Application of Pneumoperitoneum Free Transvaginal Natural Orifice Endoscopic Surgery in Ectopic Pregnancy and Related Factors of Operation Time
-
摘要:
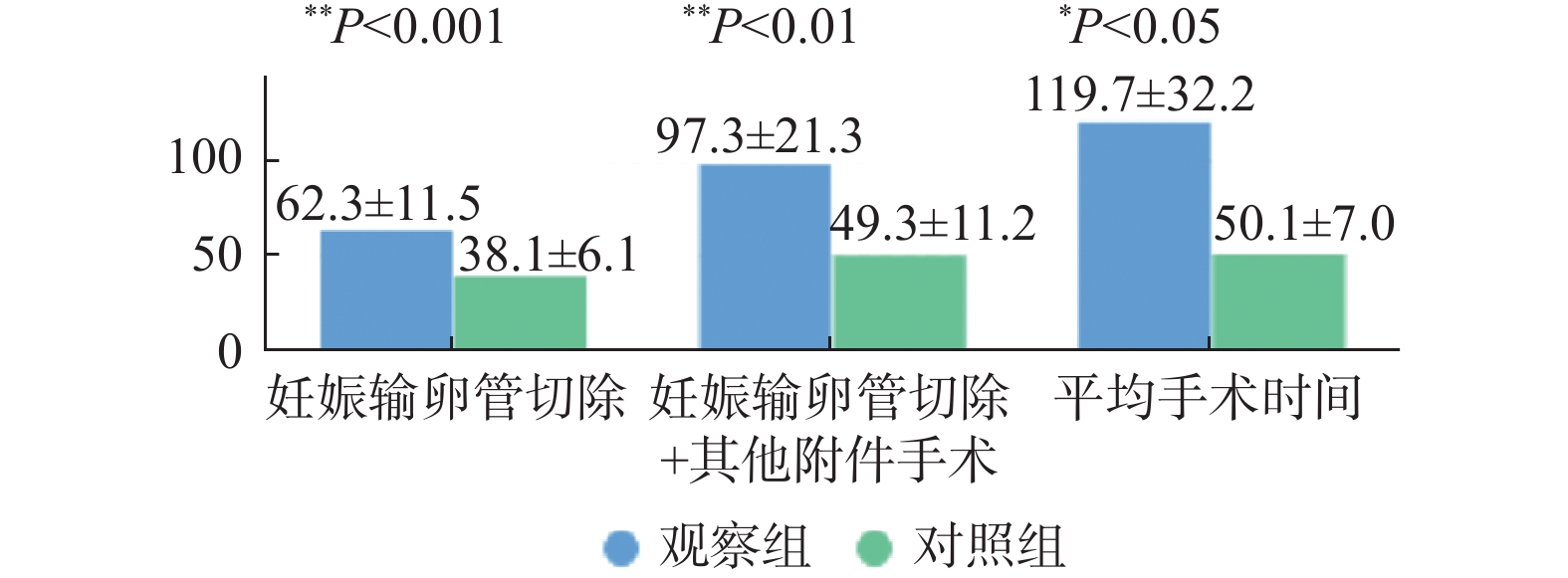
目的 探讨无气腹经阴道自然腔道内镜手术在异位妊娠中的运用及开展初期影响手术时间的相关因素。 方法 选取2020年7月至2021年11月昆明市第一人民医院收治的生命体征平稳、具有异位妊娠手术指征、估计内出血 < 800 mL的23名患者为研究对象,实施无气腹v-NOTES妊娠输卵管切除,选取同期行经腹多孔腹镜妊娠输卵管切除术的23名患者为对照组。 结果 23例观察组患者成功切除妊娠输卵管,未出现感染、直肠损伤等手术并发症。观察组手术时间长于对照组(P < 0.001),观察组与对照组术后排气时间及住院时间,差异无统计学意义(P > 0.05),观察组术口NRS评分及术后首次下床时间短于对照组,差异有统计学意义(P < 0.05)。对v-NOTES下妊娠输卵管切除的手术时间进一步分析发现镜下操作时间显著长于建立入路及缝合阴道黏膜时间,差异有统计学意义(P < 0.001),镜下操作时间随开展手术例数增加逐渐缩短。建立入路和缝合阴道黏膜时间因既往分娩方式不同存在差异,有阴道分娩史者最短,差异无统计学意义(P > 0.05),自开展第11例开始建立入路手术时间趋于稳定。 结论 v-NOTES下输卵管切除可安全有效的用于异位妊娠的手术治疗,应选择生命体征平稳、盆腔积液少、无严重盆腔粘连的患者进行手术。无气腹v-NOTES降低手术难度,避免气腹带来的风险,利于术中麻醉管理,增加手术安全性,同时避免使用一次性Port,不增加患者经济负担,适合在基层医院开展。技术开展初期手术时间与患者既往分娩史、盆腔积液量、术者的手术例数相关。 Abstract:Objective To investigate the application of pneumoperitoneum transvaginal natural orifice endoscopic surgery in ectopic pregnancy and the related factors affecting the operation time in the initial stage. Methods A total of 23 patients who were admitted to Kunming First People’s Hospital from July 2020 to November 2021, with stable vital signs, indicating for ectopic pregnancy surgery, and estimated internal bleeding < 800 mL, were selected as the study subjects. v-NOTES pregnancy tubal resection without air was performed. Another 23 patients who underwent peritoneal porous peritoneoscope tubal resection were selected as the control group. Results 23 patients in observation group were successfully resected without complications such as infection and rectal injury. The operation time of observation group was significantly longer than that of control group (P < 0.001). There was no significant difference in postoperative exhaust time and hospital stay between the observation group and the control group (P > 0.05). The NRS score and the first time out of bed after operation in the observation group were lower than those in the control group, and the differences were statistically significant (P < 0.05). Further analysis of the operation time of pregnancy tubal resection under v-NOTES showed that the operation time under the laparoscope was significantly longer than the time of establishing the approach and suturing the vaginal mucosa, and the difference was statistically significant (P < 0.001), and the time of laparoscopic operation gradually shortened with the increase of the number of cases undergoing surgery. The time to establish the approach and suture the vaginal mucosa was different according to the previous delivery mode, and those with a history of vaginal delivery had the shortest time, (P > 0.05)and the difference was not statistically significant. Conclusion v-NOTES salpingectomy is safe and effective for the surgical treatment of ectopic pregnancy. Patients with stable vital signs, less pelvic effusion, and no severe pelvic adhesions should be selected for surgery. Pneumoperitoneum v-NOTES reduces the difficulty of surgery by avoiding the risk of pneumoperitoneum, and is beneficial to intraoperative anesthesia management. It increases the safety of surgery by avoiding the use of disposable port, which does not increase the economic burden of patients, and is suitable for primary hospitals. The initial operation time was correlated with the patient’s previous delivery history, the volume of pelvic effusion, and the number of surgical cases. -
表 1 2组患者临床资料($ \bar x \pm s $)
Table 1. Clinical data of the two groups ($\bar x \pm s $)
组别 年龄(岁) BMI 附件包块直径(cm) 子宫前凹积液(cm) 子宫后凹积液(cm) 术前Hb(g/L) 观察组 31.6 ± 4.3 22.7 ± 2.7 2.4 ± 1.1 0.4 ± 0.8 0.6 ± 1.0 132.4 ± 11.5 对照组 33.4 ± 6.8 20.0 ± 2.2 2.3 ± 0.6 0.5 ± 1.0 0.5 ± 1.0 125.5 ± 12.6 t −1.122 3.772 0.593 −0.466 0.014 1.955 P 0.268 0.441 0.556 0.644 0.989 0.057 表 2 观察组各手术阶段时间比较[($ \bar x \pm s $),min]
Table 2. The time of each operation stage was compared in the observation group [($ \bar x \pm s $),min]
手术阶段 最小值 最大值 平均值 ± 标准差 建立入路 10 81 32.1 ± 19.7 镜下操作 26 139 67.8 ± 32.1 缝合阴道黏膜 6 53 19.6 ± 11.5 总手术时长 52 187 119.7 ± 32.2 表 3 不同分娩史手术时间比较[($ \bar x \pm s $),min]
Table 3. Comparison of operation time with different labor history [($ \bar x \pm s $),min]
手术阶段 分娩史 F P 无妊娠
分娩史剖宫
产史阴道
分娩史建立入路 34.2 ± 12.3 28.8 ± 14.9 25.8. ± 9.8 0.074 0.803 缝合阴
道黏膜22.4 ± 8.3 18.7 ± 10.4 20.4 ± 11.6 0.302 0.770 表 4 术后情况比较($ \bar x \pm s $ )
Table 4. Comparison of postoperative conditions ($\bar x \pm s $)
组别 排气时间
(h)住院时间
(d)术口NRS
评分首次下床
时间(h)观察组 19.9 ± 12.1 3.7 ± 0.9 0.7 ± 0.9 13.2 ± 7.1 对照组 23.2 ± 10.4 4 ± 1 2.1 ± 1.3 18.2 ± 4.7 t 0.459 0.944 −4.23 1.873 P 0.649 0.35 < 0.01* 0.034* *P < 0.05。 -
[1] 孙静,隋孟松. 经阴道自然腔道内镜手术在妇科良性疾病中的应用[J]. 中国实用妇科与产科杂志,2019,35(12):1315-1318. [2] Lee C L,Wu K Y,Su H,et al. Transvaginal natural-orifice transluminal endoscopic surgery(NOTES)in adnexal procedures[J]. J Minim Invasive Gynecol,2012,19(4):509-513. [3] Xu B,Liu Y,Ying X,et al. Transvaginal endoscopic surgery for tubal ectopic pregnancy[J]. JSLS,2014,18(1):76-82. doi: 10.4293/108680813X13693422519875 [4] Sarah V P,Jan B. Natural orifice transluminal endoscopic surgery ( NOTES ) salpingectomy for ectopic pregnancy:A first series demonstrating how a new surgical technique can be applied in a low - resource setting[J]. GynecolSurg,2015,12(4):299-302. [5] 刘海元,陈欣,孙大为,等. 经阴道自然腔道内镜手术在异位妊娠中的应用八例分析[J]. 中华腔镜外科杂志(电子版),2018,11(1):20-23. [6] 陈艳,陈诗慧,刘娟. 经阴道自然腔道内镜手术与经脐单孔腹腔镜手术在妇科良性疾病中应用比较的Meta分析[J]. 实用妇产科杂志,2021,37(12):929-934. [7] 曲思娆,赵曼曼,李全红,等. 无气腹V-NOTES与传统腹腔镜治疗卵巢囊肿临床疗效比较[J]. 中华腔镜外科杂志(电子版),2021,14(4):217-220. [8] 唐瑶,史梦茹,许鑫玥,等. 经阴道单孔腹腔镜行异位妊娠手术效果[J]. 中国计划生育学杂志,2022,30(2):416-418,423. [9] 王惠,彭继蓉,田黇,等. 基于ERAS理念下良性卵巢囊肿患者经阴道自然腔道内镜手术与经脐单孔腹腔镜手术术后恢复的对比研究[J]. 中华肿瘤防治杂志,2020,27(S1):134-135. [10] 戴金城,潘汉斌,凌幼霞,等. 无腹壁悬吊无气腹经阴道自然腔道内镜异位妊娠手术21例可行性和安全性分析[J]. 中外医疗,2021,40(31):65-67,76. [11] 曲思娆,赵曼曼,李全红,等. 无气腹经阴道自然腔道内镜手术在妇科良性疾病中的应用[J]. 中国妇产科临床杂志,2022,23(4):415-416. [12] 张强,张凌,查莉,等. 经阴道内镜手术在输卵管妊娠中的运用探索[J]. 中国计划生育和妇产科,2019,11(8):33-36. [13] Ozceltik G,Simsek D,Hortu I,et al. Transvaginal natural orifice transluminal endoscopic surgery for ectopic pregnancy[J]. J Obstet Gynaecol Res,2022,48(3):843-849. [14] Chen X,Liu H,Sun D,et al. Transvaginal natural orifice transluminal endoscopic surgery for tubal pregnancy and a device innovation from our institution[J]. J Minim Invasive Gynecol,2019,26(1):169-174. doi: 10.1016/j.jmig.2018.05.013 -






 下载:
下载: