Analysis of Nutritional Status and Immune Function of Tuberculosis Patients in Yunnan
-
摘要:
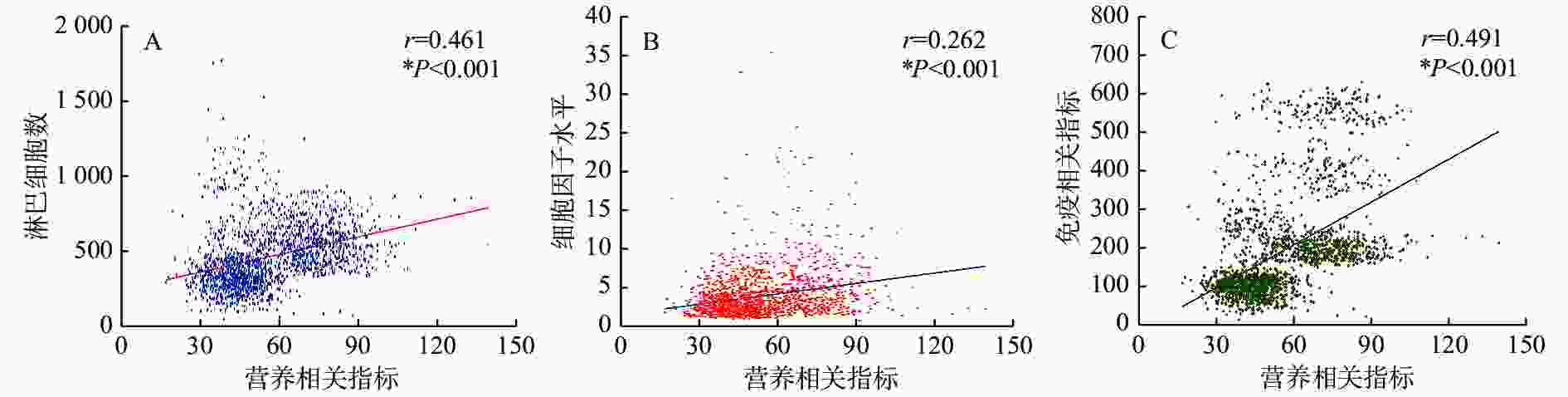
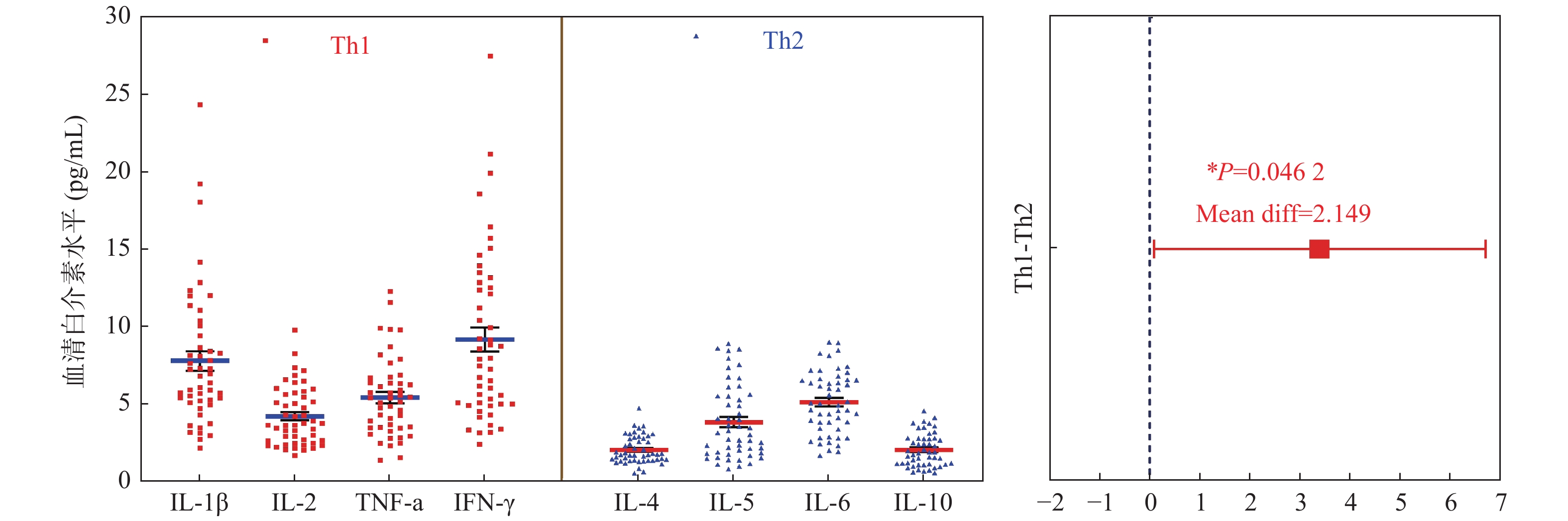
目的 探讨肺结核病患者营养状况及免疫功能的特点和意义。 方法 收集2021年3月至2022年3月在昆明市第三人民医院收治的1041例肺结核病患者为研究组,以同期健康体检者854例作为对照组。比较2组相关指标水平,分析肺结核病患者的营养状况及免疫功能的特点和关系。 结果 与对照组比较,研究组营养及免疫相关指标Hb、TP、Alb、Glob、A/G、PA、TC、TG、HDL、LDL、CD3+T、CD4+T、CD8+T、CD4+/CD8+、CD19+B、NK、NKT 表达降低(P均 < 0.05);细胞因子IL-1β、IL-8、IL-17水平升高,IL-4、IL-10、IL-12p70、IFN-γ水平降低,差异均有统计学意义(P < 0.05)。研究组中:肺结核病患者低血红蛋白、低白蛋白、高胆固醇、高甘油三酯、低高密度脂蛋白以轻度和中度为主,重度占比较少;Th1型细胞因子(IL-1β、IL-2、TNF-a、IFN-γ)较Th2型细胞因子(IL-4、IL-5、IL-6、IL-10 )水平高(P < 0.05);TP、TG、NKT水平男性高于女性,TC、CD3+T、CD4+T、CD8+T、IL-1β、IL-4、IL-10、IL-12p70表达则男性低于女性,差异均有统计学意义(P < 0.05);各年龄段相关指标经单因素方差分析,Hb、TC、TG、CD3+T、CD4+T、CD8+T、CD4+/CD8+、IL-1β表达差异均有统计学意义,其中41~60岁组和≥61岁组CD3+T、CD4+T、CD8+T计数较≤20岁组降低(P均 < 0.05);营养相关指标与淋巴细胞数、细胞因子水平及免疫相关指标经Spearman相关性分析都呈正相关(r = 0.461、0.262、0.491;P均 < 0.05)。 结论 云南省肺结核病患者营养状况及免疫功能较健康人群低,可能易发生轻度和中度营养不良,其免疫反应以Th1型为主,女性免疫功能及应答能力强于男性,老年患者免疫功能较差,患者营养状况可影响其免疫功能,二者间呈正相关。血清蛋白水平、淋巴细胞数及细胞因子水平可作为结核病患者营养状况和免疫功能的重要参考指标,对结核病的预防和治疗起积极作用。 Abstract:Objective To investigate the characteristics and significance of nutritional status and immune function in patients with pulmonary tuberculosis. Methods 1041 tuberculosis patients admitted to Kunming Third People’s Hospital from March 2021 to March 2022 were collected as the research group and 854 healthy subjects during the same period were selected as the control group. The levels of related indicators between the two groups were compared, and the characteristics and relationships of the nutritional status and immune function of tuberculosis patients were analysed. Results Compared with the control group, the nutritional and immune-related indicators expressions of Hb, TP, Alb, Glob, A/G, PA, TC, TG, HDL, LDL, CD3+T, CD4+T, CD8+T, CD4+/CD8+ CD19+B, NK and NKT were decreased (all P < 0.05). The levels of cytokines IL-1β, IL-8, IL-17 were increased, and IL-4, IL-10, IL-12p70, IFN-γ were decreased (P < 0.05). In the research group, tuberculosis patients with low hemoglobin, low albumin, high cholesterol, high triglyceride, and low high-density lipoprotein were mainly mild and moderate, with a small proportion of severe; Th1 cytokines (IL-1β, IL-2, TNF-a, IFN-γ) were higher than Th2 cytokines (IL-4, IL-5, IL-6, IL-10) (P < 0.05); The levels of TP, TG and NKT were higher in males than those in females, and the expressions of TC, CD3+T, CD4+T, CD8+T, IL-1β, IL-4, IL-10 and IL-12p70 were lower than those in females (all P < 0.05); The relevant indicators of each age group analyzed with one-way ANOVA of variance showed that there were statistically significant differences in the expression of Hb, TC, TG, CD3+T, CD4+T, CD8+T, CD4+/CD8+, and IL-1β; The counts of CD3+T, CD4+T, CD8+T in the ≥61 year old group were significantly lower than those in the ≤20 year old group (all P < 0.05); Nutrition-related indicators were positively correlated with the number of lymphocytes, cytokine levels and immune-related indicators by Spearman correlation analysis (r = 0.461, 0.262, 0.491; P < 0.05). Conclusion The nutritional status and immune function of tuberculosis patients in Yunnan are lower than those of healthy people, which may be prone to mild and moderate malnutrition, and its immune response is mainly Th1 type. Women’s immune function and responsiveness are stronger than men’s, and elderly patients are often in poor immune function. The nutritional status of patients can affect their immune function and there is a positive correlation between them. Serum protein levels, lymphocyte counts and cytokine levels can be used as the important reference indicators for nutritional status and immune function in tuberculosis patients and play a positive role in the prevention and treatment of tuberculosis. -
Key words:
- Tuberculosis /
- Patient /
- Nutritional status /
- Immune function /
- Analyze
-
表 1 对照组和研究组相关检测指标水平比较 [
$ \bar x \pm s$ /M(P25,P75)]Table 1. Comparison of relevant detection index levels in controland study group [
$ \bar x \pm s$ /M(P25,P75)]相关指标 对照组(n = 854) 研究组(n = 1041) t'/U P Hb(g/L) 155.8 ± 16.74 120.4 ± 21.88 27.75 < 0.001* TP(g/L) 74.40 ± 5.864 66.9 ± 7.674 28.64 < 0.001* Alb(g/L) 42.97 ± 4.457 37.42 ± 5.516 28.52 < 0.001* Glob(g/L) 31.43 ± 5.953 28.35 ± 6.061 12.67 < 0.001* A/G 1.426 ± 0.356 1.369 ± 0.328 4.035 < 0.001* PA(mmol/L) 300.5 ± 87.29 222.6 ± 70.51 23.02 < 0.001* TC(mmol/L) 4.634 ± 1.042 4.193 ± 0.982 10.79 < 0.001* TG(mmol/L) 1.22(0.830,1.960) 1.06(0.790,1.465) 637362 < 0.001* HDL(mmol/L) 1.31(1.100,1.540) 1.02(0.830,1.220) 367655 < 0.001* LDL(mmol/L) 3.00(2.470,3.560) 2.64(2.140,3.160) 553012 < 0.001* CD3+T(个/μL) 1202 ± 499.1 1086 ± 456.4 963035 < 0.001* CD4+T(个/μL) 704.5 ± 308.4 628.3 ± 279.4 951581 < 0.001* CD8+T(个/μL) 460.6 ± 234.5 429.1 ± 217.8 1033269 < 0.001* CD4+/CD8+ 1.720 ± 0.763 1.644 ± 0.746 1049776 0.003* CD19+B (个/μL) 246.9 ± 163.4 218.3 ± 158.9 285140 < 0.001* NK (个/μL) 241.7 ± 169.1 207.1 ± 142.8 277918 < 0.001* NKT (个/μL) 194.0(135.3,299.0) 74.0(44.0,118.0) 110096 < 0.001* IL-1β (pg/mL) 3.30(1.710,6.120) 4.03(1.540,7.420) 1017339 0.005* IL-2 (pg/mL) 2.01(1.040,3.363) 1.72(1.080,3.095) 1114912 0.226 IL-4 (pg/mL) 1.65(1.190,2.520) 1.26(1.020,1.790) 829465 < 0.001* IL-5 (pg/mL) 2.13(1.030,3.260) 1.76(1.060,3.038) 1112062 0.106 IL-6 (pg/mL) 3.33(2.118,5.880) 3.18(1.850,6.505) 979359 0.188 IL-8 (pg/mL) 1.84(1.080,3.790) 1.85(1.233,4.740) 1068098 0.029* IL-10 (pg/mL) 1.33(0.890,2.090) 1.23(0.870,1.720) 1055485 < 0.001* IL-12p70 (pg/mL) 1.58(1.220,2.330) 1.48(1.130,2.003) 1031405 < 0.001* IL-17 (pg/mL) 1.86(1.280,3.400) 2.26(1.520,4.510) 917365 < 0.001* TNF-a (pg/mL) 1.70(1.170,2.650) 1.71(1.040,2.820) 931857 0.224 IFN-γ (pg/mL) 4.61(2.310,9.843) 3.65(2.350,8.188) 1069329 0.003* 经校正t检验和曼惠特尼U检验,*P < 0.05。 表 2 研究组相关指标程度分析 [n(%)]
Table 2. Analysis of the degree of relevant indicators in the study group [n(%)]
组别 低血红蛋白 低白蛋白 高胆固醇 高甘油三酯 低高密度脂蛋白 轻度 60 (41.38) 412 (80.63) 99 (60.36) 126 (63.00) 163 (30.41) 中度 58 (40.00) 92 (18.00) 56 (34.15) 71 (35.50) 241 (44.96) 重度 27 (18.62) 7 (1.37) 9 (5.49) 3 (1.50) 132 (24.63) 合计 145 511 164 200 536 表 3 不同性别相关检测指标比较 [
$ \bar x \pm s$ /M(P25,P75)]Table 3. Comparison of relevant test indicators by gender [
$ \bar x \pm s$ /M(P25,P75)]相关指标 性别 t /U P 男性 (n = 581) 女性 (n = 523) Hb(g/L) — TP(g/L) 66.76 ± 7.457 65.80 ± 7.646 2.173 0.030* Alb(g/L) 37.10 ± 5.410 37.11 ± 5.313 0.014 0.989 Glob(g/L) 28.22 ± 5.779 28.04 ± 5.345 0.569 0.569 PA(mmol/L) 223.1 ± 68.67 222.5 ± 71.89 0.138 0.890 TC(mmol/L) 4.054 ± 0.9732 4.332 ± 0.9711 4.884 < 0.001* TG(mmol/L) 1.09(0.830,1.520) 1.04(0.770,1.430) 157520 0.035* HDL(mmol/L) 1.02(0.830,1.210) 1.02(0.840,1.230) 152054 0.999 LDL(mmol/L) 2.60(2.120,3.173) 2.65(2.160,3.160) 150805 0.812 CD3+T (个/μL) 1049 ± 458.4 1124 ± 451.4 555100 < 0.001* CD4+ T(个/μL) 602.2 ± 280.1 655.5 ± 276.2 544894 < 0.001* CD8+T (个/μL) 422.7 ± 230.2 435.8 ± 204.1 577473 0.005* CD4+/CD8+ 1.638 ± 0.790 1.65 ± 0.698 599054 0.163 CD19+B (个/μL) 226.5 ± 171.8 210.1 ± 144.4 138840 0.428 NK (个/μL) 210.1 ± 149.9 204.1 ± 135.2 140958 0.709 NKT (个/μL) 78.00(45.00,129.0) 70.0(43.00,112.0) 134182 0.046* IL-1β (pg/mL) 3.64(1.460,7.150) 4.17(1.623,7.835) 351233 0.026* IL-4 (pg/mL) 1.24(1.010,1.715) 1.31(1.035,1.870) 374319 0.011* IL-8 (pg/mL) 1.76(1.230,4.615) 1.92(1.243,5.015) 377760 0.381 IL-10 (pg/mL) 1.18(0.840,1.680) 1.28(0.900,1.780) 368229 0.003* IL-12p70(pg/mL) 1.42(1.080,1.880) 1.56(1.190,2.098) 354128 < 0.001* IL-17 (pg/mL) 2.30(1.470,4.510) 2.18(1.520,4.520) 138157 0.593 IFN-γ (pg/mL) 3.45(2.200,8.660) 3.84(2.380,9.090) 382754 0.225 经t检验和曼惠特尼U检验,*P < 0.05。 表 4 不同年龄段相关检测指标比较 [
$ \bar x \pm s$ /M(P25,P75)]Table 4. Comparison of relevant test indicators in different age groups [
$ \bar x \pm s$ /M(P25,P75)]相关指标 年龄组 (岁) ≤20 (n = 129) 21~40 (n = 426) 41~60 (n = 311) ≥61 (n = 175) F/H P Hb(g/L) 118.9 ± 19.56 117.9 ± 21.31 125.3 ± 21.15# 118.5 ± 24.28 8.010 0.046* TP(g/L) 67.17 ± 8.429 65.77 ± 7.325 66.44 ± 7.741 66.68 ± 7.300 1.034 0.376 Alb(g/L) 37.18 ± 4.870 37.07 ± 5.344 37.39 ± 5.423 36.60 ± 5.495 0.556 0.644 Glob(g/L) 28.15 ± 5.276 28.03 ± 5.873 28.06 ± 5.271 28.47 ± 5.541 0.848 0.838 PA(mmol/L) 221.9 ± 78.24 223.7 ± 71.80 223.2 ± 68.94 220.3 ± 65.48 1.743 0.156 TC(mmol/L) 3.70 ± 0.7442 4.13 ± 0.840■ 4.36 ± 1.068■ # 4.23 ± 1.113■ 45.50 < 0.001* TG(mmol/L) 0.89 ± 0.328 1.11 ± 0.650■ 1.41 ± 0.741■ # 1.33 ± 0.661■ # 99.14 < 0.001* HDL(mmol/L) 1.06 ± 0.3176 1.05 ± 0.306 1.04 ± 0.297 1.03 ± 0.298 1.270 0.736 LDL(mmol/L) 2.74 ± 0.900 2.72 ± 0.775 2.66 ± 0.817 2.69 ± 0.817 2.558 0.465 CD3+T (个/μL) 1291 ± 540.6 1166 ± 445.6 1021 ± 420.6■ # 880.8 ± 389.5■ # Δ 161.6 < 0.001* CD4+ T(个/μL) 712.9 ± 314.5 665.3 ± 281.6 606.6 ± 264.8■ # 520.2 ± 240.4■ # Δ 93.99 < 0.001* CD8+T (个/μL) 512.0 ± 238.2 458.4 ± 204.4■ 400.1 ± 215.1■ # 359.8 ± 213.1■ # Δ 135.2 < 0.001* CD4+/CD8+ 1.478 ± 0.470 1.57 ± 0.612 1.74 ± 0.821■ # 1.73 ± 0.9733 24.27 < 0.001* CD19+B (个/μL) 215.4 ± 198.1 209.5 ± 149.5 233.5 ± 159.0 210.1 ± 151.9 5.430 0.143 NK (个/μL) 196.1 ± 143.7 201.7 ± 133.2 218.0 ± 148.2 204.7 ± 154.2 6.459 0.091 NKT (个/μL) 79.50(47.0,108.3) 70.0(42.0,113.0) 78.0(46.0,125.3) 73.0(41.75,137.3) 3.794 0.285 IL-1β (pg/mL) 4.43(1.533,8.098) 4.41(1.790,7.925) 3.76(1.400,7.400) 2.94(1.350,6.185)# 15.97 0.001* IL-4 (pg/mL) 1.28(1.00,1.710) 1.26(1.030,1.793) 1.29(1.020,1.860) 1.25(1.018,1.683) 1.422 0.701 IL-8 (pg/mL) 2.03(1.320,5.253) 1.83(1.228,4.450) 1.84(1.228,4.733) 1.82(1.230,5.330) 2.545 0.467 IL-10 (pg/mL) 1.19(0.860,1.710) 1.23(0.860,1.720) 1.25(0.890,1.690) 1.21(0.870,1.780) 0.180 0.981 IL-12p70(pg/mL) 1.48(1.140,2.020) 1.51(1.155,2.100) 1.48(1.120,1.950) 1.44(1.120,1.850) 3.771 0.287 IL-17 (pg/mL) 2.16(1.520,3.940) 2.13(1.428,4.290) 2.21(1.525,4.388) 2.65(1.540,5.355) 5.747 0.125 IFN-γ (pg/mL) 4.44(2.325,9.41) 3.65(2.318,9.04) 3.11(2.190,8.830) 3.81(2.343,9.29) 4.522 0.210 与≤20岁比较,■P < 0.05;与21~40岁组比较,#P < 0.05;与41~60岁组比较,ΔP < 0.05。*P < 0.05。 -
[1] World Health Organization. Global tuberculosis report 2021 [EB/OL]. [2021-01-20] ( 2021-10-14). https://www.who.int/tb/publications/global_ report/en/2021.10.14. [2] Girardi E,Sane S M,Goletti D,et al. The global dynamics of diabetes and tuberculosis: The impact of migration and policy implications[J]. Int J Infect Dis,2017,3(56):45-53. [3] Sinha P,Davis J,Saag L,et al. Undernutrition and tuberculosis:Public health implications[J]. J Infect Dis,2019,219(9):1356-1363. doi: 10.1093/infdis/jiy675 [4] 冯治宇,谭守勇,章志俊,等. 营养支持对伴营养不良的肺结核并肺部感染者的疗效观察[J]. 临床肺科杂志,2018,23(7):1169-1171. doi: 10.3969/j.issn.1009-6663.2018.07.002 [5] 郭冬生. 营养与免疫关系及其研究进展[J]. 湖南文理学院学报(自然科学版),2021,33(3):24-27. [6] Gombart A F,Pierre A,Maggini S. A review of micronutrients and the immune system-working in harmony to reduce the risk of infection[J]. Nutrients,2020,12(1):236. doi: 10.3390/nu12010236 [7] Marcos A. Editorial: A review of micronutrients and the immune system-working in harmony to reduce the risk of infection[J]. Nutrients,2021,13(11):4180. doi: 10.3390/nu13114180 [8] 周林,刘二勇,孟庆琳,等. 《WS 288-2017肺结核诊断》标准实施后肺结核诊断质量评估分析[J]. 中国防痨杂志,2020,42(9):910-915. doi: 10.3969/j.issn.1000-6621.2020.09.005 [9] 王智慧,董雅坤,池跃朋,等. 河北省老年耐药结核性胸膜炎患者细胞免疫及营养状况[J]. 中国热带医学,2021,21(10):943-947. doi: 10.13604/j.cnki.46-1064/r.2021.10.06 [10] 叶涛生,韦彩岭,张明霞,等. 活动性肺结核患者支气管肺泡灌洗液免疫细胞分析[J]. 中国热带医学,2019,19(7):610-614. doi: 10.13604/j.cnki.46-1064/r.2019.07.03 [11] Chuang Y,He L,Pinn M L,et al. Albumin fusion with granulocyte-macrophage colony-stimulating factor acts as an immunotherapy against chronic tuberculosis[J]. Cellular & Molecular Immunology,2021,18(10):2393-2401. [12] 吕和,王政,王婷,等. 非活动性肺结核并发慢性阻塞性肺疾病患者营养状况及营养风险分析[J]. 中国防痨杂志,2020,42(12):1310-1312. doi: 10.3969/j.issn.1000-6621.2020.12.011 [13] 柯学,李国保,沈生荣. 结核病的营养治疗[J]. 中华结核和呼吸杂志,2020,43(1):8-10. doi: 10.3760/cma.j.issn.1001-0939.2020.01.003 [14] Kalscheuer R,Palacios A,Anos I,et al. The mycobacterium tuberculosis capsule: A cell structure with key implications in pathogenesis[J]. Biochem J,2019,476(14):1995-2016. doi: 10.1042/BCJ20190324 [15] Urazova O I,Churina E G,Hasanova R R,et al. Association between polymorphisms of cytokine genes and secretion of IL-12p70,IL-18,and IL-27 by dendritic cells in patients with pulmonary tuberculosis[J]. Tuberculosis (Edinb),2019,3(115):56-62. [16] 翟云霞,胥萍,赵静,等. 结核患者外周血25-羟基维生素D的表达与免疫细胞亚群相关性[J]. 中国热带医学,2020,20(11):1053-1056. [17] Pooja Pandey,Anuj Kumar Bhatnagar,Anant Mohan,et al. Insights in tuberculosis immunology: Role of NKT and T regulatory cells[J]. Int J Mycobacteriol,2019,8(4):333-340. doi: 10.4103/ijmy.ijmy_141_19 [18] Takahashi T,Iwasaki A. Sex differences in immune responses[J]. Science,2021,371(6527):347-348. doi: 10.1126/science.abe7199 [19] Maggini S,Pierre A,Calder P C. Immune function and micronutrient requirements change over the life course[J]. Nutrients,2018,10(10):1-30. -






 下载:
下载: