Effect of Different Intestinal Surgical Methods on Prognosis of Patients with Intestinal Invasive Epithelial Ovarian Cancer
-
摘要:
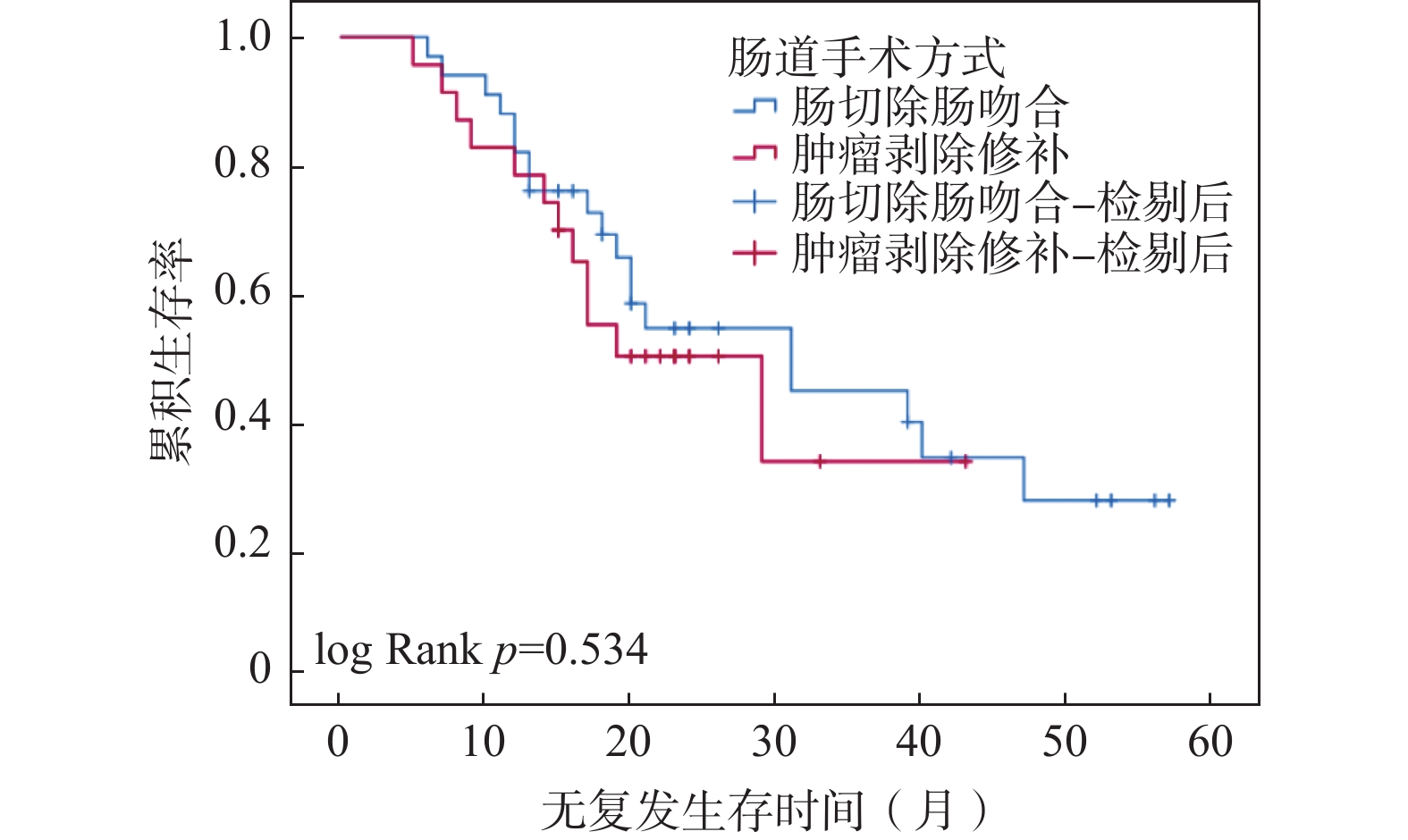
目的 比较受累部位肠切除和局部肿瘤剥除2种手术方式对肠道转移上皮性卵巢癌患者预后的影响。 方法 回顾性分析2017年6月至2021年6月在云南省肿瘤医院妇科由同1位妇瘤专家及其团队行肿瘤细胞减灭术并涉及肠道手术的晚期上皮性卵巢癌患者的临床资料,比较受累部位肠切除与保留肠管的局部肿瘤剥除2种手术方式的安全性及可行性。 结果 共纳入56例患者,33例(58.9%)行肠切除术,23例(41.1%)行肿瘤剥除,2组患者在满意减瘤率方面,差异无统计学意义(63.6%,87.0%,P > 0.05);在24.5个月(18.75~42.75)的中位随访时间中,肠切除组和肿瘤剥除组的复发率分别为57.6%、42.4%,死亡率分别为78.8%、82.6%,中位无复发生存期分别为31个月、19个月,差异均无统计学意义(P > 0.05);肠切除组较肿瘤剥除组手术时间更长、手术难度更大、术中失血量及输血量更多、术后并发症发生率更高,差异有统计学意义(P < 0.05)。 结论 卵巢癌肿瘤细胞减灭术中行肠切除及肿瘤剥除患者的减瘤结局与生存情况差异无统计学意义,但术中切除肠道可能使患者面临更多的并发症及更差的生活质量。因此,术中应结合肿瘤浸润肠壁的深度、侵犯肠道的范围及肿瘤的可分离性充分评估,尽可能保留肠道,以减少术后并发症。 Abstract:Objective To investigate the effect of intestinal segment resection and local tumor removal on the prognosis of patients with intestinal metastatic epithelial ovarian cancer. Methods The clinical data of the patients who were admitted to Yunnan Province Tumor Hospital with advanced epithelial ovarian cancers from June 2017 to June 2021 were reviewed. All of the patients were treated by the same woman tumor expert of the Department of Gynecology and his team and the safety and feasibility of two kinds of operation methods were compared. Results Among 56 patients, 33 (58.9%) underwent the intestinal resection and anastomosis, and 23 (41.1%) underwent the intestinal tumor removal and bowel repair. There was no significant difference in satisfactory tumor reduction rate between the two groups (63.6%, 87.0%, P > 0.05). In the median follow-up time of 24.5 months (18.75~42.75), the recurrence rates in the enterectomy group and the tumor excision group were 57.6% and 42.4% respectively, the mortality rates were 78.8% and 82.6%, respectively, and the median relapse-free survival time were 31 months and 19 months, respectively, with no statistical significance (P > 0.05). Operations in intestinal resection group were carried out with longer time, more difficulties, more blood loss and more blood transfusion. The incidence of postoperative complications was higher, and the difference was statistically significant (P < 0.05). Conclusion There is no significant difference in the tumor reduction outcome and survival of patients with ovarian cancer tumor cell reduction after the intestinal resection and tumor removal, but the patients may face more complications and poorer quality of life after the intestinal resection. Therefore, during the operation, the depth of tumor invasion of the intestinal wall, the scope of intestinal invasion and the separability of the tumor should be fully assessed, so as to preserve the intestinal tract as much as possible, and to reduce the occurrence of postoperative complications. -
Key words:
- Epithelial ovarian cancer /
- Debulking surgery /
- Intestinal surgery /
- Prognosis
-
表 1 2组患者一般资料及手术情况比较[(
$ \bar x \pm s $ )n(%)/M(P25,P75)]Table 1. Comparison of general information and operation between two groups[(
$ \bar x \pm s $ )n(%)/M(P25,P75)]临床特征 肠切除组 肿瘤剥除组 t/Z/χ2 P 年龄(岁) 51.700 ± 7.346 54.700 ± 10.191 −1.281 0.210 BMI(kg/m2) 22.800 ± 3.690 23.090 ± 3.140 −0.301 0.780 FIGO分期 5.774 0.217 IIIA /IIIB期 1(1.8) 1(1.8) IIIC期 25(44.6) 16(27.6) IV期 7(12.5) 6(10.8) 组织类型 1.599 0.660 浆液性腺癌 31(55.4) 22(39.3) 子宫内膜样腺癌 2(3.6) 1(1.8) 新辅助化疗 3.178 0.075 是 7(12.5) 10(17.9) 否 26(46.4) 13(23.2) 是否满意减瘤 3.759 0.053 是 21(63.6) 20(87.0) 否 12(36.4) 3(13.0) 浸润深度 浆膜层 11(33.3) − 肌层 18(54.5) − 黏膜层 4(12.1) − 术后并发症 4.250 0.039* 是 27(81.8) 13(56.5) 否 6(18.2) 10(43.5) 手术复杂性得分(分) 7(6,8) 4(3.0,5.5) −4.859 <0.001* 术后住院天数(天) 14(11,16) 13(11,17) −0.561 0.575 术前CA125水平(U/mL) 1116(387,2660.5) 452(100.8,1472) −1.307 0.191 腹水量(mL) 800(150,2000) 400(20,3000) −0.344 0.731 手术历时(min) 300(260,362) 240(210,300) −2.735 0.006* 估计失血量(mL) 1050(500,1750) 500(300,1000) −2.454 0.014* 术中输血量(mL) 1300(850,2000) 900(0,1200) −2.499 0.012* 是否复发 0.160 0.689 是 19(57.6) 12(42.4) 否 14(52.2) 11(47.8) 是否死亡 0.125 0.723 是 26(78.8) 19(82.6) 否 7(21.2) 4(17.4) *P < 0.05。 表 2 术后并发症发生情况[n(%)]
Table 2. The incidence of postoperative complications [n(%)]
并发症 肠切除组 肿瘤剥除组 合计 感染 12(36.4) 5(21.7) 17(30.2) 胸腔积液 7(21.2) 4(17.4) 11(19.6) 输血 9(27.3) 0 9(16.1) 肠瘘 2(6.1) 0 2(3.6) 血栓栓塞 5(15.2) 1(4.3) 6(10.7) 肠梗阻 3(9.1) 2(8.7) 5(8.9) 切口延迟愈合 3(9.1) 1(4.3) 4(7.1) 大便习惯改变 16(48.5) 7(30.4) 23(41.1) 表 3 2组患者术后并发症严重程度比较[n(%)]
Table 3. Comparison of the severity of postoperative complications between the two groups [n(%)]
分组 合计(n) CDC 0-2分 CDC 3-5分 χ2 P 肠切除 33 22(66.7) 11(33.3) 1.756 0.185 肿瘤剥除 23 19(82.6) 4(17.4) -
[1] Sung H,Ferlay J,Siegel R L,et al. Global Cancer Statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin,2021,71(3):209-249. doi: 10.3322/caac.21660 [2] Chang S J,Hodeib M,Chang J,et al. Survival impact of complete cytoreduction to no gross residual disease for advanced-stage ovarian cancer: A meta-analysis[J]. Gynecol Oncol,2013,130(3):493-498. doi: 10.1016/j.ygyno.2013.05.040 [3] Obermair A,Hagenauer S,Tamandl D,et al. Safety and efficacy of low anterior en bloc resection as part of cytoreductive surgery for patients with ovarian cancer[J]. Gynecol Oncol,2001,83(1):115-120. doi: 10.1006/gyno.2001.6353 [4] Bryant C L,Lunniss P J,Knowles C H,et al. Anterior resection syndrome[J]. The Lancet Oncology,2012,13(9):403-408. doi: 10.1016/S1470-2045(12)70236-X [5] Kranawetter M, Ataseven B,Grimm C,et al. Low anterior resection syndrome (LARS) in patients with epithelial ovarian cancer after primary debulking surgery[J]. Gynecol Oncol,2019,154(3):577-582. doi: 10.1016/j.ygyno.2019.06.015 [6] Bidzinski M,Derlatka P,Kubik P,et al. The evaluation of intra-and postoperative complications related to debulking surgery with bowel resection in patients with FIGO stage III-IV ovarian cancer[J]. Int J Gynecol Cancer,2007,17(5):993-997. doi: 10.1111/j.1525-1438.2007.00896.x [7] Aletti G D,Podratz K C,Jones M B,et al. Role of rectosigmoidectomy and stripping of pelvic peritoneum in outcomes of patients with advanced ovarian cancer[J]. J Am Coll Surg,2006,203(4):521-526. doi: 10.1016/j.jamcollsurg.2006.06.027 [8] Hertel H,Diebolder H,Herrmann J,et al. Is the decision for colorectal resection justified by histopathologic findings: A prospective study of 100 patients with advanced ovarian cancer[J]. Gynecol Oncol,2001,83(3):481-484. doi: 10.1006/gyno.2001.6338 [9] Kim M,Suh D H,Park J Y,et al. Survival impact of low anterior resection in patients with epithelial ovarian cancer grossly confined to the pelvic cavity:A Korean multicenter study[J]. J Gynecol Oncol,2018,29(4):60-61. doi: 10.3802/jgo.2018.29.e60 [10] Vergote I,Gonzalez-Martin A,Lorusso D,et al. Clinical research in ovarian cancer: Consensus recommendations from the Gynecologic Cancer InterGroup[J]. Lancet Oncol,2002,23(8):374-384. [11] Di Donato V,Di Pinto A,Giannini A,et al. Modified fragility index and surgical complexity score are able to predict postoperative morbidity and mortality after cytoreductive surgery for advanced ovarian cancer[J]. Gynecol Oncol,2021,161(1):4-10. doi: 10.1016/j.ygyno.2020.08.022 [12] Dindo D,Demartines N,Clavien P A,et al. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey[J]. Ann Surg,2004,240(2):205-213. doi: 10.1097/01.sla.0000133083.54934.ae [13] Rustin G J,Vergote I,Eisenhauer E,et al. Definitions for response and progression in ovarian cancer clinical trials incorporating RECIST 1.1 and CA 125 agreed by the Gynecological Cancer Intergroup (GCIG)[J]. Int J Gynecol Cancer,2011,21(2):419-423. doi: 10.1097/IGC.0b013e3182070f17 [14] Vito Andrea C,Uccella S, Sozzi G,et al. Primary site disease and recurrence location in ovarian cancer patients undergoing primary debulking surgery vs. interval debulking surgery[J]. Eur J Surg Oncol,2021,47(5):1075-1082. doi: 10.1016/j.ejso.2020.09.014 [15] Gallotta V,Fanfani F,Vizzielli G,et al. Douglas peritonectomy compared to recto-sigmoid resection in optimally cytoreduced advanced ovarian cancer patients: Analysis of morbidity and oncological outcome[J]. Eur J Surg Oncol,2011,37(12):1085-1092. doi: 10.1016/j.ejso.2011.09.003 [16] Plotti F,Montera R,Aloisi A,et al. Total rectosigmoidectomy versus partial rectal resection in primary debulking surgery for advanced ovarian cancer[J]. Eur J Surg Oncol,2016,42(3):383-390. doi: 10.1016/j.ejso.2015.12.001 [17] Park J Y,Seo S S,Kang S,et al. The benefits of low anterior en bloc resection as part of cytoreductive surgery for advanced primary and recurrent epithelial ovarian cancer patients outweigh morbidity concerns[J]. Gynecol Oncol,2006,103(3):977-984. doi: 10.1016/j.ygyno.2006.06.004 [18] Park S J,Mun J,Lee E J,et al. Clinical phenotypes of tumors invading the rectosigmoid colon affecting the extent of debulking surgery and survival in advanced ovarian cancer[J]. Front Oncol,2021,22(11):631-673. -






 下载:
下载: