frequent the defecation and the higher the incidence of LBMJ. In addition, the enhancement of bilirubin enterohepatic circulation pathway in LBMJ has little correlation with the increased defecation frequency in infants. -
Key words:
- Late-onset breast milk jaundice /
- Infant /
- Defecation frequency /
- Breast feeding /
- Factor analysis.
-
表 1 不同排便频次纯母乳喂养婴儿的一般情况比较
Table 1. Comparison of the general situation of infants who were exclusively breastfed at different defecation frequencies
组别日龄(d)
M(P25,P75)性别(n) 迟发型母乳性黄疸(n) 母乳喂养频次(n) 男 女 有 无 频次较多 频次正常 频次少 频次极少 A 50(38,94) 21 16 12 25 24 10 3 0 B 90(50,150) 19 15 3 31 16 17 1 0 C 56(42,120) 15 16 7 24 18 10 3 0 Hc/χ2 7.801 0.555 5.865 5.064 P 0.020* 0.758 0.053 0.281 *P < 0.05。 -
[1] 绍肖梅,叶鸿瑁,丘小汕. 实用新生儿学[J]. 北京:人民出版社,2019:455-456. [2] Weng Y H,Cheng S W,Yang C Y,et al. Risk assessment of prolonged jaundice in infants at one month of age:A prospective cohort study[J]. Scientific Reports,2018,8(1):14824. doi: 10.1038/s41598-018-33249-6 [3] 孙雨,周炳文,缪东幸. 母乳性黄疸发病机制的研究进展[J]. 医学综述,2013,19(11):1963-1966. doi: 10.3969/j.issn.1006-2084.2013.11.014 [4] 朱琳涵. 母乳性黄疸的诊断和治疗[J]. 中国医刊,2016,51(6):1-4. doi: 10.3969/j.issn.1008-1070.2016.06.001 [5] 杨英莲,陈贻骥. 母乳性黄疸发病机制研究进展[J]. 重庆医学,2013,42(14):1659-1661. doi: 10.3969/j.issn.1671-8348.2013.14.037 [6] 贾尔肯阿依·阿不都拉依,寇新红,陈凤娟,等. 迟发型母乳性黄疸患儿肠道菌群特征研究[J]. 中国妇幼卫生杂志,2022,13(1):57-61. doi: 10.19757/j.cnki.issn1674-7763.2022.01.012 [7] Xiao L L,Zhang X F,Wang X Y. Changes in epidermal growth factor concentrations in neonates with late-onset breast milk jaundice after stopping breast feeding[J]. Zhong Guo Dang Dai Er Ke Za Zhi,2013,15(12):1079-1081. [8] 杨晓云,张林,朱自伟. 新生儿黄疸消退延迟的相关因素分析[J]. 中国医药指南,2017,15(19):30-31. doi: 10.15912/j.cnki.gocm.2017.19.019 [9] Weng Y H,Chiu Y W,Cheng S W. Breast milk jaundice and maternal diet with chinese herbal medicines[J]. Evid Based Complement Alternat Med,2012,2012:150120. doi: 10.1155/2012/150120 [10] Elmassry M M,Kim S,Busby B. Predicting drug-metagenome interactions:Variation in the microbial β-glucuronidase level in the human gut metagenomes[J]. PLoS One,2021,16(1):e0244876. doi: 10.1371/journal.pone.0244876 [11] Yang Y Y,Tsai T H. Enterohepatic circulation and pharmacokinetics of genistin and genistein in rats[J]. ACS Omega,2019,4(19):18428-18433. doi: 10.1021/acsomega.9b02762 [12] Little M S,Pellock S J,Walton W G,et al. Structural basis for the regulation of β-glucuronidase expression by human gut enterobacteriaceae[J]. Proc Natl Acad Sci U S A,2018,115(2):E152-e161. [13] Zhou S,Wang Z,He F,et al. Association of serum bilirubin in newborns affected by jaundice with gut microbiota dysbiosis[J]. The Journal of Nutritional Biochemistry,2018,63(9):54-61. doi: 10.1016/j.jnutbio.2018.09.016.Epub2018Sep26 [14] 茹彩旺,秦涛,王玲,等. 母乳和新生儿粪便细菌与母乳性黄疸的相关性分析[J]. 中国微生态学杂志,2015,27(3):325-327. doi: 10.13381/j.cnki.cjm.201503020 [15] 李亚璇. 母乳外泌体miRNA调节肠道菌群与母乳性黄疸的相关机制研究[D]. 上海: 上海交通大学硕士论文, 2019. [16] Apaydin K,Ermis B,Arasli M,et al. Cytokines in human milk and late-onset breast milk jaundice[J]. Pediatr Int,2012,54(6):801-805. doi: 10.1111/j.1442-200X.2012.03680.x [17] Nagao Y,Ohsawa M,Kobayashi T. Correlation between unconjugated bilirubin and total cholesterol in the sera of 1-month-old infants[J]. J Paediatr Child Health,2010,46(12):709-713. doi: 10.1111/j.1440-1754.2010.01826.x -






 下载:
下载: