Effect of Abdominal Regional Block Combined with Intravenous Analgesia on Postoperative Complications In Elderly Patients
-
摘要:
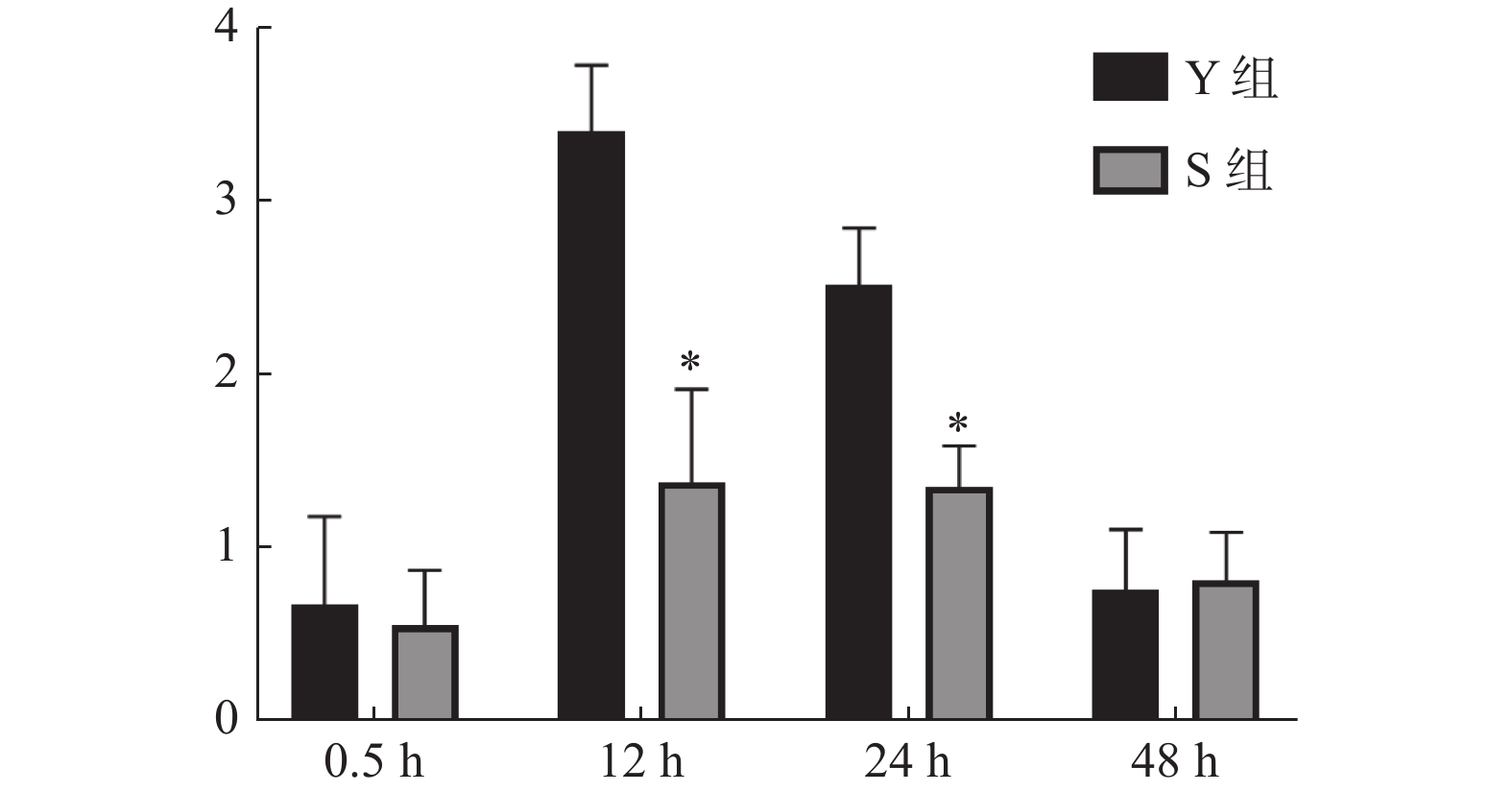
目的 探讨腹部区域阻滞联合患者自控静脉镇痛(PCIA)对比患者自控硬膜外镇痛(PCEA)对腹腔镜腹股沟疝修补术老年患者术后镇痛效果、焦虑情绪、恶心呕吐及炎性介质释放的影响。 方法 选取昆明市第二人民医院普外科所收治的全身麻醉气管插管下腹腔镜腹股沟疝修补术老年患者90例,时间自2021年2月至2022年6月,采用随机数字表法分为神经阻滞组(S组)和硬膜外镇痛组(Y组)。每组各45例,Y组患者择T12~L1行硬膜外穿刺置管,连接PCEA测定硬膜外阻滞平面在T8~L1以上后行快速诱导全麻气管插管下完成手术,术毕继续使用PCEA行术后镇痛;S组患者在超声引导下行术侧髂腹下/髂腹股沟神经阻滞(IINB)及双侧腹直肌鞘阻滞(RSB),测定区域阻滞平面在术侧及腹正中T8~L1以上后行快速诱导全麻气管插管下完成手术,术毕联合PCIA行术后镇痛。对比2组患者术毕清醒及术后不同时间点疼痛强度数字等级评定量表(NRS)评分、贝克焦虑量表(BAI)评分、血清高迁移率族蛋白B1(HMGB1)浓度及术后恶心呕吐(PONV)发生率。 结果 2组患者性别、年龄、美国麻醉医师协会风险评估分级(ASA)、身体质量指数值(BMI)、手术用时比较,差异均无统计学意义(P > 0.05);S组住院天数少于Y组,差异有统计学意义(P < 0.05)。2组组间及时间存在交互作用(P < 0.05);2组术毕拔除气管导管后0.5 h的NRS评分组间比较,差异无统计学意义(P > 0.05);S组术后12 h,24 h时间点NRS评分均低于Y组(P < 0.05);2组术后48 h时间点NRS评分组间比较,差异无统计学意义(P > 0.05)。2组组间及时间存在交互作用(P < 0.05);S组术后12 h,24 h时间点BAI评分均低于Y组(P < 0.05);2组术后48 h时间点BAI评分组间比较,差异无统计学意义(P > 0.05);2组术后12 h,24 h,48 h任意时间点BAI评分组内比较,差异均有统计学意义(P < 0.05),且BAI评分逐渐降低。2组术前12 h时间点HMGB1组间比较,差异无统计学意义(P > 0.05);S组术后12 h,24 h时间点HMGB1均低于Y组(P < 0.05);2组术后48 h时间点HMGB1组间比较,差异无统计学意义(P > 0.05);2组术后12 h,24 h,48 h时间点HMGB1组内比较均高于术前12 h时间点(P < 0.05)。S组术后12 h,24 h,48 h时间点PONV发生率均低于Y组(P < 0.05);2组术后12 h,24 h,48 h时间点PONV发生率组内比较,差异均有统计学意义(P < 0.05)。 结论 术前采用腹部区域阻滞联合PCIA多模式镇痛相较于硬膜外阻滞镇痛,对减轻全身麻醉下腹腔镜腹股沟疝修补术老年患者术后疼痛和焦虑情绪、减少术后恶心呕吐发生率以及降低静脉血中HMGB1浓度有更积极的作用,且对减少术后恶心呕吐发生率的效应更为持久,有利于老年患者术后恢复。 Abstract:Objective To investigate the influences of abdominal regional block combined with patient-controlled intravenous analgesia (PCIA) and patient-controlled epidural analgesia (PCEA) on postoperative analgesia, anxiety, nausea, vomiting and inflammatory mediator release in elderly patients underwent laparoscopic inguinal hernia repair. Methods 90 elderly patients with laparoscopic inguinal hernia repair under general anesthesia and endotracheal intubation treated in Kunming Second People’s Hospital from February 2021 to June 2022 were randomly divided into nerve block group (S group) and epidural analgesia group (Y group), with 45 cases in each group. Patients in group Y received epidural puncture and intubation at T12~L1 level, and PCEA was connected to determine the epidural block level. After the epidural block level was above T8~L1, the operation was completed under rapid induction of general anesthesia and endotracheal intubation. PCEA was used for postoperative analgesia after operation. In group S, the patients underwent ultrasound-guided lateral ilioabdominal/ilioinguinal nerve block (IINB) and bilateral rectus abdominis sheath block (RSB). The regional block level was measured and confirmed above T8~L1 at the operation side and abdominal medline. And the operation was completed under rapid induction of general anesthesia and endotracheal intubation. Postoperative analgesia was performed in combination with PCIA. The scores of NRS, BAI, HMGB1 and PONV were compared between the two groups. Results There was no significant difference in gender, age, ASA, BMI and operating time in the two groups (P > 0.05). The length of stay in group S was less than that in group Y (P < 0.05). There was no significant difference in NRS between the two groups at 0.5h after tracheal tube removal (P > 0.05). The NRS of group S at 12 h and 24 h after operation were lower than those of group Y (P < 0.05). There was no significant difference in NRS between the two groups at 48 h after operation (P > 0.05). There was interaction between the two groups (P < 0.05). The BAI of group S at 12 h and 24 h after operation were lower than those of group Y (P < 0.05). There was no significant difference in BAI between the two groups at 48 h after operation (P > 0.05). At any time point of 12 h, 24 h and 48 h after operation, there were significant differences in BAI between the two groups (P < 0.05), and the BAI decreased gradually. There was no significant difference in HMGB1 between the two groups at 12 h before operation (P > 0.05). HMGB1 in group S was lower than that in group Y at 12 h and 24 h after operation (P < 0.05). There was no significant difference in HMGB1 between the two groups at 48 h after operation (P > 0.05). HMGB1 at 12 h, 24 h and 48 h after operation in both groups was higher than that at 12 h before operation (P < 0.05). The incidence of PONV at 12 h, 24 h and 48 h after operation in group S was lower than that in group Y (P < 0.05). The incidence of PONV at 12 h, 24 h and 48 h after operation in the two groups had significant difference (P < 0.05). Conclusion Compared with epidural block analgesia, preoperative abdominal block combined with PCIA multimodal analgesia has a more positive effect on reducing the postoperative pain and anxiety of elderly patients underwent laparoscopic inguinal hernia repair under general anesthesia, reducing the incidence of postoperative nausea and vomiting, and reducing the concentration of HMGB1 in venous blood, and has a more lasting effect on reducing the incidence of postoperative nausea and vomiting, which is conducive to the postoperative recovery of elderly patients. -
表 1 一般情况($\bar x \pm s $)
Table 1. General information ($\bar x \pm s $)
因素 Y组(n = 45) S组(n = 45) χ2/t P 性别(男/女) 44/1 43/2 0.345 0.587 年龄(岁) 67.52 ± 6.84 67.63 ± 7.43 0.073 0.941 ASA (II/III) 35/10 37/8 0.278 0.598 BMI (kg/m2) 22.6 ± 1.47 22.3 ± 1.55 0.942 0.348 手术用时(min) 71.31 ± 20.17 70.24 ± 19.65 0.254 0.799 住院天数(d) 15.38 ± 2.69 13.76 ± 2.27 3.087 0.003* *P < 0.05。 表 2 术后NRS评分[($\bar x \pm s $),分]
Table 2. Postoperative NRS scores [($\bar x \pm s $),scores]
组别 0.5 h 12 h 24 h 48 h Y组(n = 45) 0.67 ± 0.51 3.41 ± 0.38 2.52 ± 0.33 0.76 ± 0.35 S组(n = 45) 0.55 ± 0.32 1.38 ± 0.54 1.35 ± 0.24* 0.81 ± 0.28 F组间/P组间 360.900/ < 0.001* F时间/P时间 101.100/ < 0.001* F组间*时间/P组间*时间 194.800/ < 0.001* *P < 0.05。 表 3 术后BAI评分[($\bar x \pm s $),分]
Table 3. Postoperative BAI scores [($\bar x \pm s $),scores]
组别 12 h 24 h 48 h Y组(n=45) 12.41 ± 2.47 9.28 ± 2.41 5.11 ± 1.13 S组(n=45) 6.64 ± 1.53 5.15 ± 1.18 4.92 ± 1.25 F组间/P组间 18.340/ < 0.001* F时间/P时间 63.610/ < 0.001* F组间*时间/P组间*时间 97.650/ < 0.001* *P < 0.05。 表 4 术后HMGB1[($\bar x \pm s $),pg/mL]
Table 4. HMGB1 after operation [($\bar x \pm s $),pg/mL]
组别 术前12 h 术后12 h 术后24 h 术后48 h Y组(n = 45) 73.67 ± 12.81 286.31 ± 32.52△ 169.52 ± 30.27△ 95.76 ± 0.35△ S组(n = 45) 73.25 ± 13.32 136.24 ± 21.93*△ 102.17 ± 21.68*△ 94.81 ± 18.29△ F组间/P组间 736.300/ < 0.001 F时间/P时间 598.800/ < 0.001 F组间*时间/P组间*时间 251.700/ < 0.001 与Y组比较,*P < 0.05;与术前12h比较,△P < 0.05。 表 5 术后PONV [n(%)]
Table 5. Postoperative PONV [n(%)]
组别 12 h 24 h 48 h χ2 P Y组(n = 45) 19(42.22) 11(24.44) 6(13.33) 9.733 0.007 S组(n = 45) 10(22.22) 4(8.89) 1(2.22) 9.450 0.009* χ2 4.121 3.920 3.873 P 0.042* 0.047* 0.049* *P < 0.05。 -
[1] 庞国防, 胡才友, 杨泽. 中国人口老龄化趋势与对策[J]. 中国老年保健医学,2021,19(1):3-5. [2] 中华医学会麻醉学分会老年人麻醉与围术期管理学组, 中华医学会麻醉学分会疼痛学组国家老年疾病临床医学研究中心, 国家老年麻醉联盟. 老年患者围手术期多模式镇痛低阿片方案中国专家共识(2021版)[J]. 中华医学杂志,2021,101(3):170-184. doi: 10.3760/cma.j.cn112137-20200520-01600 [3] 郭雁飞, 施燕, 阮晔, 等. 全球老龄化与成人健康研究中国项目进展[J]. 中华流行病学杂志,2019,40(10):1203-1205. doi: 10.3760/cma.j.issn.0254-6450.2019.10.006 [4] Gambassi G, Catananti C. Pain assessment in the elderly[J]. Surgical oncology,2010,19(3):140-148. doi: 10.1016/j.suronc.2009.11.010 [5] 董文芳, 陆建华. 术后急性疼痛与慢性疼痛关系的研究进展[J]. 国际麻醉学与复苏杂志,2015,36(1):78-81. doi: 10.3760/cma.j.issn.1673-4378.2015.01.019 [6] 中华医学会麻醉学分会. 成人手术后疼痛处理专家共识[J]. 临床麻醉学杂志,2017,33(9):911-917. [7] Zhou B, Ji H, Liu Y, et al. ERAS reduces postoperative hospital stay and complications after bariatric surgery: A retrospective cohort study[J]. Medicine,2021,100(47):e2783. [8] 李响. 美国麻醉医师协会分级在老年肝癌患者外科治疗风险评估中的作用[J]. 实用老年医学,2015,29(9):755-758. [9] 刘晓灵, 高世定. 不同NYHA分级慢性心力衰竭患者心肌纤维化指标水平与心电图变化的临床意义[J]. 武警医学,2018,29(11):1028-1031,1035. doi: 10.3969/j.issn.1004-3594.2018.11.004 [10] 劳贤邦, 庞德春, 纪建波, 等. 两种苏醒评分方法对麻醉复苏效果影响的比较[J]. 护士进修杂志,2016,31(11):1043-1045. [11] 曹琳. 双抗原夹心ELISA法检测抗-HCV的临床价值研究[J]. 当代医学,2021,27(4):166-167. doi: 10.3969/j.issn.1009-4393.2021.04.072 [12] 兰岭, 申乐, 黄宇光. 术后慢性疼痛相关炎症反应及炎症细胞因子研究进展[J]. 中国医学科学院学报,2015,37(6):741-745. [13] 宋学军, 樊碧发, 万有, 等. 国际疼痛学会新版疼痛定义修订简析[J]. 中国疼痛医学杂志,2020,26(9):641-644. doi: 10.3969/j.issn.1006-9852.2020.09.001 [14] 中华医学会老年医学分会. 老年患者术后谵妄防治中国专家共识[J]. 中华老年医学杂志,2016,35(12):1257-1262. doi: 10.3760/cma.j.issn.0254-9026.2016.12.001 [15] 郝楠楠. 超声引导下腹横肌筋膜阻滞麻醉对老年腹腔镜手术患者疼痛应激及胃肠功能的影响[J]. 中国实用医药,2021,16(5):31-33. [16] Evered L, Silbert B, Knopman D, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018[J]. Anesthesiology,2018,129(5):872-879. doi: 10.1097/ALN.0000000000002334 [17] 唐丹. 简版老年抑郁量表(GDS-15)在中国老年人中的使用[J]. 中国临床心理学杂志,2013,21(3):402-405. [18] 叶瑞繁, 耿庆山, 陈剑, 等. 医院焦虑抑郁量表与Beck抑郁问卷在综合医院门诊病人中评定抑郁的比较[J]. 中国临床心理学杂志,2013,21(1):48-50,173. [19] Ying L, Lei W, Jianbo Z. Factor structure and psychometric properties of Chinese version of Beck Anxiety Inventory in Chinese doctors[J]. Journal of Health Psychology,2018,23(5):657-666. doi: 10.1177/1359105316658971 [20] 于洋, 孙建良. 术后恶心呕吐(PONV)的机制及其防治研究进展[J]. 麻醉安全与质控,2018,13(2):113-118. [21] 蔡少英, 叶丽玲, 张平恒, 等. 不同麻醉方法对老年胃肠手术患者术后认知功能和外周血高迁移率族蛋白B1的影响[J]. 实用临床医药杂志,2021,25(4):41-44. doi: 10.7619/jcmp.20201189 [22] 李欣. 麻醉深度对中老年患者术后认知功能及外周血高迁移率族蛋白B1的影响[J]. 中国保健营养,2019,29(5):356. doi: 10.3969/j.issn.1004-7484.2019.05.465 [23] 赵敏, 陆江阳, 吕艺. 高迁移率族蛋白B1的生物学效应及在几种疾病发病中的作用[J]. 军事医学科学院院刊,2005,29(1):91-95. [24] 姚咏明, 徐珊, 盛志勇. 高迁移率族蛋白B1的组织损伤效应及其干预途径[J]. 中国医学科学院学报,2007,29(4):459-465. [25] 濮健峰, 王梅芳, 潘四磊, 等. 超声引导下以旋髂深动脉为标记的髂腹股沟-髂腹下神经阻滞在老年斜疝手术中的应用[J]. 临床麻醉学杂志,2017,33(10):974-976. doi: 10.3969/j.issn.1004-5805.2017.10.010 [26] Yilmazlar A, Bilgel H, Donmez C, et al. Comparison of ilioinguinal-iliohypogastric nerve block versus spinal anesthesia for inguinal herniorrhaphy[J]. Southern Medical Journal,2006,99(1):48-51. doi: 10.1097/01.smj.0000197298.48311.80 [27] Willschke H, Bösenberg A, Willschke A, et al. Ultrasonography-guided rectus sheath block in paediatricanaesthesia-a new approach to an old technique[J]. British Journal of Anaesthesia,2006,97(2):244-249. doi: 10.1093/bja/ael143 [28] 祝胜美. 积极推动舒适化医疗服务模式的转变[J]. 现代实用医学,2011,23(3):247-249. doi: 10.3969/j.issn.1671-0800.2011.03.003 [29] Khalil K, Boutrous M, Irani A, et al. Operative intercostal nerve blocks with long-acting bupivacaine liposome for pain control after thoracotomy[J]. The Annals of Thoracic Surgery,2015,100(6):2013-2018. doi: 10.1016/j.athoracsur.2015.08.017 [30] 国家卫生健康委员会医管中心加速康复外科专家委员会. 中国加速康复外科围手术期非甾体抗炎药临床应用专家共识[J]. 中华普通外科杂志,2019,34(3):283-288. doi: 10.3760/cma.j.issn.1007-631X.2019.03.032 [31] 王天龙, 梅伟. 围手术期多模式镇痛低阿片方案是加速老年患者术后康复的关键[J]. 中华 医学杂志,2021,101(3):167-169. [32] 秦玲, 薛晓明. 患者疼痛管理研究进展[J]. 中国护理管理,2016,16(1):121-124. -






 下载:
下载: