Evaluation of Therapeutic Effect of Transabdominal and Transvaginal Ultrasound on Cesarean Scar Pregnancy
-
摘要:
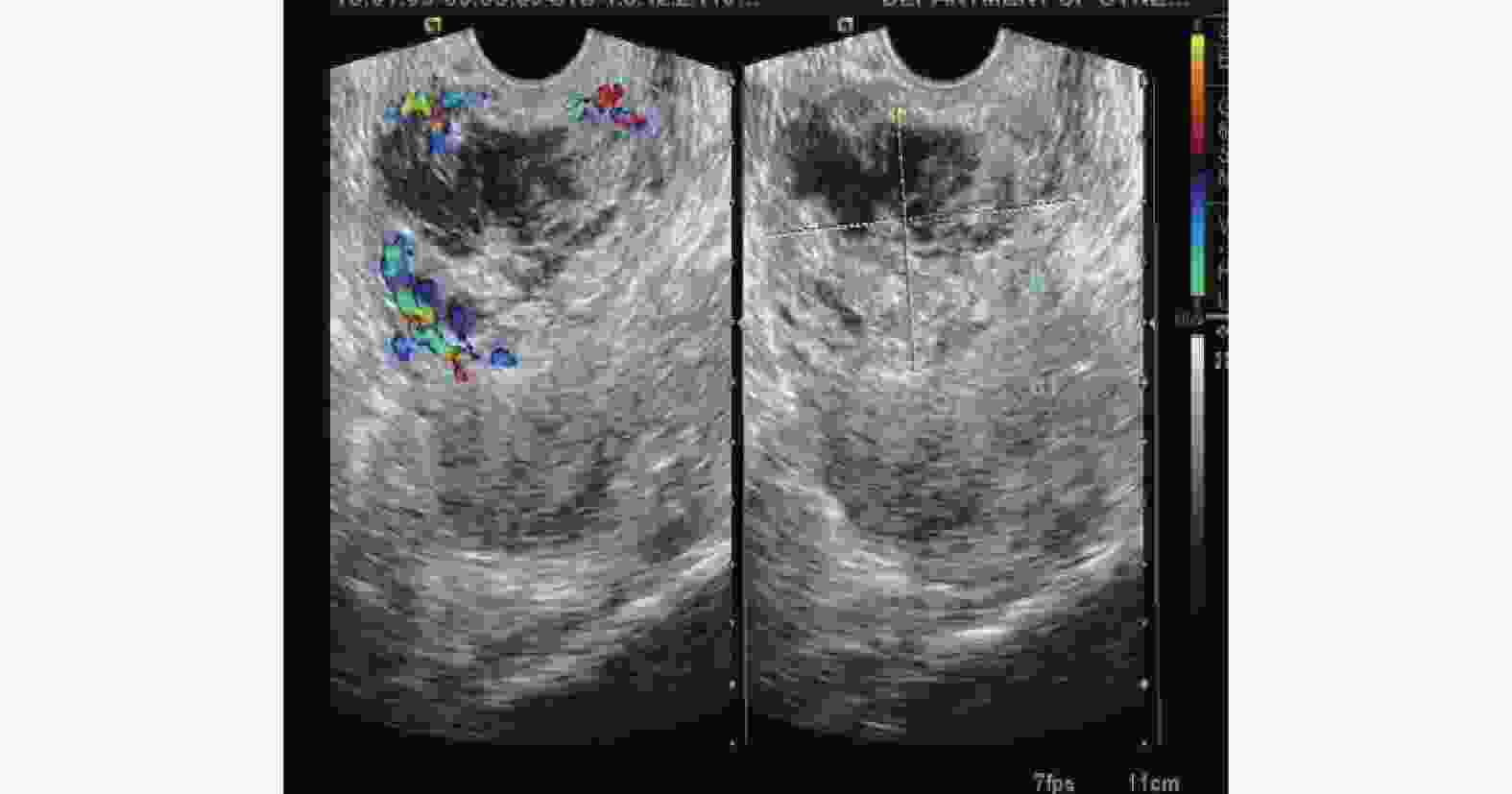
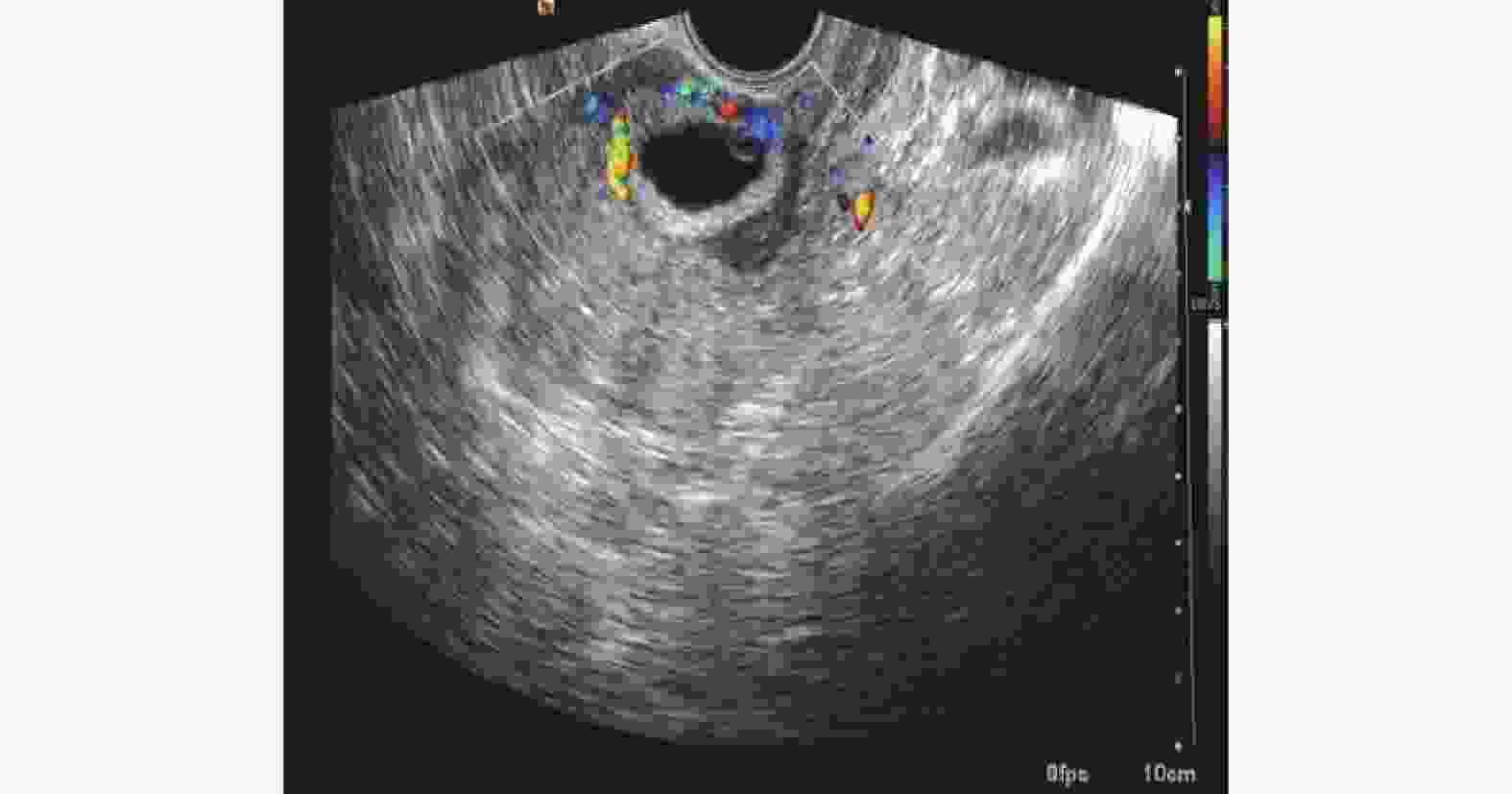
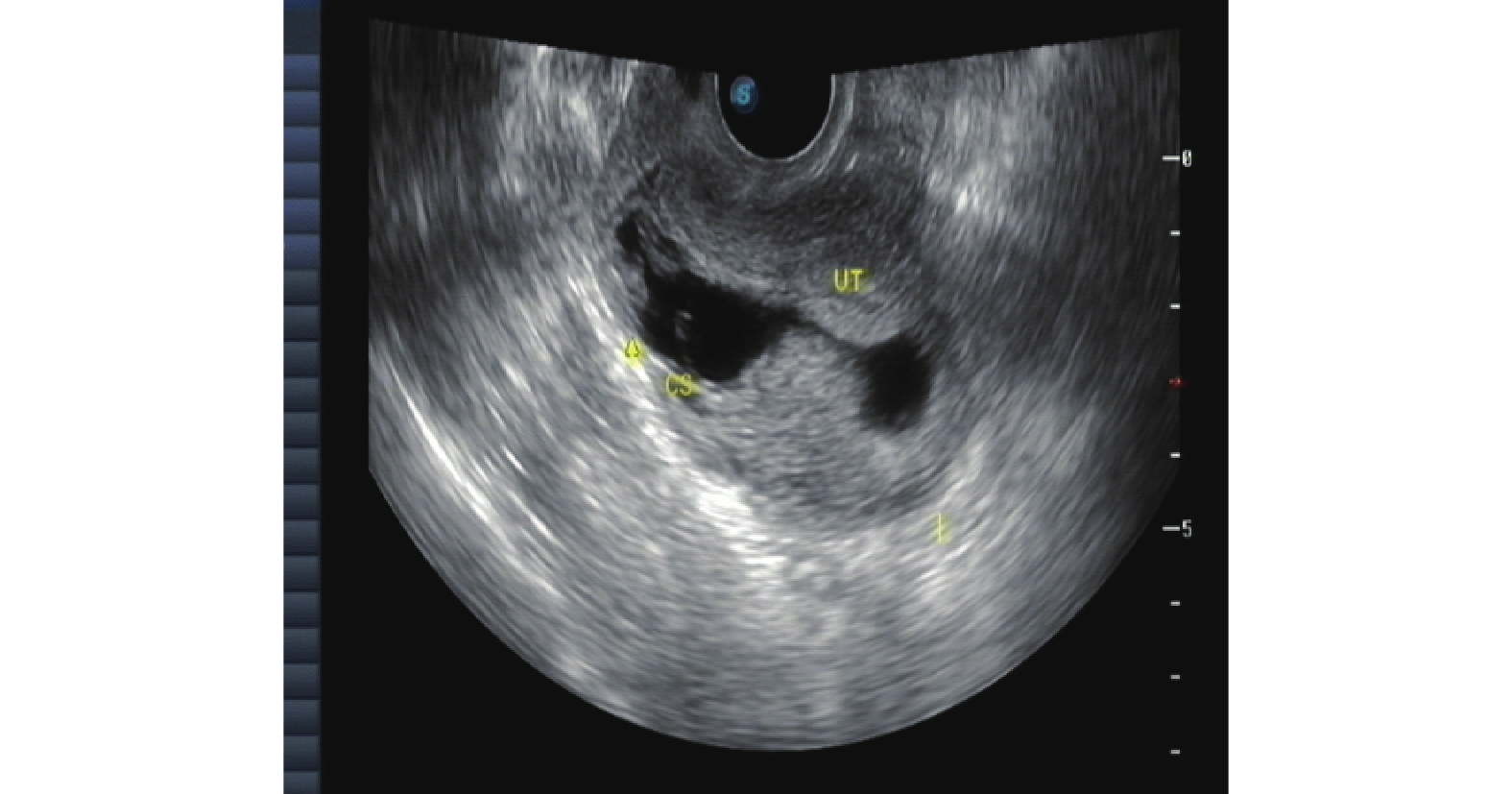
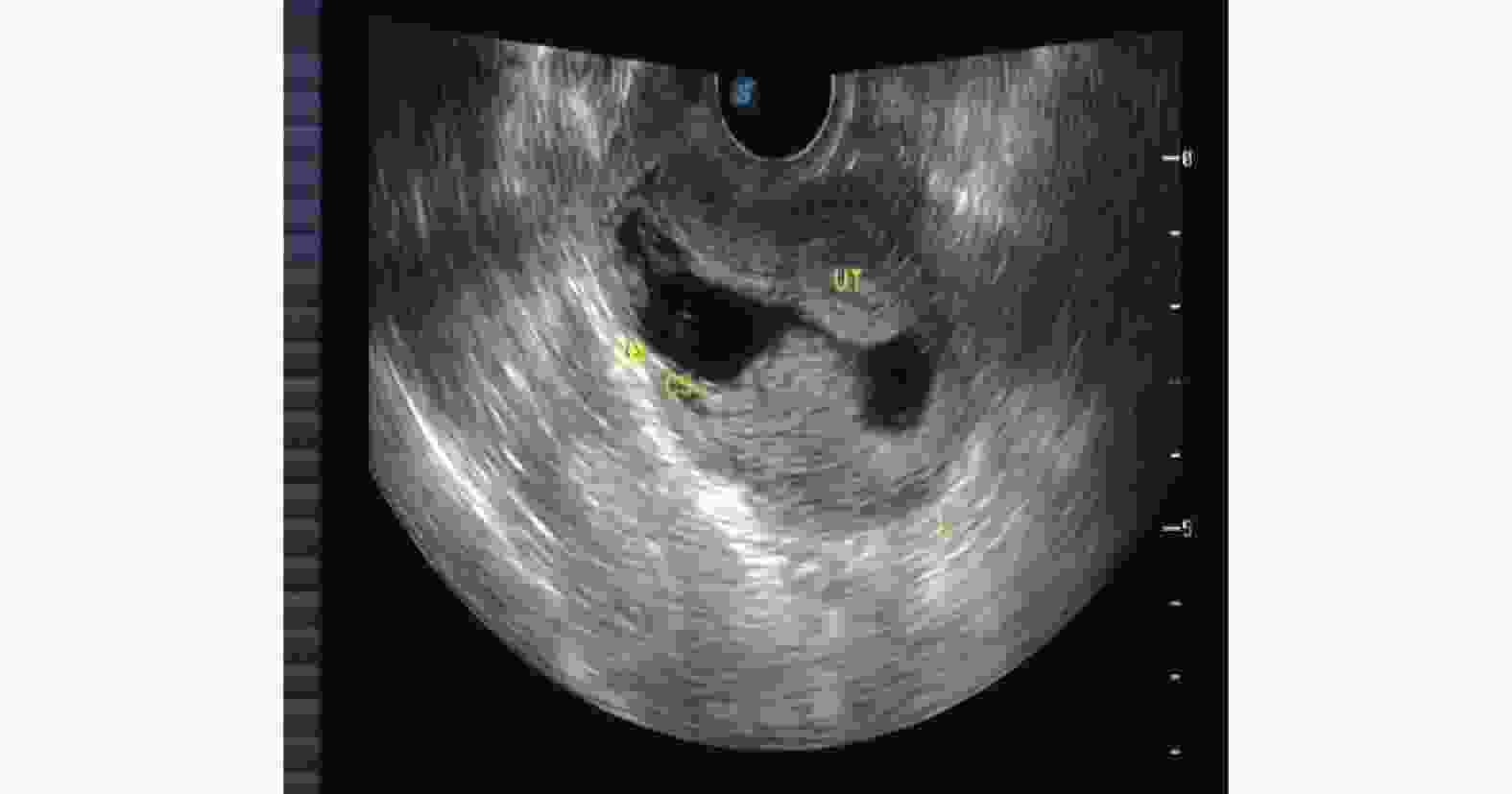
目的 探讨彩色多普勒超声对剖产瘢痕妊娠疗效的临床意义。 方法 收集2019年1月至2021年12月在云南省第一人民医院妇科诊治的82例CSP患者,应用超声对CSP诊疗过程临床价值的回顾性分析。用SPSS19.0对数据进行统计分析,组间比较采用卡方检验进行分析,采用配对t检验进行术前术后比较分析。 结果 B超对CSP分型诊断后选择个体化治疗方案结果差异有统计学意义(P < 0.05)。病灶面积越大,术后B超的异常概率越高且差异有统计学意义( P = 0.002);GSPⅡ型的术后异常比例高于Ⅰ型、Ⅲ型且差异有统计学意义(P = 0.027);手术方式方面宫腔鏡下病灶挖出术的术后异常比例低于B超引导下高危人流术、腹腔镜下病灶挖出术且差异有统计学意义(P = 0.002);剖宫产次数、病灶血供情况与术后B超的结果之间差异没有统计学意义(χ2值和P分别为1.300/0.558、--/0.059 )。同时个体化治疗须充分结合CSP的其他相关检验指标。 结论 经腹联合阴道彩色多普勒超声对子宫瘢痕妊娠疗效评估过程具有非常重要的临床价值。 Abstract:Objective To investigate the clinical significance of color Doppler ultrasound in the diagnosis and treatment of cesarean scar pregnancy. Methods A total of 82 CSP patients diagnosed and treated in the Department of Gynecology of Yunnan First People’s Hospital from January 2019 to December 2021 were collected, and their diagnosis and treatment processes were retrospectively analyzed. A retrospective analysis of the clinical value of ultrasound in the diagnosis and treatment of CSP was carried out. The results of statistical analysis of data by SPSS19.0, Chi square test analysis of inter group comparison and paired T test were used for the comparison and analysis before and after the surgery Results There was the statistical significance in selecting individualized treatment plan after the classification diagnosis of CSP by B-ultrasound. The larger the lesion area, the higher the abnormal probability of postoperative B-ultrasonography and the difference was statistically significant (P = 0.002); The abnormal rate of GSP type II was higher than that of type Ⅰ and type Ⅲ (P = 0.027); In terms of operation mode, the abnormal rate of hysteroscopic lesion extraction was lower than that of B-ultrasound guided high-risk abortion and laparoscopic lesion extraction, and the difference was statistically significant (P = 0.002); There was no significant difference between the number of cesarean section, the blood supply of the focus and the results of postoperative ultrasound (andP values were 1.300/0.558, -/0.059, respectively). At the same time, the individualized treatment should be fully combined with other relevant test indicators of CSP. Conclusion Transabdominal combined vaginal color Doppler ultrasound has a very important clinical value in the clinical diagnosis and treatment of uterine scar pregnancy. -
Key words:
- Ultrasound /
- Cesarean section /
- Scar pregnancy /
- Ultrasound classification
-
表 1 超声对CSP疗效影响因素分析[n(%)]
Table 1. Analysis of the influencing factors of ultrasound on the curative effect of CSP [n(%)]
指标 疗效术后B超 χ2 P 正常(n = 63例) 异常(n = 19例) 剖宫产次数 1 43(68.3) 13(68.4) 1.300 0.558 2 19(30.2) 5(26.3) 3 1(1.6) 1(5.3) 病灶大小 正常 63(100.0) 15(78.9) —— 0.002* 大 0(0.0) 4(21.1) 血供情况 正常 51(81.0) 19(100.0) —— 0.059 丰富 12(19.0) 0(0.0) CSP的分型 Ⅰ型 33(52.4) 8(42.1) 7.313 0.027* Ⅱ型 14(22.2) 10(52.6)a Ⅲ型 16(25.4) 1(5.3)b 手术方式 B超引导下高危人流术 24(38.1) 16(84.2) 11.872 0.002* 宫腔鏡下病灶挖出术 15(23.8) 1(5.3)c 腹腔镜下病灶挖出术 24(38.1) 2(10.5)d 注:“——”为精确概率法;a:与Ⅰ型比较,差异有统计学意义;b:与Ⅱ型比较,差异有统计学意义;c:与B超引导下高危人流术比较,差异有统计学意义;d:与宫腔鏡下病灶挖出术比较,差异有统计学意义。*P < 0.05。 表 2 手术前后的HCG、孕酮的差异性分析
Table 2. Difference analysis of HCG and progesterone before and after operation
指标 $\bar x \pm s $ 标准误 95%CI t P 术前血HCG - 术后血HCG 24701.34 ± 41890.54 4626.04 (15496.98,33905.70) 5.340 < 0.001* 术前孕酮 - 术后孕酮 45.39 ± 26.78 3.11 (39.19,51.60) 14.583 < 0.001* *P < 0.05。 -
[1] 谢幸, 孔北华, 段涛. 异位妊娠. 妇产科学[M]第9版. 北京: 人民卫生出版社, 2018: 80-81. [2] 希阳,史安平,周永强,等. 剖宫产瘢痕妊娠治疗研究进展[J]. 陕西医学杂志,2019,48(8):1102-1105. doi: 10.3969/j.issn.1000-7377.2019.08.040 [3] Sholapurkaps L. Etiology of cesarean uterine scar defect (niche):Detailed critical analysis of hypotheses and prevention strategies and peritoneal closure debate[J]. J Clin Med Res,2018,10(3):166-173. doi: 10.14740/jocmr3271w [4] 韦晓昱,于晓兰. 剖宫产术后瘢痕妊娠的处理[J]. 中国临床医生杂志,2022,50(7):763-765. doi: 10.3969/j.issn.2095-8552.2022.07.003 [5] Jurlovic D,Hillaby K,WoelferB,et al. Fimt-trimester diagnosis and mangemengt of pregnancies implanted into the lower uterine segment cesarean section scar[J]. Ultrasoimd Obstet Gynecol,2003,21(3):220-227. [6] 涂艳萍,王丽敏,黄苑铭,等. 超声对剖宫产术后子宫瘢痕妊娠分型的临床价值研究[J]. 中国超声医学杂志,2018,34(4):339-341. doi: 10.3969/j.issn.1002-0101.2018.04.018 [7] Timor-Tritsch Ilan BUca,Danilo,Di Mascio Daniele,et al. Outcome of cesarean scar pregnancy according to gestationalage atdiagnosis: A systematic review and meta-nanlysis[J]. Eur J Obstet Gyn R B,2021,258(52):1421-1423. [8] 马彦,徐云. 剖宫产术后子宫瘢痕妊娠的诊治进展[J]. 中国妇产科临床杂志,2017,18(3):284-285. doi: 10.13390/j.issn.1672-1861.2017.03.040 [9] 胡锐,朱俊勇,袁昊,等. 剖宫产术后子宫瘢痕妊娠发病机制的研究进展[J]. 中华妇产科杂志,2014,49(1):61-63. doi: 10.3760/cma.j.issn.0529-567x.2014.01.018 [10] Glenn TL, Bembry J, Findley A D, et al, Cesarean scar ectopic pregnancy: Current management strategies[J]. Obstet Gynecol Surv, 2018, 73(5): 293-302. [11] 梁喜霞,谢许萍,卢燕敏,等. 经阴道超声对剖宫产瘢痕妊娠的诊断准确性及其影响因素分析[J]. 微创医学,2021,16(6):753-756. [12] LIY,LUL,WANGW,et al. Retrospective study of patients with cesareanscar pregnancies treated by uterine artery chemoembolization and curettage[J]. Int J Gynaecol Obstet,2018,143(2):172-177. doi: 10.1002/ijgo.12636 [13] Society For Maternal-Fetal Medicine. (SMFM)consult series#49: Cesarean scar pregnancy[J]. Am J Obstet Gynecol,2020,222(5):B2-B14. doi: 10.1016/j.ajog.2020.01.030 [14] 孙阳. 经腹超声和经阴道超声对剖宫产术后子宫瘢痕妊娠的诊断价值比较[J], 医学信息2021, 34(19): 175-177. [15] 严静,楼叶琳,陈静婉,等. 多途径超声联合检查用于剖宫产子宫瘢痕妊娠分型诊断的临床观察[J]. 中华全科医学,2021,19(3):463-465,475. [16] 邓玉艳,陆静,宋丁,等. 剖宫产瘢痕部位妊娠的超声分型及治疗效果的研究[J]. 实用妇产科杂志,2017,33(7):538-540. [17] 李康宁. 超声在剖宫产瘢痕妊娠术前诊断、风险评估及远期随访中的临床应用研究[D]. 北京: 北京协和医学院硕士学位论文, 2016 . [18] 中华医学会妇产科学分会计划生育学组. 剖宫产术后子宫瘢痕妊娠诊治专家共识(2016)[J]. 中华妇产科杂志,2016,51(8):568-572. doi: 10.3760/cma.j.issn.0529-567x.2016.08.003 [19] 韦晓昱,于晓兰. 子宫动脉栓塞术的相关并发症[J]. 中华围产医学杂志,2020,23(7):502-504. doi: 10.3760/cma.j.cn113903-20200109-00016 -





 下载:
下载: