Risk Factors Analysis and Prediction Model Establishment of Refeeding Syndrome in ICU Patients with Sepsis
-
摘要:
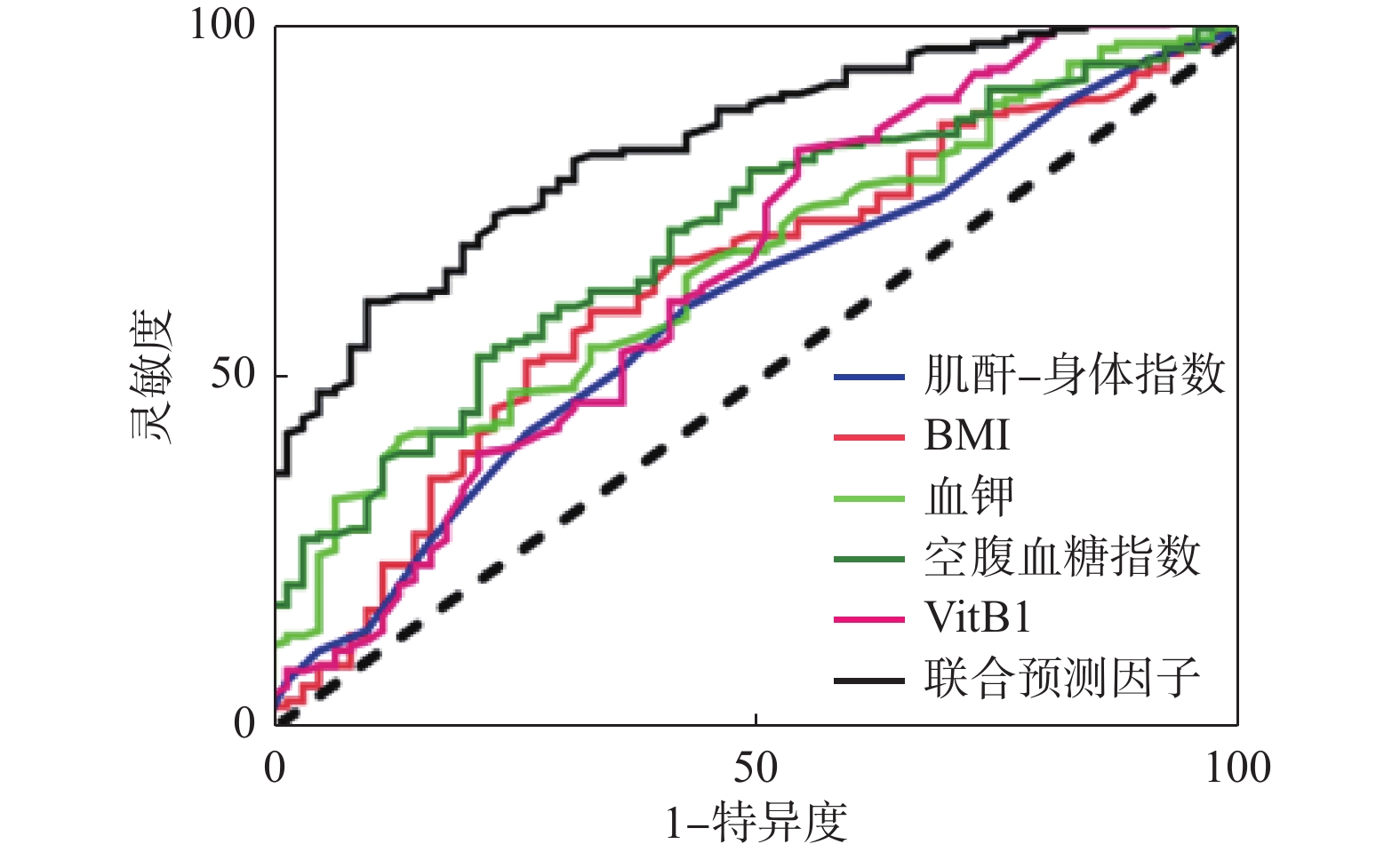
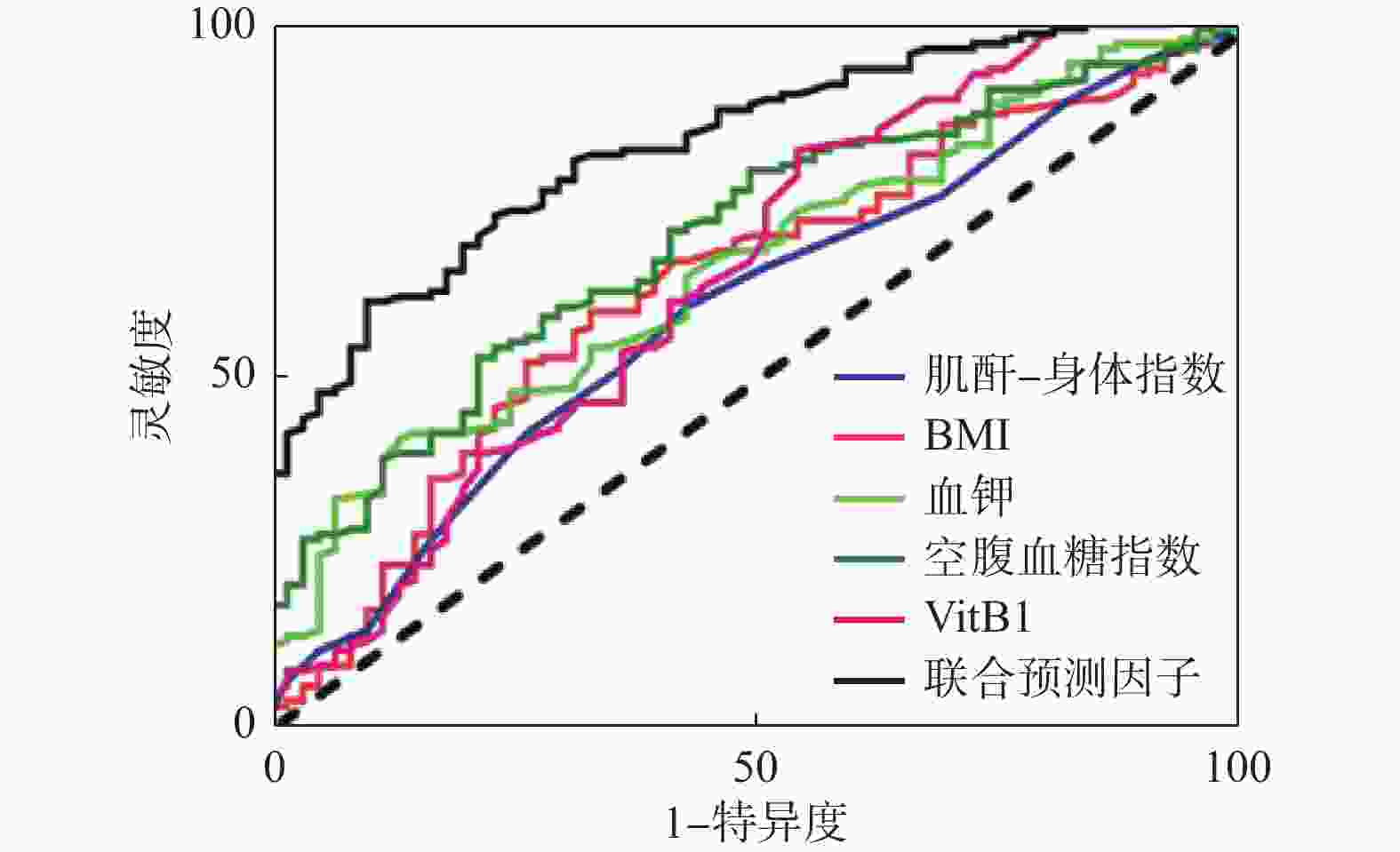
目的 探讨ICU脓毒症患者发生再喂养综合征(RFS)的相关危险因素,以此为基础建立RFS的预测模型。 方法 回顾性分析昆明医科大学第一附属医院ICU 2020年11月至2022年1月期间收治的202例脓毒症患者的临床资料,根据“ASPEN关于RFS共识建议中”诊断标准,将患者是否发生RFS,分为RFS组(n = 141)和非RFS组(n = 61);比较2组间性别、体重指数(BMI)、营养风险筛查、营养方式、相关危重评分、腹内压(IAP)、相关实验室检查及用药的差异。选取统计学方法中的单因素和多因素Logistic回归分析筛选出ICU脓毒症患者发生RFS的独立危险因素,根据分析结果建立一种预测模型,绘制出受试者工作特征曲线(ROC)评价RFS的预测模型对ICU脓毒症患者发生RFS的预测价值。 结果 202例脓毒症患者相关资料分析,单因素分析结果显示:体重指数(BMI)、白蛋白(ALB)、前白蛋白(PA)、肌酐-身高指数(CHI)、血清钠(Na+)、血清钾(K+)、血清镁(Mg2+)、血清磷(P-)、白介素-6(IL-6)、空腹血糖(FBG)、维生素B1(VitB1)、糖化血红蛋白(HbA1c)、是否使用利尿剂、是否使用胰岛素等指标差异有统计学意义(P < 0.05);多因素分析结果显示:利尿剂的使用、BMI、CHI、血K +、FBG、VitB1是ICU脓毒症患者发生RFS独立危险因素。 结论 以多因素筛选出独立危险因素为基础,建立预测模型表达式为:Logit = 1.39×利尿剂+0.15×BMI-0.14×CHI+0.75×血K+-0.16×FBG+0.78×VitB1-2.94。通过回归分析建立的预测模型一致性强,联合预测有较好的预测价值。 Abstract:Objective To explore the relevant risk factors for Refeeding Syndrome (RFS) in ICU patients with sepsis, and to establish a prediction model of RFS based on the selected risk factors. Methods The clinical data of sepsis patients admitted to the ICU of the First Affiliated Hospital of Kunming Medical University from November 2020 to January 2022 were studied retrospectively. Finally, 202 patients were selected according to the inclusion and exclusion criteria. According to the diagnosis criteria of ASPEN Consensus Recommendations (2020) for RFS, the patients were divided into two groups: RFS group (n = 141) and non-RFS group (n = 61) on the basis of whether occur of RFS. The differences of gender, body mass index (BMI), nutrition risk screening, nutritional way, related critical score, intraabdominal pressure (IAP), relevant laboratory tests, biochemical indexes and pharmacy were compared between the two groups. The independent risk factors of RFS in ICU patients with sepsis were screened by single factor and multivariate logistic regression analysis, and a prediction model was established according to the results of the analysis. The predictive value of the prediction model for RFS in ICU patients with sepsis was evaluated by drawing the receiver operating characteristic curve (ROC) of the subjects. Results After analyzing the relevant data of 202 sepsis patients, the results of monofactor logistic regression analysis showed: Body mass index (BMI), albumin (ALB), prealbumin (PA), creatinine-height index (CHI), serum sodium (Na+), serum potassium (K+), serum magnesium (Mg2+), serum phosphorus (P- ), interleukin-6 (IL-6), fasting blood glucose (FBG), vitamin B1 (VitB1), glycosylated hemoglobin (HbA1c), use of diuretics, use of insulin and other indicators were significantly different (P < 0.05). And multivariate analysis showed that the use of diuretics, BMI, CHI, serum K+, FBG, and VitB1 were independent risk factors for RFS in ICU sepsis patients. Conclusions Based on the independent risk factors in the multivariate screening, the prediction model expression is established as: L = 1.39×diuretics + 0.15×BMI - 0.14×CHI + 0.75×K+-0.16×FBG+0.78×VitB1-2.94. The prediction model established by regression analysis has strong consistency, the joint prediction model has better predictive value. -
Key words:
- Sepsis /
- Refeeding Syndrome /
- Risk factor /
- Prediction model
-
表 1 患者一般情况统计分析[(
$\bar x \pm s $ )/n(%)]Table 1. Statistical analysis of the general data of patients [(
$\bar x \pm s $ )/n(%)]指标 RFS组 非RFS组 χ2/t P 性别 0.049 0.824 男 97(70.29) 41(29.71) 女 44(68.75) 20(31.25) TPN 0.043 0.836 使用 60(70.59) 25(38.46) 未使用 81(69.23) 36(30.77) EN+PN 1.008 0.315 使用 24(77.42) 7(22.58) 未使用 117(68.42) 54(31.58) TEN 1.304 0.254 使用 95(67.38) 46(32.62) 未使用 46(75.41) 15(24.59) BMI(kg/m2) 18.90 ± 3.00 20.23 ± 3.02 −2.714 0.007* NRS2002评分 5.44 ± 1.09 5.21 ± 1.14 0.183 0.227 AGI 2.306 0.129 正常 91(66.42) 46(33.58) 受损 50(76.92) 15(23.08) APACHE-II评分 22.30 ± 2.91 21.93 ± 3.51 0.913 0.362 SOFA评分 12.60 ± 1.82 12.92 ± 2.80 −0.790 0.432 *P < 0.05。 表 2 患者实验室指标统计分析[(
$\bar x \pm s $ )/M(P25,P75)]Table 2. Statistical analysis of laboratory indicators of patients [(
$\bar x \pm s $ )/M(P25,P75)]指标 RFS组 非RFS组 Z/t P WBC(109/L) 12.16 ± 6.18 12.42 ± 5.45 −0.279 0.780 NEUT% 83.63 ± 14.17 85.05 ± 8.68 −0.724 0.470 PCT(ng/L) 3.56(0.78,14.56) 1.90(0.47,11.57) −1.796 0.073 HGB(g/L) 101.77 ± 24.42 107.77 ± 27.00 −1.553 0.122 ALB(g/L) 26.67 ± 5.25 29.18 ± 5.40 −3.093 0.002* PA(mg/L) 87.39 ± 37.48 107.02 ± 50.34 −2.735 0.008* CHI% 44.44 ± 3.64 45.72 ± 3.46 2.330 0.021* 血K+(mmol/L) 3.67 ± 0.55 3.94 ± 0.54 −3.312 0.001* 血Mg2+(mmol/L) 0.60 ± 0.18 0.80 ± 0.12 −8.991 < 0.001* 血P−(mmol/L) 0.57 ± 0.18 0.99 ± 0.31 −9.910 < 0.001* 血Na+(mmol/L) 140.24 ± 6.52 143.13 ± 8.50 −2.636 0.009* 血Ca2+(mmol/L) 2.10 ± 0.17 2.11 ± 0.16 −0.576 0.565 FBG(mmol/L) 11.42 ± 4.42 8.58 ± 3.06 5.254 < 0.001* HbA1c% 6.51 ± 0.96 6.24 ± 0.66 2.322 0.021* FRUC(mmol/L) 283.99 ± 44.15 273.08 ± 43.33 1.622 0.106 VitB1(ng/mL) 2.03(1.18,2.45) 2.40(1.78,2.88) −3.186 0.001* OI 163.00(90.00,237.00) 143.50(78.00,234.75) −1.089 0.276 PaO2(mmHg) 87.00(71.50,118.50) 84.50(68.00,128.00) −0.443 0.658 PaCO2(mmHg) 34.00(30.00,40.00) 36.00(32.00,44.50) −1.454 0.146 *P < 0.05。 表 3 2组患者炎症指标与免疫系统情况比较[(
$\bar x \pm s $ )/M(P25,P75)]Table 3. Comparison of inflammatory indicators and immune system conditions between the two groups[(
$\bar x \pm s $ )/M(P25,P75)]指标 RFS组 非RFS组 Z/t P IL-4(pg/mL) 0.78(0.53,2.04) 0.67(0.46,1.40) −1.357 0.175 IL-6(pg/mL) 47.88(14.72,254.83) 34.02(5.77,98.40) −2.012 0.044* IL-8(pg/mL) 19.34(5.38,55.81) 15.39(4.54,45.53) −0.810 0.418 IL-10(pg/mL) 3.21(1.71,11.66) 3.45(1.73,5.66) −0.834 0.404 CD45+(个/µL) 730.00(532.50,1108.50) 768.00(585.00,1083.00) −0.548 0.584 CD3+/CD45+% 61.46 ± 15.51 60.06 ± 14.03 0.607 0.544 CD3+/CD45+#(个/µL) 529.00(235.50,760.00) 543.00(358.00,771.00) −0.527 0.598 CD3+CD4+/CD45+% 37.29 ± 14.02 35.26 ± 11.94 0.984 0.326 CD3+CD4+/CD45+#(个/µL) 290.00(146.50,432.00) 304.00(165.50,462.50) −0.484 0.629 *P < 0.05。 表 4 2组患者药物使用与其它情况比较[(
$\bar x \pm s $ )/M(P25,P75)/n(%)]Table 4. Comparison of drug use with other conditions of patients between the two groups [(
$\bar x \pm s $ )/M(P25,P75)/n(%)]指标 RFS组 非RFS组 χ2/Z/t P 机械通气时间(h) 246.00(133.00,336.00) 321.50(246.00,372.00) −0.309 0.757 IAP(mmHg) 6.03 ± 1.87 5.97 ± 1.95 0.210 0.834 利尿剂 21.439 < 0.001* 使用 87 ( 84.47) 16 (15.53) 未使用 54 (54.55) 45 (45.45) 胰岛素 20.286 < 0.001* 使用 110 (79.71) 28 (20.29) 未使用 31 (48.44) 33 (51.56) 住院时间(d) 11.00(7.00,15.00) 11.00(7.00,14.00) −0.365 0.715 预后 1.121 0.290 死亡 83 (72.81) 31 (27.19) 好转 58 ( 65.91) 30 (34.09) *P < 0.05。 表 5 ICU脓毒症发生RFS危险因素的单因素分析结果
Table 5. Results of the univariate logistics regression analysis of risk factors for the RFS development in ICU sepsis
指标 OR(95%CI) P BMI 1.14(1.04~1.26) 0.009* ALB 1.09(1.03~1.16) 0.003* PA 1.01(1.01~1.02) 0.004* CHI 0.90(0.83~0.99) 0.022* 血K+ 2.42(1.39~4.24) 0.002* 血Mg2+ 33.64(40.03~58.15) < 0.001* 血P− 81.58(12.76~160.66) < 0.001* 血Na+ 1.06(1.01~1.11) 0.014* FBG 0.82(0.75~0.90) < 0.001* HbA1c 0.62(0.40~0.98) 0.040* VitB1 1.78(1.24~2.54) 0.002* IL-6 0.99(0.99~1.01) 0.106 利尿剂 2.97(1.84~4.78) < 0.001* 胰岛素 4.18(2.20~7.95) < 0.001* *P < 0.05。 表 6 ICU脓毒症患者发生RFS危险因素的多因素Logistic回归分析
Table 6. Multivariate logistic regression analysis of the risk factors for developing RFS in ICU sepsis patients
变量 β S.E Wald OR 95%CI P 利尿剂 1.39 0.40 12.35 4.01 1.85~8.70 < 0.001* BMI 0.15 0.06 6.26 1.16 1.03~1.31 0.012* CHI −0.14 0.05 6.33 0.87 0.79~0.97 0.012* 血K+ 0.75 0.34 5.00 2.12 1.10~4.11 0.025* FBG −0.16 0.05 8.59 0.86 0.77~0.95 0.003* VitB1 0.78 0.25 9.83 2.17 1.34~3.52 0.002* 常量 −2.94 3.08 .091 − − 0.039* *P < 0.05。 表 7 预测模型中各个变量赋值表
Table 7. Each variable assignment table in the prediction model
变量 各个变量赋值 利尿剂 是 = 1,否 = 0 BMI 连续变量 CHI 连续变量 血K+ 连续变量 FBG 连续变量 VitB1 连续变量 表 8 联合预测指标和各个变量对ICU脓毒症患者发生RFS的预测价值
Table 8. Predictive value of the combined predictors and various variables for the occurrence of RFS in patients with ICU sepsis
指标 AUC(95%CI) cut-off P 联合预测因子 0.83(0.77-0.88) −1.01 < 0.001* BMI 0.63(0.54-0.71) 19.38 0.004* CHI 0.60(0.51-0.68) 44.50 0.043* 血K+ 0.65(0.58-0.73) 3.31 0.001* FBG 0.69(0.62-0.77) 7.57 < 0.001* VitB1 0.64(0.55-0.73) 1.94 0.001* *P < 0.05。 -
[1] Reinhart K,Daniels R,Kissoon N,et al. Recognizing sepsis as a global health priority - WHO resolution[J]. N Engl J Med,2017,377(5):414-417. doi: 10.1056/NEJMp1707170 [2] Preiser J C,van Zanten A R,Berger M M,et al. Metabolic and nutritional support of critically ill patients:Consensus and controversies[J]. Crit Care,2015,19(1):35-46. doi: 10.1186/s13054-015-0737-8 [3] Wischmeyer P E. Nutrition therapy in sepsis[J]. Crit Care Clin,2018,4(1):107-125. [4] McKnight C L,Newberry C,Sarav M,et al. Refeeding syndrome in the critically ill:A literature review and clinician’s guide[J]. Curr Gastroenterol Rep,2019,21(11):1-7. [5] Brozek J,Chapman C B,Keys A. Drastic food restriction:effect on cardiovascular dynamics dynamics in normotensive and hypertensive conditions[J]. J Am Med Assoc,1948,137(18):1569. doi: 10.1001/jama.1948.02890520001001 [6] Da Silva J S V,Seres D,Sabino K et al. ASPEN Consensus recommendations for refeeing syndrome[J]. Nutr Clin Pract,2020,35(2):178-195. doi: 10.1002/ncp.10474 [7] National Collaborating Centre for Acute Care ( UK). Nutrition support for adults:oral nutrition support,enteral tube feeding and parenteral nutrition[J]. London:National Collaborating Centre for Acute Care (UK),2006,63(3):342-350. [8] Wong,Gabriel J Y,Pang,et al. Refeeding hypophosphatemia in patients receiving parenteral nutrition:Prevalence,risk factors,and predicting its occurrence[J]. Nutr Clin Pract,2021,36(3):679-688. doi: 10.1002/ncp.10559 [9] Luke R G,Galla J H. It is chloride depletion alkalosis,not contraction alkalosis[J]. J Am Soc Nephrol,2012,23:204-207. doi: 10.1681/ASN.2011070720 [10] 于恺英,刘俐惠,石汉平. 营养状况是基本生命体征[J]. 肿瘤代谢与营养电子杂志,2019,6(4):391-396. doi: 10.16689/j.cnki.cn11-9349/r.2019.04.001 [11] 沈丽达,龙庭凤,赵艳芳,等. 胃癌患者营养风险筛查和营养支持治疗调查分析[J]. 昆明医科大学学报,2014,35(10):86-90. doi: 10.3969/j.issn.1003-4706.2014.10.024 [12] Datta,Debapriya,Foley,et al. Can creatinine height index predict weaning and survival outcomes in patients on prolonged mechanical ventilation after critical illness?[J]. J Intensive Care Med,2018,33(2):104-110. doi: 10.1177/0885066616648133 [13] Blaser A R, van Zanten R H. Electrolyte disorders during the initiation of nutrition therapy in the ICU[J]. Curr Opin Clin Nutr Metab Care, 202), 24(2): 151-158. [14] Tongyoo S,Viarasilpa T,Permpikul C. Serum potassium levels and outcomes in critically ill patients in the medical intensive care unit[J]. J Int Med Res,2018,46:1254-1262. doi: 10.1177/0300060517744427 [15] Friedli N,Baumann J,Hummel R,et al. Refeeding syndrome is associated with increased mortality in malnourished medical inpa- tients:secondary analysis of a randomized trial[J]. Medicine (Baltimore),2020,99(1):e18506. [16] Deutsche,Gesellschaftfür,ErnährungÖGfE,et al. Gesellschaft für Ernährungsforschung (2015) Referenzwerte für die Nährstoffffzufuhr[J]. Umschau Buchverlag,Neustadtan derWeinstraße,2015,64(12):975-976. [17] Collie J T B,Greaves R F,Jones O A H,et al. Vitamin B1 in critically ill patients:needs and challenges[J]. Clin Chem Lab Med,2017,55(11):1652-1668. [18] Zhang Q,Zhao G,Yang N L,et al. Fasting blood glucose levels in patients with different types of diseases[J]. Prog Mol Biol Transl Sci,2019,162:277-292. [19] See K C. Glycemic targets in critically ill adults:A mini-review[J]. World J Diabetes,2021,12(10):1719-1730. doi: 10.4239/wjd.v12.i10.1719 -





 下载:
下载: