Association between LOXL2 and Snail Expression Levels and Overall Survival Rate after Surgery in Patients with Cholangiocarcinoma
-
摘要:
目的 探讨赖氨酰氧化酶样蛋白2(LOXL2)及Snail在胆管癌(CCA)组织中的表达及其与患者临床病理特征和术后生存预后的关系。 方法 收集云南省第一人民医院2014年1月至2021年4月期间行手术切除的31例胆管癌病例及随访资料,应用免疫组织化学染色检测患者癌组织及癌旁正常组织标本中LOXL2及Snail的表达情况,分析2种蛋白表达与临床病理资料及预后的关系。 结果 肿瘤组织中LOXL2及Snail蛋白表达量均明显高于癌旁组织,且LOXL2表达与Snail表达存在着一定的正相关关系(r = 0.430,P = 0.016),Snail表达与淋巴结转移(P = 0.025)有关,与LOXL2及Snail高表达患者比较,LOXL2及Snail低表达患者术后总生存率较高(P < 0.05),单因素生存分析显示:Snail高表达、存在淋巴结转移与预后更差的胆管癌患者相关(P < 0.05)。Cox多因素生存分析结果表明:淋巴结转移可能是影响胆管癌患者预后的独立因素(P = 0.017)。 结论 LOXL2、Snail在胆管癌组织中表达增加,LOXL2与Snail 2种蛋白的表达密切相关,Snail的过表达可能更易出现淋巴结的转移,促进肿瘤细胞的侵袭性行为,并且淋巴结转移可能是影响胆管癌患者预后的独立因素。LOXL2及Snail过表达的患者其术后生存率相对较低。因此临床联合检测LOXL2及Snail对胆管细胞癌患者的预后判断具有重要意义。 Abstract:Objective To investigate the expression of lysoxygenase-like protein 2 (LOXL2) and Snail in the tissues of cholangiocarcinoma (CCA) and their association with clinicopathological features and postoperative survival. Methods 31 patients with cholangiocarcinoma who underwent surgical removal in the First People’s Hospital of Yunnan Province from 2014 to 2021 and their follow-up data were collected. The expression of LOXL2 and Snail in cancer tissues and adjacent normal tissues of patients was detected by immunohistochemical staining, and the association between the expression of the two proteins and clinicopathological data and prognosis was analyzed. Results The expression levels of LOXL2 and Snail in tumor tissues were significantly higher than those in adjacent tissues, and there was a positive correlation between LOXL2 expression and Snail expression (r = 0.430, P = 0.016). Snail expression was associated with lymph node metastasis (P = 0.025). Compared with patients with high expression of LOXL2 and Snail, patients with low expression of LOXL2 and Snail had higher overall survival rate (all P < 0.05). Univariate survival analysis showed that high expression of Snail and lymph node metastasis were associated with worse prognosis in patients with cholangiocarcinoma (all P < 0.05). Multivariate Cox survival analysis showed that lymph node metastasis might be an independent prognostic factor for patients with cholangiocarcinoma (P = 0.017). Conclusion The expression of LOXL2 and Snail is increased in cholangiocarcinoma tissues, and the expression of LOXL2 and Snail is closely related. The overexpression of Snail may be more prone to lymph node metastasis and promote the invasive behavior of tumor cells, and lymph node metastasis may be an independent factor affecting the prognosis of cholangiocarcinoma patients. Patients with LOXL2 and Snail overexpression have a relatively low postoperative survival rate.Therefore, the combined detection of LOXL2 and Snail is of great significance for the prognosis of patients with cholangiocarcinoma. -
Key words:
- Cholangiocarcinoma /
- LOXL2 /
- Snail /
- Invasive metastasis /
- Epithelial mesenchymal transition /
- Prognosis
-
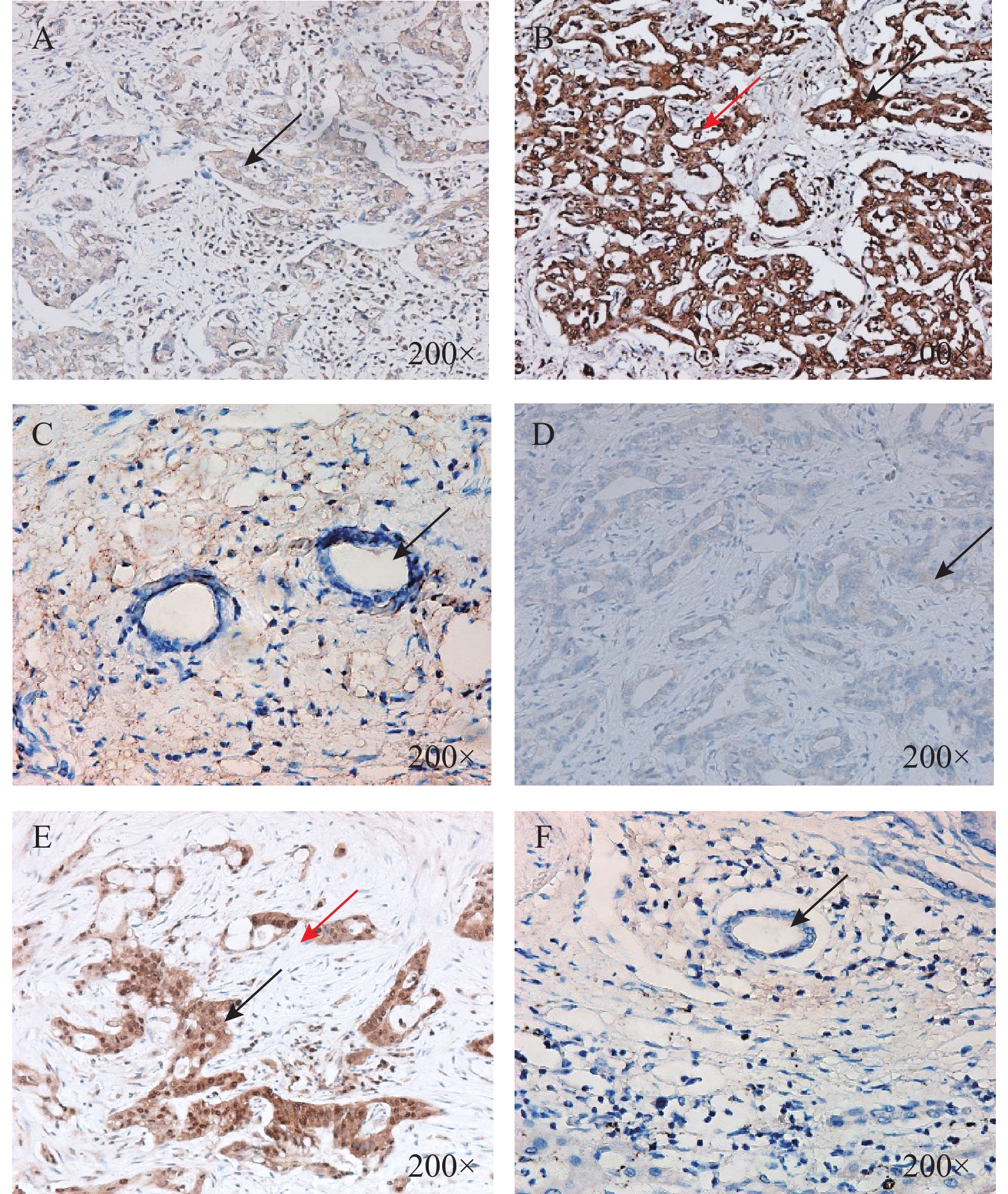
图 1 胆管癌病理组织和癌旁正常胆管组织LOXL2和Snail表达(×200)
A:胆管癌组织中LOXL2低表达(箭头所示部位胞质);B:胆管癌组织中LOXL2高表达(黑色箭头所示部位胞质,红色箭头所示部位核周);C:癌旁正常胆管组织中LOXL2无表达(箭头所示癌旁正常胆管细胞)D:胆管癌组织中Snail低表达(箭头所示部位胞质);E:胆管癌组织中Snail高表达(黑色箭头所示部位胞质,红色箭头所示部位胞核);F:癌旁正常胆管组织中Snail无表达(箭头所示癌旁正常胆管细胞)。
Figure 1. Expression of LOXL2 and Snail in pathological tissues and adjacent normal bile duct tissues of cholangiocarcinoma(×200)
表 1 胆管癌病理组织中LOXL2和Snail表达相关性(n)
Table 1. Correlation between LOXL2 and Snail expression in pathological tissues of cholangiocarcinoma (n)
表达情况 LOXL2 r P 高表达(n = 16) 低表达(n = 15) Snail 高表达(n = 13) 10 3 0.430 0.016* 低表达(n = 18) 6 12 *P < 0.05。 表 2 胆管癌病理组织中LOXL2和Snail表达与临床病理参数相关性[n(%)]
Table 2. Correlation between LOXL2 and Snail expression and clinicopathological parameters in pathological tissues of cholangiocarcinoma [n(%)]
临床病理参数 n Snail表达 P LOXL2表达 P 高表达 低表达 高表达 低表达 性别 男 16 6(37.5) 10(62.5) 0.722 9(56.3) 7(43.7) 0.724 女 15 7(46.7) 8(53.3) 7(46.7) 8(53.3) 年龄(岁) ≥60 16 8(50.0) 8(50.0) 0.473 11(68.7) 5(31.3) 0.076 < 60 15 5(33.3) 10(66.7) 5(33.3) 10(66.7) 肿瘤大小(cm) ≥5.7 17 6(35.3) 11(64.7) 0.481 7(41.2) 10(58.8) 0.285 < 5.7 14 7(50.0) 7(50.0) 9(64.3) 5(35.7) 肿瘤位置 肝内 26 10(38.5) 16(61.5) 0.625 13(50.0) 13(50.0) 1.000 肝外 5 3(60.0) 2(40.0) 3(60.0) 2(40.0) 肿瘤分化程度 高中 14 5(35.7) 9(64.3) 0.717 8(57.1) 6(42.9) 0.722 中低 17 8(47.1) 9(52.9) 8(47.1) 9(52.9) 淋巴结转移 有 15 10(66.7) 5(33.3) 0.025* 10(66.7) 5(33.3) 0.156 无 16 3(18.7) 13(81.3) 6(37.5) 10(62.5) *P < 0.05。 表 3 胆管癌患者总生存率预后因素的单因素和多因素分析
Table 3. Univariate and multivariate analysis of prognostic factors for overall survival of patients with cholangiocarcinoma
因数单因素分析 多因素分析 HR(95% CI) P HR(95% CI) P 性别 1.042(0.467~2.323) 0.920 - - 年龄 1.354(0.605~3.301) 0.461 - - 肿瘤大小 0.882(0.391~1.993) 0.764 - - 肿瘤位置 0.665(0.226~1.960) 0.460 - - 分化程度 0.724(0.319~1.643) 0.440 - - 淋巴转移 0.267(0.115~0.621) 0.002** 0.244(0.077~0.776) 0.017* Snail表达 0.437(0.194~0.983) 0.045* 1.135(0.377~3.420) 0.822 LOXL2表达 0.445(0.192~1.030) 0.059 - - *P < 0.05。 -
[1] Banales J M,Cardinale V,Carpino G,et al. Expert consensus document:Cholangiocarcinoma:Current knowledge and future perspectives consensus statement from the european network for the study of cholangiocarcinoma (ENS-CCA)[J]. Nat Rev Gastroenterol Hepatol,2016,13(5):261-280. [2] Rizvi S,Khan S A,Hallemeier C L,et al. Cholangiocarcinoma - evolving concepts and therapeutic strategies[J]. Nat Rev Clin Oncol,2018,15(2):95-111. [3] Bertuccio P,Malvezzi M,Carioli G,et al. Global trends in mortality from intrahepatic and extrahepatic cholangiocarcinoma[J]. J Hepatol,2019,71(1):104-114. doi: 10.1016/j.jhep.2019.03.013 [4] Banales J M,Marin J J G,Lamarca A,et al. Cholangiocarcinoma 2020:The next horizon in mechanisms and management[J]. Nat Rev Gastroenterol Hepatol,2020,17(9):557-588. doi: 10.1038/s41575-020-0310-z [5] Groot Koerkamp B,Wiggers J K,Allen P J,et al. Recurrence rate and pattern of perihilar cholangiocarcinoma after curative intent resection[J]. J Am Coll Surg,2015,221(6):1041-1049. doi: 10.1016/j.jamcollsurg.2015.09.005 [6] Lindnér P,Rizell M,Hafström L. The impact of changed strategies for patients with cholangiocarcinoma in this millenium[J]. HPB Surg,2015(12):1-6. [7] Spolverato G,Kim Y,Alexandrescu S,et al. Management and outcomes of patients with recurrent intrahepatic cholangiocarcinoma following previous curative-intent surgical resection[J]. Ann Surg Oncol,2016,23(1):235-243. [8] Strijker M,Belkouz A,Van Der Geest L G,et al. Treatment and survival of resected and unresected distal cholangiocarcinoma:A nationwide study[J]. Acta Oncol,2019,58(7):1048-1055. [9] Cambridge W A,Fairfield C,Powell J J,et al. Meta-analysis and meta-regression of survival after liver transplantation for unresectable perihilar cholangiocarcinoma[J]. Ann Surg,2021,273(2):240-250. doi: 10.1097/SLA.0000000000003801 [10] Thiery J P,Acloque H,Huang R Y,et al. Epithelial-mesenchymal transitions in development and disease[J]. Cell,2009,139(5):871-890. doi: 10.1016/j.cell.2009.11.007 [11] Nieto M A. The snail superfamily of zinc-finger transcription factors[J]. Nat Rev Mol Cell Biol,2002,3(3):155-166. [12] Ke A W,Shi G M,Zhou J,et al. Role of overexpression of CD151 and/or c-Met in predicting prognosis of hepatocellular carcinoma[J]. Hepatology,2009,49(2):491-503. [13] Huang X Y,Zhang C,Cai J B,et al. Comprehensive multiple molecular profile of epithelial mesenchymal transition in intrahepatic cholangiocarcinoma patients[J]. PLoS One,2014,9(5):e96860. doi: 10.1371/journal.pone.0096860 [14] 康强,邹浩,刘立鑫,等. Snail在肝内胆管癌中的表达及其临床意义[J]. 中国普通外科杂志,2017,26(2):199-204. [15] Akiri G,Sabo E,Dafni H,et al. Lysyl oxidase-related protein-1 promotes tumor fibrosis and tumor progression in vivo[J]. Cancer Res,2003,63(7):1657-1666. [16] Peinado H,Moreno-Bueno G,Hardisson D,et al. Lysyl oxidase-like 2 as a new poor prognosis marker of squamous cell carcinomas[J]. Cancer Res,2008,68(12):4541-4550. doi: 10.1158/0008-5472.CAN-07-6345 [17] Ahn S G,Dong S M,Oshima A,et al. LOXL2 expression is associated with invasiveness and negatively influences survival in breast cancer patients[J]. Breast Cancer Res Treat,2013,141(1):89-99. [18] Zhan P,Lv X J,Ji Y N,et al. Increased lysyl oxidase-like 2 associates with a poor prognosis in non-small cell lung cancer[J]. Clin Respir J,2018,12(2):712-720. [19] Torres S,Garcia-Palmero I,Herrera M,et al. LOXL2 is highly expressed in cancer-associated fibroblasts and associates to poor colon cancer survival[J]. Clin Cancer Res,2015,21(21):4892-4902. doi: 10.1158/1078-0432.CCR-14-3096 [20] Peng L,Ran Y L,Hu H,et al. Secreted LOXL2 is a novel therapeutic target that promotes gastric cancer metastasis via the Src/FAK pathway[J]. Carcinogenesis,2009,30(10):1660-1669. doi: 10.1093/carcin/bgp178 [21] Tian J,Sun H X,Li Y C,et al. LOXL 2 promotes the epithelial-mesenchymal transition and malignant progression of cervical cancer[J]. Onco Targets Ther,2019,12:8947-8954. [22] Choi J,Chung T,Rhee H,et al. Increased expression of the matrix-modifying enzyme Lysyl oxidase-like 2 in aggressive hepatocellular carcinoma with poor prognosis[J]. Gut Liver,2019,13(1):83-92. doi: 10.5009/gnl17569 [23] Li T Y,Xu L Y,Wu Z Y,et al. Reduced nuclear and ectopic cytoplasmic expression of lysyl oxidase-like 2 is associated with lymph node metastasis and poor prognosis in esophageal squamous cell carcinoma[J]. Hum Pathol,2012,43(7):1068-1076. doi: 10.1016/j.humpath.2011.07.027 [24] Canesin G,Cuevas E P,Santos V,et al. Lysyl oxidase-like 2 (LOXL2) and E47 EMT factor:Novel partners in E-cadherin repression and early metastasis colonization[J]. Oncogene,2015,34(8):951-964. doi: 10.1038/onc.2014.23 [25] Hong X,Yu J J. Silencing of lysyl oxidase-like 2 inhibits the migration,invasion and epithelial-to-mesenchymal transition of renal cell carcinoma cells through the Src/FAK signaling pathway[J]. Int J Oncol,2019,54(5):1676-1690. [26] Wen B,Xu L Y,Li E M. LOXL2 in cancer:Regulation,downstream effectors and novel roles[J]. Biochim Biophys Acta Rev Cancer,2020,1874(2):188435. [27] 高应鸿,李天宇,高占峰,等. 胆管癌组织中赖氨酰氧化酶样蛋白-2的表达及其与EMT的关系[J]. 中华普通外科杂志,2008,10(23):784-787. [28] Bergeat D,Fautrel A,Turlin B,et al. Impact of stroma LOXL2 overexpression on the prognosis of intrahepatic cholangiocarcinoma[J]. J Surg Res,2016,203(2):441-450. doi: 10.1016/j.jss.2016.03.044 [29] Boulay J L,Dennefeld C,Alberga A. The Drosophila developmental gene snail encodes a protein with nucleic acid binding fingers[J]. Nature,1987,330(6146):395-398. [30] Alberga A,Boulay J L,Kempe E,et al. The snail gene required for mesoderm formation in Drosophila is expressed dynamically in derivatives of all three germ layers[J]. Development,1991,111(4):983-992. doi: 10.1242/dev.111.4.983 [31] Peinado H,Ballestar E,Esteller M,et al. Snail mediates E-cadherin repression by the recruitment of the Sin3A/histone deacetylase 1 (HDAC1)/HDAC2 complex[J]. Mol Cell Biol,2004,24(1):306-319. doi: 10.1128/MCB.24.1.306-319.2004 [32] Peinado H,Del Carmen Iglesias-De La Cruz M,Olmeda D,et al. A molecular role for lysyl oxidase-like 2 enzyme in snail regulation and tumor progression[J]. Embo J,2005,24(19):3446-3458. doi: 10.1038/sj.emboj.7600781 [33] Peinado H,Portillo F,Cano A. Switching on-off Snail:LOXL2 versus GSK3beta[J]. Cell Cycle,2005,4(12):1749-1752. doi: 10.4161/cc.4.12.2224 [34] Cuevas E P,Eraso P,Mazón M J,et al. LOXL2 drives epithelial-mesenchymal transition via activation of IRE1-XBP1 signalling pathway[J]. Sci Rep,2017,7(1):44988. doi: 10.1038/srep44988 [35] Fan Z,Zheng W,Li H,et al. LOXL2 upregulates hypoxia-inducible factor-1α signaling through Snail-FBP1 axis in hepatocellular carcinoma cells[J]. Oncol Rep,2020,43(5):1641-1649. -






 下载:
下载: